ASDERA – Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmaceutical Powder Compressibility – a Science-Based Approach
Pharmaceutical powder compressibility – a science-based approach Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Nicolaos D.Gentis aus Egrigoros (Chios) Griechenland Oberkulm (AG) Schweiz Basel, 2012 Approval Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger und PD Dr. Gabriele Betz und Prof. Dr. Thierry F. Vandamme Basel, den 21. Februar 2012 Prof. Dr. Martin Spiess Dekan 2 Dedicated to my parents with love, appreciation and respect 3 Σωκράτης ―I know one thing, that I know nothing‖ Socrates c. 469 BC – 399 BC 4 Acknowledgements The work for this PhD thesis was carried out in the Industrial Pharmacy Lab, Department of Pharmaceutical Sciences, University of Basel and at the facility of Natoli Engineering Inc. in Saint Louis, Missouri (USA). I would like to express my appreciation and sincere gratefulness to PD Dr. Gabriele Betz for giving me the opportunity to do a PhD under her excellent supervision with essential, continuous support, guidance and brilliant, positive motivation. I would like to thank Prof. Dr. Matthias Hamburger for accepting to be my Faculty Responsible and for the support. My appreciation goes also to Prof. Dr. Thierry F. Vandamme for accepting to assume the co-referencing of this PhD thesis. At this point I would like to thank all former Industrial Pharmacy Research Group members for the unique support and for the great, crazy working atmosphere in the laboratory. Especially I would like to thank Mr. Branko Z. Vranic for his great collaboration and support in the research work of project 2 in this thesis. -

Development of Pain-Free Methods for Analyzing 231 Multiclass Drugs and Metabolites by LC-MS/MS
Clinical, Forensic & Toxicology Article “The Big Pain”: Development of Pain-Free Methods for Analyzing 231 Multiclass Drugs and Metabolites by LC-MS/MS By Sharon Lupo As the use of prescription and nonprescription drugs grows, the need for fast, accurate, and comprehensive methods is also rapidly increasing. Historically, drug testing has focused on forensic applications such as cause of death determinations or the detection of drug use in specific populations (military, workplace, probation/parole, sports doping). However, modern drug testing has expanded well into the clinical arena with a growing list of target analytes and testing purposes. Clinicians often request the analysis of large panels of drugs and metabolites that can be used to ensure compliance with prescribed pain medication regimens and to detect abuse or diversion of medications. With prescription drug abuse reaching epidemic levels [1], demand is growing for analytical methods that can ensure accurate results for comprehensive drug lists with reasonable analysis times. LC-MS/MS is an excellent technique for this work because it offers greater sensitivity and specificity than immunoassay and—with a highly selective and retentive Raptor™ Biphenyl column—can provide definitive results for a wide range of compounds. Typically, forensic and pain management drug testing consists of an initial screening analysis, which is qualitative, quick, and requires only minimal sample preparation. Samples that test positive during screening are then subjected to a quantitative confirmatory analysis. Whereas screening assays may cover a broad list of compounds and are generally less sensitive and specific, confirmation testing provides fast, targeted analysis using chromatographic conditions that are optimized for specific panels. -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -

PR2 2009.Vp:Corelventura
Pharmacological Reports Copyright © 2009 2009, 61, 197216 by Institute of Pharmacology ISSN 1734-1140 Polish Academy of Sciences Review Third-generation antiepileptic drugs: mechanisms of action, pharmacokinetics and interactions Jarogniew J. £uszczki1,2 Department of Pathophysiology, Medical University of Lublin, Jaczewskiego 8, PL 20-090 Lublin, Poland Department of Physiopathology, Institute of Agricultural Medicine, Jaczewskiego 2, PL 20-950 Lublin, Poland Correspondence: Jarogniew J. £uszczki, e-mail: [email protected]; [email protected] Abstract: This review briefly summarizes the information on the molecular mechanisms of action, pharmacokinetic profiles and drug interac- tions of novel (third-generation) antiepileptic drugs, including brivaracetam, carabersat, carisbamate, DP-valproic acid, eslicar- bazepine, fluorofelbamate, fosphenytoin, ganaxolone, lacosamide, losigamone, pregabalin, remacemide, retigabine, rufinamide, safinamide, seletracetam, soretolide, stiripentol, talampanel, and valrocemide. These novel antiepileptic drugs undergo intensive clinical investigations to assess their efficacy and usefulness in the treatment of patients with refractory epilepsy. Key words: antiepileptic drugs, brivaracetam, carabersat, carisbamate, DP-valproic acid, drug interactions, eslicarbazepine, fluorofelbamate, fosphenytoin, ganaxolone, lacosamide, losigamone, pharmacokinetics, pregabalin, remacemide, retigabine, rufinamide, safinamide, seletracetam, soretolide, stiripentol, talampanel, valrocemide Abbreviations: 4-AP -

