The Antipyretic Efficacy and Safety of Propacetamol Compared With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmaceutical Powder Compressibility – a Science-Based Approach
Pharmaceutical powder compressibility – a science-based approach Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Nicolaos D.Gentis aus Egrigoros (Chios) Griechenland Oberkulm (AG) Schweiz Basel, 2012 Approval Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger und PD Dr. Gabriele Betz und Prof. Dr. Thierry F. Vandamme Basel, den 21. Februar 2012 Prof. Dr. Martin Spiess Dekan 2 Dedicated to my parents with love, appreciation and respect 3 Σωκράτης ―I know one thing, that I know nothing‖ Socrates c. 469 BC – 399 BC 4 Acknowledgements The work for this PhD thesis was carried out in the Industrial Pharmacy Lab, Department of Pharmaceutical Sciences, University of Basel and at the facility of Natoli Engineering Inc. in Saint Louis, Missouri (USA). I would like to express my appreciation and sincere gratefulness to PD Dr. Gabriele Betz for giving me the opportunity to do a PhD under her excellent supervision with essential, continuous support, guidance and brilliant, positive motivation. I would like to thank Prof. Dr. Matthias Hamburger for accepting to be my Faculty Responsible and for the support. My appreciation goes also to Prof. Dr. Thierry F. Vandamme for accepting to assume the co-referencing of this PhD thesis. At this point I would like to thank all former Industrial Pharmacy Research Group members for the unique support and for the great, crazy working atmosphere in the laboratory. Especially I would like to thank Mr. Branko Z. Vranic for his great collaboration and support in the research work of project 2 in this thesis. -

A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia
Korean J Pain 2015 July; Vol. 28, No. 3: 203-209 pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2015.28.3.203 | Original Article | A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea Bong Ha Heo, Ji Hun Park, Jung Il Choi, Woong Mo Kim, Hyoung Gon Lee, Soo Young Cho, and Myoung Ha Yoon Background: Ketorolac has been used as a postoperative analgesia in combination with opioids. However, the use of ketorolac may produce serious side effects in vulnerable patients. Propacetamol is known to induce fewer side effects than ketorolac because it mainly affects the central nervous system. We compared the analgesic effects and patient satisfaction levels of each drug when combined with fentanyl patient-controlled analgesia (PCA). Methods: The patients were divided into two groups, each with n = 46. The patients in each group were given 60 mg of ketorolac or 2 g of propacetamol (mixed with fentanyl) for 10 minutes. The patients were then given 180 mg of ketorolac or 8 g of propacetamol (mixed with fentanyl and ramosetron) through PCA. We assessed the visual analogue pain scale (VAS) at the time point immediately before administration (baseline) and at 15, 30, and 60 minutes, and 24 hours after administration. Also, the side effects of each regimen and each patient’s degree of satisfaction were assessed. Results: There was a significant decline in the VAS score in both groups (P < 0.05). However, there were no significant differences in the VAS scores between the groups at each time point. -

The Challenge of Drug-Induced Aseptic Meningitis Revisited
Letters cardioverter-defibrillator generator replacements and upgrade procedures: brospinal fluid (CSF) findings and reviews added to the litera- results from the REPLACE registry. Circulation. 2010;122(16):1553-1561. ture from 1999 to date. Tables have been assembled from 6. Kramer DB, Buxton AE, Zimetbaum PJ. Time for a change: a new approach to information derived from 192 studies (these data are avail- ICD replacement. N Engl J Med. 2012;366(4):291-293. able from the authors on request). The Challenge of Drug-Induced Aseptic Results | Four groups of drugs continue to be associated Meningitis Revisited with DIAM (Table 1): nonsteroidal anti-inflammatory Cases of drug-induced aseptic meningitis (DIAM) are likely drugs (NSAIDs), antibiotics, immunosuppressive- underreported, and only a few reviews of the literature have immunomodulatory (IS-IM), and antiepileptic drugs.1 Prior been performed. We have updated (to February 2014) a pre- exposure to the associated drug was present in 26% to 35% vious review (1999)1 to identify newer agents associated with of cases (Table 1). The interval between exposure and men- DIAM, as well as distinctive new features. ingitis ranged from minutes to 5 months (Table 1). Most patients presented with headache, fever, meningismus, and Methods | Using the MEDLINE database, we searched the lit- mental status changes (Table 2). Underlying systemic disor- erature to February 2014 and included those cases with cere- ders were often present, particularly systemic lupus ery- Table 1. Drugs Involved in Drug-Induced -

