CD5-Positive Acute Lymphoblastic Leukemia Dawood Ahmed1, Tahir Aziz Ahmed1, Suhaib Ahmed 2, Hamid Nawaz Tipu1 and Muhammad Amin Wiqar1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Lymphoma and Multiple Myeloma Center
The Lymphoma and Multiple Myeloma Center What Sets Us Apart We provide multidisciplinary • Experienced, nationally and internationally recognized physicians dedicated exclusively to treating patients with lymphoid treatment for optimal survival or plasma cell malignancies and quality of life for patients • Cellular therapies such as Chimeric Antigen T-Cell (CAR T) therapy for relapsed/refractory disease with all types and stages of • Specialized diagnostic laboratories—flow cytometry, cytogenetics, and molecular diagnostic facilities—focusing on the latest testing lymphoma, chronic lymphocytic that identifies patients with high-risk lymphoid malignancies or plasma cell dyscrasias, which require more aggresive treatment leukemia, multiple myeloma and • Novel targeted therapies or intensified regimens based on the other plasma cell disorders. cancer’s genetic and molecular profile • Transplant & Cellular Therapy program ranked among the top 10% nationally in patient outcomes for allogeneic transplant • Clinical trials that offer tomorrow’s treatments today www.roswellpark.org/partners-in-practice Partners In Practice medical information for physicians by physicians We want to give every patient their very best chance for cure, and that means choosing Roswell Park Pathology—Taking the best and Diagnosis to a New Level “ optimal front-line Lymphoma and myeloma are a diverse and heterogeneous group of treatment.” malignancies. Lymphoid malignancy classification currently includes nearly 60 different variants, each with distinct pathophysiology, clinical behavior, response to treatment and prognosis. Our diagnostic approach in hematopathology includes the comprehensive examination of lymph node, bone marrow, blood and other extranodal and extramedullary tissue samples, and integrates clinical and diagnostic information, using a complex array of diagnostics from the following support laboratories: • Bone marrow laboratory — Francisco J. -

Low-Grade Non-Hodgkin Lymphoma Book
Low-grade non-Hodgkin lymphoma Low-grade non-Hodgkin lymphoma Follicular lymphoma Mantle cell lymphoma Marginal zone lymphomas Lymphoplasmacytic lymphoma Waldenström’s macroglobulinaemia This book has been researched and written for you by Lymphoma Action, the only UK charity dedicated to people affected by lymphoma. We could not continue to support you, your clinical team and the wider lymphoma community, without the generous donations of our incredible supporters. As an organisation we do not receive any government or NHS funding and so every penny received is truly valued. To make a donation towards our work, please visit lymphoma-action.org.uk/Donate 2 Your lymphoma type and stage Your treatment Key contact Name: Role: Contact details: Job title/role Name and contact details GP Consultant haematologist/ oncologist Clinical nurse specialist or key worker Treatment centre 3 About this book Low-grade (or indolent) non-Hodgkin lymphoma is a type of blood cancer that develops from white blood cells called lymphocytes. It is a broad term that includes lots of different types of lymphoma. This book explains what low-grade non-Hodgkin lymphoma is and how it is diagnosed and treated. It includes tips on coping with treatment and dealing with day-to-day life. The book is split into chapters. You can dip in and out of it and read the sections that are relevant to you at any given time. Important and summary points are written in the chapter colour. Lists practical tips and chapter summaries. Gives space for questions and notes. Lists other resources you might find useful, some of which are online. -

