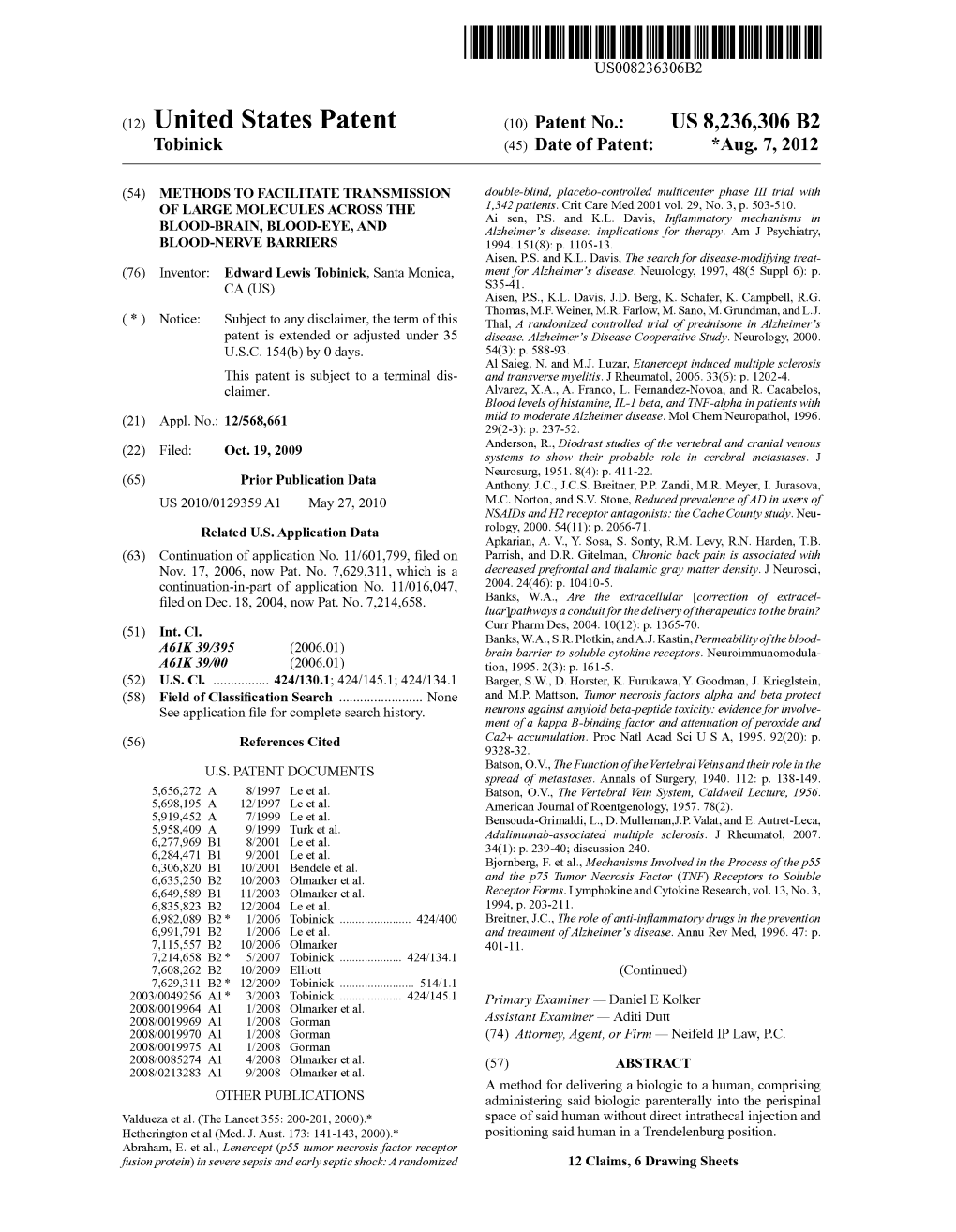
(12) United States Patent (10) Patent No.: US 8.236,306 B2 Tobinick (45) Date of Patent: *Aug
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arteries and Veins) of the Gastrointestinal System (Oesophagus to Anus)
2021 First Sitting Paper 1 Question 07 2021-1-07 Outline the anatomy of the blood supply (arteries and veins) of the gastrointestinal system (oesophagus to anus) Portal circulatory system + arterial blood flow into liver 1100ml of portal blood + 400ml from hepatic artery = 1500ml (30% CO) Oxygen consumption – 20-35% of total body needs Arterial Supply Abdominal Aorta • It begins at the aortic hiatus of the diaphragm, anterior to the lower border of vertebra T7. • It descends to the level of vertebra L4 it is slightly to the left of midline. • The terminal branches of the abdominal aorta are the two common iliac arteries. Branches of Abdominal Aorta Visceral Branches Parietal Branches Celiac. Inferior Phrenics. Superior Mesenteric. Lumbars Inferior Mesenteric. Middle Sacral. Middle Suprarenals. Renals. Internal Spermatics. Gonadal Anterior Branches of The Abdominal Aorta • Celiac Artery. Superior Mesenteric Artery. Inferior Mesenteric Artery. • The three anterior branches supply the gastrointestinal viscera. Basic Concept • Fore Gut - Coeliac Trunk • Mid Gut - Superior Mesenteric Artery • Hind Gut - Inferior Mesenteric Artery Celiac Trunk • It arises from the abdominal aorta immediately below the aortic hiatus of the diaphragm anterior to the upper part of vertebra LI. • It divides into the: left gastric artery, splenic artery, common hepatic artery. o Left gastric artery o Splenic artery ▪ Short gastric vessels ▪ Lt. gastroepiploic artery o Common hepatic artery ▪ Hepatic artery proper JC 2019 2021 First Sitting Paper 1 Question 07 • Left hepatic artery • Right hepatic artery ▪ Gastroduodenal artery • Rt. Gastroepiploic (gastro-omental) artery • Sup pancreatoduodenal artery • Supraduodenal artery Oesophagus • Cervical oesophagus - branches from inferior thyroid artery • Thoracic oesophagus - branches from bronchial arteries and aorta • Abd. -