Original Article: Isobolographic Antinociception of Nonsteroidal Anti-Inflam- Matory Drugs in Rodent Formalin Orofacial Pain
September 2020. Volume 6. Number 3 Original Article: Isobolographic Antinociception of Nonsteroidal Anti-inflam- matory Drugs in Rodent Formalin Orofacial Pain Viviana Noriega1 , Fernando Sierralta2 , Nicolás Aranda3 , Ramón Sotomayor-Zárate4, Paula Poblete5 , Juan Carlos Prieto1,2 , Hugo F. Miranda3* 1. Department of Cardiovascular, Clinical Hospital, Universidad de Chile, Santiago, Chile. 2. Pharmacology Program, ICBM, Faculty of Medicine, Universidad de Chile, Santiago, Chile. 3. Department of Neuroscience, Faculty of Medicine, Universidad de Chile, Santiago, Chile. 4. Laboratorio de Neuroquímica y Neurofarmacología, Centro de Neurobiología y Fisiopatología Integrativa, Instituto de Fisiología, Facultad de Ciencias, Universidad de Valparaíso. 5. Clínica alemana, Santiago, Chile. * Corresponding Author: Hugo F. Miranda, PhD. Address: Department of Neuroscience, Faculty of Medicine, Universidad de Chile, Santiago, Chile. Phone: +56 (22) 9786237 E-mail: [email protected] A B S T R A C T Background: Diverse studies suggest that non-steroidal anti-inflammatory drugs (NSAIDs) Copyright© 2020, The Authors. induce antinociception through the inhibition of cyclooxygenases. Objectives: This study evaluated the effect of NSAIDs in inducing antinociception either alone or in combination in mice formalin orofacial pain. Methods: Male mice were injected intraperitoneally with dexibuprofen, dexketoprofen, Article info: diclofenac meloxicam, metamizole and piroxicam. Then from a dose-response curve the Received: 21 Oct 2019 ED50 (dose that produce -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine -
Paracetamol Kabi Data Sheet
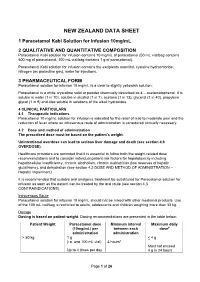
NEW ZEALAND DATA SHEET 1 Paracetamol Kabi Solution for Infusion 10mg/mL 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Paracetamol Kabi solution for infusion contains 10 mg/mL of paracetamol (50 mL vial/bag contains 500 mg of paracetamol, 100 mL vial/bag contains 1 g of paracetamol). Paracetamol Kabi solution for infusion contains the excipients mannitol, cysteine hydrochloride, nitrogen (as protective gas), water for injections. 3 PHARMACEUTICAL FORM Paracetamol solution for infusion 10 mg/mL is a clear to slightly yellowish solution. Paracetamol is a white crystalline solid or powder chemically described as 4 – acetamidophenol. It is soluble in water (1 in 70), soluble in alcohol (1 in 7), acetone (1 in 13), glycerol (1 in 40), propylene glycol (1 in 9) and also soluble in solutions of the alkali hydroxides. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Paracetamol 10 mg/mL solution for infusion is indicated for the relief of mild to moderate pain and the reduction of fever where an intravenous route of administration is considered clinically necessary. 4.2 Dose and method of administration The prescribed dose must be based on the patient’s weight. Unintentional overdose can lead to serious liver damage and death (see section 4.9 OVERDOSE). Healthcare providers are reminded that it is essential to follow both the weight-related dose recommendations and to consider individual patient risk factors for hepatotoxicity including hepatocellular insufficiency, chronic alcoholism, chronic malnutrition (low reserves of hepatic glutathione), and dehydration (see section 4.2 DOSE AND METHOD OF ADMINISTRATION – Hepatic Impairment). It is recommended that suitable oral analgesic treatment be substituted for Paracetamol solution for infusion as soon as the patient can be treated by the oral route (see section 4.3 CONTRAINDICATIONS). -