And Heterodimeric Interactions Between the Gene Products of PKD1 and PKD2 (Polycystic Kidney Disease͞yeast Two-Hybrid System͞protein–Protein Interactions)
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 6965–6970, June 1997 Medical Sciences Homo- and heterodimeric interactions between the gene products of PKD1 and PKD2 (polycystic kidney diseaseyyeast two-hybrid systemyprotein–protein interactions) LEONIDAS TSIOKAS*†,EMILY KIM†‡,THIERRY ARNOULD*, VIKAS P. SUKHATME*, AND GERD WALZ*§ *Renal Division, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02215; and ‡Laboratory of Molecular and Developmental Neuroscience, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114 Communicated by Irving M. London, Massachusetts Institute of Technology, Cambridge, MA, May 1, 1997 (received for review January 3, 1997) ABSTRACT PKD1 and PKD2 are two recently identified clarified the nature of the aberrant gene products caused by genes that are responsible for the vast majority of autosomal mutations of PKD1 and PKD2. Renal cysts are thought to arise polycystic kidney disease, a common inherited disease that through a process of persistent epithelial proliferation related causes progressive renal failure. PKD1 encodes polycystin, a to the lack of terminal differentiation. Both abnormal growth large glycoprotein that contains several extracellular motifs factor responsiveness (8–12) and the elevated expression of indicative of a role in cell–cell or cell–matrix interactions, and certain oncogenes appear to support this hypothesis (13–16). the PKD2 encodes a protein with homology to a voltage- Recently, loss of heterozygosity was discovered within a subset activated calcium channel and to PKD1. It is currently un- of cysts for two closely linked polymorphic markers located known how mutations of either protein functionally cause within the PKD1 gene, indicating that cyst formation in autosomal polycystic kidney disease. -

Papers J Clin Pathol: First Published As 10.1136/Jcp.49.7.539 on 1 July 1996
Clin Pathol 1996;49:539-544 539 Papers J Clin Pathol: first published as 10.1136/jcp.49.7.539 on 1 July 1996. Downloaded from Differential expression of T cell antigens in normal peripheral blood lymphocytes: a quantitative analysis by flow cytometry L Ginaldi, N Farahat, E Matutes, M De Martinis, R Morilla, D Catovsky Abstract diagnosis by comparison with findings in Aims-To obtain reference values of the normal counterparts. level of expression of T cell antigens on ( Clin Pathol 1996;49:539-544) normal lymphocyte subsets in order to disclose differences which could reflect Keywords: flow cytometry, T cell antigens, peripheral their function or maturation stages, or blood lymphocytes. both. Methods-Peripheral blood from 15 healthy donors was processed by flow The most common use of flow cytometry is to cytometry with triple colour analysis. For determine the percent of "positive" or "nega- each sample phycoerythrin (PE) conju- tive" cells for each antigen in different cell gated CD2, CD4, CD5, CD8, and CD56 populations. However, valuable information is monoclonal antibodies were combined lost when the relative intensities of the positive with Cy5-R-phycoerythrin (TC) conju- cells, reflecting antigenic densities, are not considered. A cell population with a well gated CD3 and fluorescein isothiocyanate http://jcp.bmj.com/ (FITC) conjugated CD7; CD2- and defined phenotype, positive for one antigen, CD7-PE were also combined with might be heterogeneous with regard to its level CD3-TC and CD4-FITC. Standard mi- of expression. This may reflect different crobeads with different capacities to bind functional or maturational states, or both, or mouse immunoglobulins were used to identify subpopulations on the basis of the dif- convert the mean fluorescence intensity ferent numbers of molecules of antigen per cell. -

Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy
cancers Review Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy Miriam Marangon 1, Carlo Visco 2 , Anna Maria Barbui 3, Annalisa Chiappella 4, Alberto Fabbri 5, Simone Ferrero 6,7 , Sara Galimberti 8 , Stefano Luminari 9,10 , Gerardo Musuraca 11, Alessandro Re 12 , Vittorio Ruggero Zilioli 13 and Marco Ladetto 14,15,* 1 Department of Hematology, Azienda Sanitaria Universitaria Giuliano Isontina, 34129 Trieste, Italy; [email protected] 2 Section of Hematology, Department of Medicine, University of Verona, 37134 Verona, Italy; [email protected] 3 Hematology Unit, ASST Papa Giovanni XXIII, 24127 Bergamo, Italy; [email protected] 4 Division of Hematology, Fondazione IRCCS, Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] 5 Hematology Division, Department of Oncology, Azienda Ospedaliero-Universitaria Senese, 53100 Siena, Italy; [email protected] 6 Hematology Division, Department of Molecular Biotechnologies and Health Sciences, Università di Torino, 10126 Torino, Italy; [email protected] 7 Hematology 1, AOU Città della Salute e della Scienza di Torino, 10126 Torino, Italy 8 Hematology Unit, Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy; [email protected] 9 Hematology Unit, Azienda Unità Sanitaria Locale IRCCS di Reggio Emilia, 42123 Modena, Italy; [email protected] 10 Surgical, Medical and Dental Department of Morphological Sciences Related -