Portal Vein: a Review of Pathology and Normal Variants on MDCT E-Poster: EE-005
Portal vein: a review of pathology and normal variants on MDCT e-Poster: EE-005 Congress: ESGAR2016 Type: Educational Exhibit Topic: Diagnostic / Abdominal vascular imaging Authors: C. Carneiro, C. Bilreiro, C. Bahia, J. Brito; Portimao/PT MeSH: Abdomen [A01.047] Portal System [A07.231.908.670] Portal Vein [A07.231.908.670.567] Hypertension, Portal [C06.552.494] Any information contained in this pdf file is automatically generated from digital material submitted to e-Poster by third parties in the form of scientific presentations. References to any names, marks, products, or services of third parties or hypertext links to third-party sites or information are provided solely as a convenience to you and do not in any way constitute or imply ESGAR’s endorsement, sponsorship or recommendation of the third party, information, product, or service. ESGAR is not responsible for the content of these pages and does not make any representations regarding the content or accuracy of material in this file. As per copyright regulations, any unauthorised use of the material or parts thereof as well as commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method is strictly prohibited. You agree to defend, indemnify, and hold ESGAR harmless from and against any and all claims, damages, costs, and expenses, including attorneys’ fees, arising from or related to your use of these pages. Please note: Links to movies, ppt slideshows and any other multimedia files are not available in the pdf version of presentations. www.esgar.org 1. Learning Objectives To review the embryology and anatomy of the portal venous system. -

Inferior Mesenteric Artery Abdominal Aorta
Gastro-intestinal Module Dr. Gamal Taha Abdelhady Assistant Professor of Anatomy & Embryology Blood Supply of the GIT Basic Concept ◼ Fore Gut ◼ Celiac Trunk ◼ Mid Gut ◼ Superior Mesenteric Artery ◼ Hind Gut ◼ Inferior Mesenteric Artery Abdominal Aorta ◼ It begins at the aortic hiatus of the diaphragm, anterior to the lower border of vertebra T12. ◼ It descends to the level of vertebra L4 it is slightly to the left of midline. ◼ The terminal branches of the abdominal aorta are the two common iliac arteries. Branches of Abdominal Aorta ◼ Visceral Branches ◼ Parietal Branches 1. Celiac (1). 2. Superior Mesenteric 1. Inferior Phrenics (1). (2). 3. Inferior Mesenteric 2. Lumbar arteries (1). 4. Middle Suprarenals 3. Middle Sacral (1). (2). 5. Renal arteries (2). 6. Gonadal arteries (2) Anterior Branches of The Abdominal Aorta 1. Celiac Artery. 2. Superior Mesenteric Artery. 3. Inferior Mesenteric Artery. ◼ The three anterior branches supply the gastrointestinal viscera. Celiac Trunk ◼ It arises from the abdominal aorta immediately below the aortic hiatus of the diaphragm anterior to the upper part of vertebra L1. ◼ It divides into the: ◼ Left gastric artery, ◼ Splenic artery, ◼ Common hepatic artery. Celiac Trunk • LEFT GASTRIC ARTERY: Lower part of esophagus and lesser curve of stomach • SPLENIC ARTERY – Short gastric vessels – Lt. gastroepiploic artery • COMMON HEPATIC ARTERY – Hepatic artery proper • Left hepatic artery • Right hepatic artery – Gastroduodenal artery gives off Rt. Gastroepiploic (gastro-omental ) artery and Superior pancreatoduodenal artery “Supra-duodenal artery” Superior Mesenteric Artery • It arises from the abdominal aorta immediately 1cm below the celiac artery anterior to the lower part of vertebra L1. • It is crossed anterior by the splenic vein and the neck of pancreas. -