(8) No. 1 March 2005 Alexandria Journal of Anaesthesia and Intensive Care 50
Alexandria Journal of Anaesthesia and Intensive Care 49 Propacetamol Versus Placebo for Management of Acute Postoperative Pain After Elective Tonsillectomy in Children. Mahmoud A Nassef, MD*. Ashraf M Moustafa, MD**. Ashraf A Moussa, MD***. *Department of Anesthesia, Beni-Suef Faculty of Medicine, Cairo University **Department of Anesthesia, Menoufiya University ***Department of Anesthesia,Menoufiya Liver Institute, Menoufiya University ABSTRACT The analgesic efficacy and safety of propacetamol, an injectable prodrug of acetaminophen, was assessed versus placebo after elective tonsillectomy operation in children. Using a double-blind, randomized parallel group design, 70 children aged 6-12 years were included to evaluate the effect of a single iv infusion of 40 mg/kg propacetamol versus a single infusion of 100 ml normal saline ( placebo ) given at the recovery room. Analgesic efficacy was assessed on pain scores rated on a four-points verbal scale, a five-points visual scale ( faces ) and a four-points pain relief verbal scale; before administration ( T0 ) and 0.25, 0.5, 1, 2, 3, 4, 5 and 6 hours after the infusion. The global efficacy was rated on a five-point scale at the end of the study. Rescue medication was allowed freely and the time for re-medication as well as the occurrence of any side effects was recorded. Propacetamol was statistically superior to placebo on all assessment criteria. The global final efficacy evaluation demonstrated 12 patients in the propacetamol group with good and very good scores compared to only one patient in the placebo group. Rescue medication was used in 40% of patients in the propacetamol group versus 83% in the placebo group. -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine. -

Inflammatory Drugs
Solubility of Nonsteroidal Anti- diflunisal, etoricoxib, fenbufen, fentiazac, flufenamic inflammatory Drugs (NSAIDs) in acid, flurbiprofen, ibuprofen, indomethacin, ketopro- Neat Organic Solvents and Organic fen, ketorolac, lornoxicam, mefenamic acid, melox- Solvent Mixtures iam, nabumetone, naproxen, niflumic acid, nimesulide, phenylbutazone, piroxicam, rofecoxib, sodium diclof- William E. Acree enac, sodium ibuprofen, sodium naproxen, sodium J. Phys. Chem. Ref. Data 43, 023102 (2014) salicylate, tenoxicam, tolfenamic acid, and valdecoxib. IUPAC-NIST Solubility Data Series, Volume 102 http://dx.doi.org/10.1063/1.4869683 This IUPAC-NIST Solubility Data Series volume reviews experimentally determined solubility data for 33 non- To access recent volumes in the Solubility Data Series, visit http://jpcrd.aip.org/ and steroidal anti-inflammatory drugs (NSAIDs) dissolved search IUPAC-NIST Solubility Data Series in neat organic solvents and well-defined binary and ternary organic solvent mixtures retrieved from the published chemical and pharmaceutical litera- ture covering the period from 1980 to the beginning of 2014. Except for aspirin (2-acetoxybenzoic acid) and salicylic acid (2-hydroxybenzoic acid), very little Provisional Recommendations physical and chemical property data are available Provisional Recommendations are drafts of IUPAC in the published literature for NSAIDs prior to 1980. recommendations on terminology, nomenclature, and Solubility data are compiled and critically reviewed symbols made widely available to allow interested -