Stroma-Free, Serum-Free Expansion and Differentiation of Hematopoietic Stem and Progenitor Cells to the T Cell Lineage Nooshin Tabatabaei-Zavareh1, Tim A
Stroma-free, serum-free expansion and differentiation of hematopoietic stem and progenitor cells to the T cell lineage Nooshin Tabatabaei-Zavareh1, Tim A. Le Fevre1, Alexander J.Y. Man1, Evan A. Karas1, Stephen J. Szilvassy1, Terry E. Thomas1 , Allen C. Eaves1,2, and Albertus W. Wognum1 1 STEMCELL Technologies Inc., Vancouver, BC, Canada 2 Terry Fox Laboratory, BC Cancer Agency, Vancouver, BC, Canada Introduction The use of T cells for cancer immunotherapy and other therapeutic applications relies on the isolation of T cells from peripheral blood and their subsequent activation and expansion in culture. T cells can also be generated from hematopoietic stem and/or progenitor cells (HSPCs) in cord blood (CB) or bone marrow (BM). This approach not only offers a renewable source of T cells, but also provides a model system to study disease mechanisms or validate new drugs that affect T cell development and/or function. Differentiation of HSPCs to T cells typically requires co-culture with stromal cell lines that have been engineered to express a Notch-ligand. In such cultures, CD34+CD38-/lo HSPCs develop into CD7+CD5+ pro-T cells that further differentiate to T lineage-committed progenitor cells (pre-T cells) characterized by the expression of CD1a. CD7+CD1a+ pre-T cells can then differentiate to express CD4 and become CD4 immature single-positive (CD4ISP) cells. CD4ISP cells give rise to CD4+CD8+ double positive (DP) cells. These finally mature into CD4 and CD8 single-positive (SP) CD3+TCRαβ+ T cells. Here we describe a serum-free culture method that recapitulates these differentiation steps in the absence of stromal cells and generates large numbers of functional T lineage cells from a limited number of purified CD34+ CB cells. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -
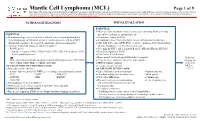
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

Expression of Endothelial Cell-Associated Molecules in AML
Leukemia (2002) 16, 112–119 2002 Nature Publishing Group All rights reserved 0887-6924/02 $25.00 www.nature.com/leu Expression of endothelial cell-associated molecules in AML cells M Watarai1, H Miwa1, M Shikami1, K Sugamura1, M Wakabayashi1, A Satoh1, K Tsuboi1, A Imamura1, H Mihara1, Y Katoh1, K Kita2 and M Nitta1 1Department of Internal Medicine, Division of Hematology, Aichi Medical University School of Medicine, Nagakute, Aichi, Japan; and 2Tokura Hospital, Uji, Kyoto, Japan Recently, it has been clarified that interaction between hemato- hematopoietic cells is also mediated by adhesion molecules poietic cells and endothelial cells is important in normal hema- such as integrins, as well as soluble factors.10,11 topoiesis and leukemogenesis. In this study, we examined the relationship between AML cells and endothelial cells by analyz- Angiopoietins and VEGF are recognized to act coordinately ing the expression profile of angiogenic factors, angiopoietin- during vascular growth and remodeling. Blood vessels remain 1 (Ang-1), Ang-2, Tie-2 (a receptor for angiopoietins) and vascu- in a stable state when Tie-2 receptor is constitutively engaged lar endothelial growth factor (VEGF). Our results demonstrated with angiopoietin-1 (Ang-1) by stabilizing blood vessels -that CD7(؉)AML expressed Ang-2 mRNA frequently and inte- through interactions with perivascular cells and the extracellu grin-family adhesion molecules (CD11c and CD18) intensively, lar matrix. When Ang-2 expression is up-regulated, the inter- suggesting the close correlation with endothelial cells. On the other hand, in t(8;21) AML cells, expression of Ang-2 was action between Tie-2 and Ang-1 is disrupted, and the vessel infrequent and expression of integrin-family adhesion mol- is destabilized. -