Cardiovascular and Thoracic Surgery June 06-07, 2018 Osaka, Japan
conferenceseries.com June 2018 | Volume 9 | ISSN: 2155-9880 Journal of Clinical & Experimental Cardiology Proceedings of 24th International Conference on Cardiovascular and Thoracic Surgery June 06-07, 2018 Osaka, Japan Conference Series llc ltd 47 Churchfield Road, London, W3 6AY, UK Contact: 1-650-889-4686 Email: [email protected] conferenceseries.com 24th International Conference on Cardiovascular and Thoracic Surgery June 06-07, 2018 Osaka, Japan Keynote Forum (Day 1) Page 11 S Spagnolo, J Clin Exp Cardiolog 2018, Volume 9 conferenceseries.com DOI: 10.4172/2155-9880-C5-100 24th International Conference on Cardiovascular and Thoracic Surgery June 06-07, 2018 Osaka, Japan S Spagnolo GVM Care & Research, Italy The role of chronic superior caval syndrome and stenosis of jugular veins in neurodegenerative diseases. Surgical treatment and preliminary results hronic superior caval syndrome (CSCS) and stenosis of jugular have been suggested to play a role in the pathogenesis of Cseveral degenerative disorders of the central nervous system. Although controversy still remains as to whether anatomic and/or functional alterations of the cerebrospinal venous effluent really contribute to the development of the disease. Several reports have shown that restoration of a normal venous flow pattern by internal jugular veins (IJV) angioplasty (PTA) can improve neurological status and functional capacity. It is thought that in the event of a stenosis of the superior vena cava, the cerebrospinal venous circle normally flows into the jugular veins and brachiocephalic veins and, by means of the superior intercostal veins and the mammary veins, it reaches the azygos and inferior vena cava. Recent studies have demonstrated that in the presence of a stenosis of the vena cava or of the brachiocephalic or the jugular veins, venous blood can invert the direction of its flow and move towards the cerebrospinal circle. -

Blood Vessels and Circulation
19 Blood Vessels and Circulation Lecture Presentation by Lori Garrett © 2018 Pearson Education, Inc. Section 1: Functional Anatomy of Blood Vessels Learning Outcomes 19.1 Distinguish between the pulmonary and systemic circuits, and identify afferent and efferent blood vessels. 19.2 Distinguish among the types of blood vessels on the basis of their structure and function. 19.3 Describe the structures of capillaries and their functions in the exchange of dissolved materials between blood and interstitial fluid. 19.4 Describe the venous system, and indicate the distribution of blood within the cardiovascular system. © 2018 Pearson Education, Inc. Module 19.1: The heart pumps blood, in sequence, through the arteries, capillaries, and veins of the pulmonary and systemic circuits Blood vessels . Blood vessels conduct blood between the heart and peripheral tissues . Arteries (carry blood away from the heart) • Also called efferent vessels . Veins (carry blood to the heart) • Also called afferent vessels . Capillaries (exchange substances between blood and tissues) • Interconnect smallest arteries and smallest veins © 2018 Pearson Education, Inc. Module 19.1: Blood vessels and circuits Two circuits 1. Pulmonary circuit • To and from gas exchange surfaces in the lungs 2. Systemic circuit • To and from rest of body © 2018 Pearson Education, Inc. Module 19.1: Blood vessels and circuits Circulation pathway through circuits 1. Right atrium (entry chamber) • Collects blood from systemic circuit • To right ventricle to pulmonary circuit 2. Pulmonary circuit • Pulmonary arteries to pulmonary capillaries to pulmonary veins © 2018 Pearson Education, Inc. Module 19.1: Blood vessels and circuits Circulation pathway through circuits (continued) 3. Left atrium • Receives blood from pulmonary circuit • To left ventricle to systemic circuit 4. -