Manufacturing of Quick Release Pharmaceutical
(19) TZZ___T (11) EP 1 916 994 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/00 (2006.01) A61K 9/20 (2006.01) 11.12.2013 Bulletin 2013/50 A61K 31/542 (2006.01) (21) Application number: 05753592.4 (86) International application number: PCT/DK2005/000435 (22) Date of filing: 28.06.2005 (87) International publication number: WO 2006/000228 (05.01.2006 Gazette 2006/01) (54) MANUFACTURING OF QUICK RELEASE PHARMACEUTICAL COMPOSITION OF WATER INSOLUBLE DRUGS AND PHARMACEUTICAL COMPOSITIONS OBTAINED BY THE PROCESS OF THE INVENTION HERSTELLUNG EINER PHARMAZEUTISCHEN ZUSAMMENSETZUNG MIT SCHNELLER FREISETZUNG AUS WASSERUNLÖSLICHEN ARZNEIMITTELN UND MIT DEM ERFINDUNGSGEMÄSSEN VERFAHREN ERHALTENE PHARMAZEUTISCHE ZUSAMMENSETZUNGEN PREPARATION DE COMPOSITIONS PHARMACEUTIQUES DE MEDICAMENTS INSOLUBLES A L’EAU A DIFFUSION RAPIDE ET COMPOSITIONS PHARMACEUTIQUES AINSI PREPAREES (84) Designated Contracting States: (56) References cited: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR EP-A- 1 352 660 WO-A-00/15195 HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR WO-A-01/41536 WO-A-99/09988 Designated Extension States: WO-A-99/12524 WO-A1-2004/047824 AL BA HR LV MK YU US-A- 4 689 218 (30) Priority: 29.06.2004 DK 200401021 • MURA P ET AL: "Solid- state characterization and dissolution properties of Naproxen-Arginine- (43) Date of publication of application: Hydroxypropyl-beta-cyclo dextrin ternary 07.05.2008 Bulletin 2008/19 system" EUROPEAN JOURNAL OF PHARMACEUTICS AND BIOPHARMACEUTICS, (73) Proprietor: Takeda Pharma A/S ELSEVIER SCIENCE PUBLISHERS B.V., 4000 Roskilde (DK) AMSTERDAM, NL, vol. -

Inflammatory Drugs (Nsaids) for People with Or at Risk of COVID-19
Evidence review Acute use of non-steroidal anti- inflammatory drugs (NSAIDs) for people with or at risk of COVID-19 Publication date: April 2020 This evidence review sets out the best available evidence on acute use of non- steroidal anti-inflammatory drugs (NSAIDs) for people with or at risk of COVID-19. It should be read in conjunction with the evidence summary, which gives the key messages. Evidence review commissioned by NHS England Disclaimer The content of this evidence review was up-to-date on 24 March 2020. See summaries of product characteristics (SPCs), British national formulary (BNF) or the MHRA or NICE websites for up-to-date information. For details on the date the searches for evidence were conducted see the search strategy. Copyright © NICE 2020. All rights reserved. Subject to Notice of rights. ISBN: 978-1-4731-3763-9 Contents Contents ...................................................................................................... 1 Background ................................................................................................. 2 Intervention .................................................................................................. 2 Clinical problem ........................................................................................... 3 Objective ...................................................................................................... 3 Methodology ................................................................................................ 4 Summary of included studies -

022450Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 022450Orig1s000 PHARMACOLOGY REVIEW(S) 5 Page(s) of Draft Labeling have been Withheld in Full as b4 (CCI/TS) immediately following this page (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) Pharmacology Toxicology Review Addendum Executive Summary I. Recommendations A. Recommendation on approvability From the nonclinical pharmacology perspective, NDA 22-450 is recommended for approval. B. Recommendation for nonclinical studies At this time, there are no nonclinical studies needed that will impact approvability. C. Recommendation on labeling The table below contains the draft labeling submitted by the sponsor, the proposed changes and the rationale for the proposed changes for the nonclinical toxicology section only. Please see the secondary review for final labeling recommendations. (b) (4) 1 Reviewer: Carlic K. Huynh, Ph.D. NDA No. 22-450 (b) (4) II. Summary of nonclinical findings A. Brief overview of nonclinical findings From the previous pharmacology toxicology review of this NDA, acetaminophen is not a mutagen (as demonstrated by negative results in the bacterial Ames test) but is a clastogen (as demonstrated by positive results in the chromosomal aberration assay in cultured human peripheral blood lymphocytes).