A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia
Korean J Pain 2015 July; Vol. 28, No. 3: 203-209 pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2015.28.3.203 | Original Article | A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea Bong Ha Heo, Ji Hun Park, Jung Il Choi, Woong Mo Kim, Hyoung Gon Lee, Soo Young Cho, and Myoung Ha Yoon Background: Ketorolac has been used as a postoperative analgesia in combination with opioids. However, the use of ketorolac may produce serious side effects in vulnerable patients. Propacetamol is known to induce fewer side effects than ketorolac because it mainly affects the central nervous system. We compared the analgesic effects and patient satisfaction levels of each drug when combined with fentanyl patient-controlled analgesia (PCA). Methods: The patients were divided into two groups, each with n = 46. The patients in each group were given 60 mg of ketorolac or 2 g of propacetamol (mixed with fentanyl) for 10 minutes. The patients were then given 180 mg of ketorolac or 8 g of propacetamol (mixed with fentanyl and ramosetron) through PCA. We assessed the visual analogue pain scale (VAS) at the time point immediately before administration (baseline) and at 15, 30, and 60 minutes, and 24 hours after administration. Also, the side effects of each regimen and each patient’s degree of satisfaction were assessed. Results: There was a significant decline in the VAS score in both groups (P < 0.05). However, there were no significant differences in the VAS scores between the groups at each time point. -

Identification of Channels Underlying the M-Like Potassium Current In
Identification of channeis underiying the M-like potassium current in NG108-15 neurobiastoma-giioma ceiis A thesis submitted for the degree of Doctor of Philosophy University of London by Jennifer Kathleen Hadley Department of Pharmacology University College London Gower Street London WC1E 6BT ProQuest Number: U644085 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest U644085 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 Abstract NG108-15 cells express a potassium current resembling the IVI-current found in sympathetic ganglia. I contributed to the identification of the channels underlying this NG108-15 current. I used patch-clamp methodology to characterise the kinetics and pharmacology of the M-like current and of three candidate channel genes, all capable of producing “delayed rectifier” currents, expressed in mammalian cells. I studied two Kvi .2 clones: NGK1 (rat Kvi .2) expressed in mouse fibroblasts, and MK2 (mouse brain Kvi .2) expressed in Chinese hamster ovary (OHO) cells. Kvi.2 showed relatively positive activation that shifted negatively on repeated activation, some inactivation, block by dendrotoxin and various cations, and activation by niflumic acid. -
Paracetamol Kabi Data Sheet
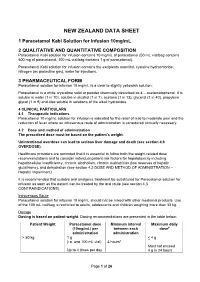
NEW ZEALAND DATA SHEET 1 Paracetamol Kabi Solution for Infusion 10mg/mL 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Paracetamol Kabi solution for infusion contains 10 mg/mL of paracetamol (50 mL vial/bag contains 500 mg of paracetamol, 100 mL vial/bag contains 1 g of paracetamol). Paracetamol Kabi solution for infusion contains the excipients mannitol, cysteine hydrochloride, nitrogen (as protective gas), water for injections. 3 PHARMACEUTICAL FORM Paracetamol solution for infusion 10 mg/mL is a clear to slightly yellowish solution. Paracetamol is a white crystalline solid or powder chemically described as 4 – acetamidophenol. It is soluble in water (1 in 70), soluble in alcohol (1 in 7), acetone (1 in 13), glycerol (1 in 40), propylene glycol (1 in 9) and also soluble in solutions of the alkali hydroxides. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Paracetamol 10 mg/mL solution for infusion is indicated for the relief of mild to moderate pain and the reduction of fever where an intravenous route of administration is considered clinically necessary. 4.2 Dose and method of administration The prescribed dose must be based on the patient’s weight. Unintentional overdose can lead to serious liver damage and death (see section 4.9 OVERDOSE). Healthcare providers are reminded that it is essential to follow both the weight-related dose recommendations and to consider individual patient risk factors for hepatotoxicity including hepatocellular insufficiency, chronic alcoholism, chronic malnutrition (low reserves of hepatic glutathione), and dehydration (see section 4.2 DOSE AND METHOD OF ADMINISTRATION – Hepatic Impairment). It is recommended that suitable oral analgesic treatment be substituted for Paracetamol solution for infusion as soon as the patient can be treated by the oral route (see section 4.3 CONTRAINDICATIONS). -