Pelvic Congestion Syndrome
Pelvic Congestion Syndrome Background Chronic pelvic pain, defined as non-cyclic pelvic pain of greater than 6 months duration, is a common presenting problem to the Gynaecologist. A third of all patients worked up for chronic pelvic pain with laparoscopy, have no obvious etiology. Pelvic congestion syndrome (PCS) has long been recognized as a cause of chronic pelvic pain, caused by retrograde flow down incompetent gonadal veins resulting in pelvic varicosities. This is anatomically analogous to the male varicocele, but because the pelvic varicosities are not externally visible or palpable, the diagnosis is most often elusive. The treatment of choice is the same as for a male varicocele, transcatheter gonadal vein embolization. Clinical Diagnosis The symptom complex can be best understood as the result of gravity related filling of the pelvic varicosities. The classic and almost pathognomonic presentation includes varying degrees of pelvic and lower back pain that is worsened with standing and exercising, and is therefore most severe at the end of the day. It is also often exacerbated with intercourse. Patients who usually describe the pain to be diminished or relieved in the supine position have the most relief upon awakening in the morning. The above presenting complaints are predictive of clinical success after transcatheter embolization of the varices and gonadal veins. The visualization of incompetent gonadal veins and associated pelvic varices has been difficult without performing invasive gonadal vein venography to demonstrate spontaneous reflux. Clinical pelvic examination is insensitive to recognise pelvic varicosities, unlike in the male of an enlarged scrotum with palpable varices. Transvaginal color Doppler ultrasound performed in a supine and upright positions with and without Valsalva is the best screening modality. -

Clinical Anatomy Flash Cards
! " #$$"" $ $%&'()'(*'+,)&*" front.card2.4.qxd 12/5/06 2:28 PM Page 1 Abdomen 2.4 Drainage of the Anterior Abdominal Wall 1 2 3 Transumbilical plane 4 5 6 Lymphatic Venous drainage drainage COA back.card2.4.qxd 12/4/06 3:16 PM Page 1 Drainage of the Anterior Abdominal Wall 1. axillary lymph nodes 2. axillary vein 3. thoracoepigastric vein 4. superficial inguinal lymph nodes 5. superficial epigastric vein 6. femoral vein Lymph superior to the transumbilical plane drains to the axil- lary lymph nodes, while lymph inferior to the plane drains to the superficial inguinal lymph nodes. When flow in the supe- rior or inferior vena cava is blocked, anastomoses between their tributaries, that is, the thoracoepi- gastric vein, may pro- vide collateral circula- tion, allowing the ob- struction to be bypassed. Thoracoepigastric vein COA © 2008 Lippincott Williams & Wilkins front.card2.36.qxd 12/5/06 1:20 PM Page 1 Abdomen 2.36 Portal System 1 3 4 2 6 5 7 Grant’s back.card2.36.qxd 12/4/06 3:28 PM Page 1 Portal System 1. inferior vena cava 2. hepatic portal vein 3. right gastric vein 4. splenic vein 5. superior mesenteric vein 6. inferior mesenteric vein 7. superior rectal veins Caput Medusae When scarring and fibrosis from cir- rhosis obstruct the portal vein, pres- sure in the portal vein rises and pro- duces portal hypertension. The blood then flows to into the systemic system at places of portal-systemic anastomo- sis, producing varicose veins. Caput medusae is caused by the veins of the anterior abdominal wall becoming dilated from portal hypertension. -