Divergent Clonal Evolution of a Common Precursor to Mantle Cell Lymphoma and Classic Hodgkin Lymphoma
Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Divergent clonal evolution of a common precursor to mantle cell lymphoma and classic Hodgkin lymphoma Hammad Tashkandi1, Kseniya Petrova-Drus1, Connie Lee Batlevi2, Maria Arcila1, Mikhail Roshal1, Filiz Sen1, Jinjuan Yao1, Jeeyeon Baik1, Ashley Bilger2, Jessica Singh2, Stephanie de Frank2, Anita Kumar2, Ruth Aryeequaye1, Yanming Zhang1, Ahmet Dogan1, Wenbin Xiao1,* 1Department of Pathology, 2Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY *Correspondence: Wenbin Xiao, MD, PhD Department of Pathology Memorial Sloan Kettering Cancer Center 1275 York Avenue New York, NY 10065 [email protected] Running title: Clonally related mantle cell lymphoma and classic Hodgkin lymphoma Words: 1771 Figures: 2 Tables: 1 Reference: 14 Supplemental materials: Figure S1-S2, Table S1-S4 Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract: Clonal heterogeneity and evolution of mantle cell lymphoma (MCL) remain unclear despite the progress in our understanding of its biology. Here we report a 71 years old male patient with an aggressive MCL and depict the clonal evolution from initial diagnosis of typical MCL to relapsed blastoid MCL. During the course of disease, the patient was diagnosed with Classic Hodgkin lymphoma (CHL), and received CHL therapeutic regimen. Molecular analysis by next generation sequencing of both MCL and CHL demonstrated clonally related CHL with characteristic immunophenotype and PDL1/2 gains. Moreover, our data illustrate the clonal heterogeneity and acquisition of additional genetic aberrations including a rare fusion of SEC22B-NOTCH2 in the process of clonal evolution. -

Multiparameter Phenotype Mapping of Normal and Post-Chemotherapy B
Leukemia (1997) 11, 1266–1273 1997 Stockton Press All rights reserved 0887-6924/97 $12.00 Multiparameter phenotype mapping of normal and post-chemotherapy B lymphopoiesis in pediatric bone marrow MN Dworzak, G Fritsch, C Fleischer, D Printz, G Fro¨schl, P Buchinger, G Mann and H Gadner Children’s Cancer Research Institute, St Anna Kinderspital, Kinderspitalgasse 6, A-1090 Vienna, Austria We studied the differentiation profiles of B cell precursors Materials and methods (BCP) in normal and post-chemotherapy pediatric bone marrow (BM) using multiparameter flow cytometry. The goal of our study was to draw a comprehensive phenotypic map of the Sample description three major maturational BCP stages in BM. By correlating lin- eage-associated markers, CD45RA, and several adhesion mol- Pediatric bone marrow (BM) samples (n = 44) were obtained ecules, the stage-specific patterns were found to differ in cer- from children undergoing diagnostic BM aspiration for the fol- tain details from previously published concepts. Among the earliest BCP, a subset of CD34+CD10lo precursors was repeat- lowing diagnoses in the absence of BM involvement at the edly observed in addition to the well characterized time of immunologic investigation: suspicion of storage dis- CD34+CD10hiCD19+ majority of cells. Only two-thirds of these ease (n = 1), bacterial lymphadenitis (n = 1), neuroblastoma CD34+CD10lo cells expressed CD19. However, uniformity of (n = 1), severe aplastic anemia in remission (n = 2), single sys- phenotypic features, absence of T lineage markers, and the tem Langerhans cell histiocytosis (n = 1), idiopathic throm- regeneration kinetics after chemotherapy suggest the B lineage = + lo bocytopenic purpura (n 1), early stage (localized) non- affiliation of the CD34 CD10 precursors in general.