(8) No. 1 March 2005 Alexandria Journal of Anaesthesia and Intensive Care 50
Alexandria Journal of Anaesthesia and Intensive Care 49 Propacetamol Versus Placebo for Management of Acute Postoperative Pain After Elective Tonsillectomy in Children. Mahmoud A Nassef, MD*. Ashraf M Moustafa, MD**. Ashraf A Moussa, MD***. *Department of Anesthesia, Beni-Suef Faculty of Medicine, Cairo University **Department of Anesthesia, Menoufiya University ***Department of Anesthesia,Menoufiya Liver Institute, Menoufiya University ABSTRACT The analgesic efficacy and safety of propacetamol, an injectable prodrug of acetaminophen, was assessed versus placebo after elective tonsillectomy operation in children. Using a double-blind, randomized parallel group design, 70 children aged 6-12 years were included to evaluate the effect of a single iv infusion of 40 mg/kg propacetamol versus a single infusion of 100 ml normal saline ( placebo ) given at the recovery room. Analgesic efficacy was assessed on pain scores rated on a four-points verbal scale, a five-points visual scale ( faces ) and a four-points pain relief verbal scale; before administration ( T0 ) and 0.25, 0.5, 1, 2, 3, 4, 5 and 6 hours after the infusion. The global efficacy was rated on a five-point scale at the end of the study. Rescue medication was allowed freely and the time for re-medication as well as the occurrence of any side effects was recorded. Propacetamol was statistically superior to placebo on all assessment criteria. The global final efficacy evaluation demonstrated 12 patients in the propacetamol group with good and very good scores compared to only one patient in the placebo group. Rescue medication was used in 40% of patients in the propacetamol group versus 83% in the placebo group. -

KCNQ5 Antibody
Product Datasheet KCNQ5 Antibody Catalog No: #34920 Package Size: #34920-1 50ul #34920-2 100ul Orders: [email protected] Support: [email protected] Description Product Name KCNQ5 Antibody Host Species Rabbit Clonality Polyclonal Purification The antibody was affinity-purified from rabbit antiserum by affinity-chromatography using epitope-specific immunogen. Applications WB Species Reactivity Hu Specificity The antibody detects endogenous levels of total KCNQ5 protein. Immunogen Type Peptide Immunogen Description Synthesized peptide derived from internal of human KCNQ5. Target Name KCNQ5 Other Names Potassium voltage-gated channel subfamily KQT member 5; Voltage-gated potassium channel subunit Kv7.5; Potassium channel subunit alpha KvLQT5; KQT-like 5; Accession No. Swiss-Prot: Q9NR82NCBI Gene ID: 56479 SDS-PAGE MW 100kd Concentration 1.0mg/ml Formulation Rabbit IgG in phosphate buffered saline (without Mg2+ and Ca2+), pH 7.4, 150mM NaCl, 0.02% sodium azide and 50% glycerol. Storage Store at -20°C Application Details Western blotting: 1:500~1:3000 Images Western blot analysis of extracts from Jurkat cells, using KCNQ5 antibody #34920. Address: 8400 Baltimore Ave., Suite 302, College Park, MD 20740, USA http://www.sabbiotech.com 1 Background Probably important in the regulation of neuronal excitability. Associates with KCNQ3 to form a potassium channel which contributes to M-type current, a slowly activating and deactivating potassium conductance which plays a critical role in determining the subthreshold electrical excitability of neurons. May contribute, with other potassium channels, to the molecular diversity of a heterogeneous population of M-channels, varying in kinetic and pharmacological properties, which underlie this physiologically important current. Insensitive to tetraethylammonium, but inhibited by barium, linopirdine and XE991. -

Progress Report on New Antiepileptic Drugs
Epilepsy Research (2013) 103, 2—30 j ournal homepage: www.elsevier.com/locate/epilepsyres REVIEW Progress report on new antiepileptic drugs: A summary of the Eleventh Eilat Conference (EILAT XI) a,∗ b c d Meir Bialer , Svein I. Johannessen , René H. Levy , Emilio Perucca , e f Torbjörn Tomson ,H. Steve White a Institute for Drug Research, School of Pharmacy and David R. Bloom Center for Pharmacy, Faculty of Medicine, Ein Karem, The Hebrew University of Jerusalem, 91120 Jerusalem, Israel b The National Center for Epilepsy, Sandvika, and Department of Pharmacology, Oslo University Hospital, Oslo, Norway c Department of Pharmaceutics and Neurological Surgery, University of Washington, Seattle, Washington, WA, USA d Clinical Pharmacology Unit, Department of Internal Medicine and Therapeutics, University of Pavia, and National Institute of Neurology IRCCS C. Mondino Foundation, Pavia, Italy e Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden f Department of Pharmacology and Toxicology, University of Utah, Salt Lake City, UT, USA Received 13 September 2012; accepted 8 October 2012 Available online 4 December 2012 KEYWORDS Summary The Eleventh Eilat Conference on New Antiepileptic Drugs (AEDs)-EILAT XI, took place in Eilat, Israel from the 6th to 10th of May 2012. About 100 basic scientists, clinical phar- Antiepileptic drugs; macologists and neurologists from 20 countries attended the conference, whose main themes Drug development; Epilepsy; included ‘‘Indications overlapping with epilepsy’’ and ‘‘Securing the successful development Pharmacology; of an investigational antiepileptic drug in the current environment’’. Consistent with previ- ous formats of this conference, a large part of the program was devoted to a review of AEDs Clinical trials; Conference in development, as well as updates on AEDs introduced since 1994.