Prenatal Diagnosis of Agenesis of Ductus Venosus: a Retrospective Study of Anatomic Variants, Associated Anomalies and Impact On
Published online: 2017-09-21 Original Article Prenatal Diagnosis of Agenesis of Ductus Venosus: A Retrospective Study of Anatomic Variants, Associated Anomalies and Impact on Postnatal Outcome Pränatale Agenesie des Ductus venosus: retrospektive Analyse anatomischer Varianten, assoziierter Fehlbildungen und Einfluss auf das postnatale Outcome Authors Brigitte Strizek1, *, Aikaterini Zamprakou1, *, Ingo Gottschalk2, Maria Roethlisberger2, Astrid Hellmund1, Andreas Müller3, Ulrich Gembruch1, Annegret Geipel1, Christoph Berg2 Affiliations ed. Charts were reviewed for associated structural or chromo- 1 Obstetrics and Prenatal Medicine, University Hospital somal anomalies, pregnancy outcome and postnatal course. Bonn, Germany Results In 24 cases (20.2 %) ADV was an isolated finding, 2 Division of Prenatal Medicine and Gynecologic while 95 cases (79.8 %) had associated anomalies. We identi- Sonography, Department of Obstetrics and Gynecology, fied 84 cases (70.6 %) with intrahepatic and 35 cases (29.4 %) University Hospital Cologne, Germany with extrahepatic drainage of the umbilical vein. 58.8 % of 3 Neonatology, Children's University Hospital Bonn, neonates were alive at follow-up. There was no statistical as- Germany sociation between drainage site and associated anomalies or outcome. Postnatal outcome was determined by the presence Key words and severity of associated anomalies. There was no adverse portosystemic shunt, intrahepatic drainage, extrahepatic outcome in the isolated group related to ADV. Overall, there drainage, outcome, ductus venosus agenesis were 6 persistent portosystemic shunts, 3 of them with a received 28.12.2016 spontaneous closure, and one total agenesis of the portal ve- accepted 21.06.2017 nous system with lethal outcome. Conclusion Postnatal outcome in cases with ADV mainly Bibliography depends on the presence of associated anomalies. -

A Syllabus of Core Surgical Anatomy
A Syllabus of Core Surgical Anatomy Background In February 2010, it was agreed that the Anatomy Committee would undertake to develop a new generic examination for implementation in 2012 to assess anatomy for surgical trainees. Content Anatomical questions relate to: • clinical examination – surface anatomy, inspection, palpation, percussion, auscultation, pelvic examination, testing for peripheral nerve injuries, potential sites of spread of tumours (as determined by anatomy e.g. lymphatic drainage of the breast) • urethral catheterization • vascular access (arterial and venous, peripheral and central) • the airway: maintenance, access • chest drainage • imaging (plain radiographs, CT, MRI, US, contrast studies) • surgical access – open and minimally invasive • endoscopy (GI, arthroscopy etc) • peripheral nerve blocks • percutaneous liver biopsy • trauma (aligned to anatomy in EMST) • common anatomical complications of routine surgical procedures • principles of anatomy: terminology, anatomical position, planes, relationships in regional anatomy, movements, tissues, systems, and anatomical variation. Syllabus Essential (+++) • What an early SET 1 trainee (PGY 2-3 with general experience) should know. • Must recognise, understand and be able to explain. • These structures comprise core basic surgical anatomy and are essential in inter-specialty communication. • Lack of knowledge could jeapordise patient safety. • Includes all common and important anatomical characteristics of the structure: location, constituent parts, relations, blood supply and lymphatic drainage, innervation, course and distribution, when the structure is at risk, effects of injury, and common variants of clinical importance. Desirable (++) • Should be able to describe the basic anatomy/location of the structure, its function, major nerve and blood supply ± lymphatic drainage, and general relations. Non-core (+) • Not considered core knowledge but may be appropriate for specialty-specific anatomy. -

Introduction of Circulatory System Process
INTRODUCTION OF CIRCULATORY SYSTEM PROCESS Qi Lin The Pennsylvania State University INTRODUCTION OF CIRCULATORY SYSTEM PROCESS Introduction Cardiovascular Circulation The circulatory system (shown in Figure An average adult has a heart (shown in 1), is an organ system that allows blood to Figure 2) that is about 14cm long by 9 cm circulate and transport nutrients, oxygen, wide. It’s approximately the size of a man’s carbon dioxide, hormones, and blood cells to closed fist. The heart pumps approximately provide nourishment, fight disease, stabilize 7,000 L of blood every day. Statistics show temperature, and maintain homeostasis. The that the heart will contract about 2.5 billion circulatory system, as simply a highway for times in an average person’s life. It contains blood, is made up of three independent four chambers in total: systems that work together: the heart (cardiovascular circulation), lungs Left atrium - the upper left chamber (pulmonary circulation); and arteries, veins, of the heart and coronary and portal vessels (systemic Left ventricle - the lower left circulation). The circulatory systems of chamber of the heart humans are close, which means that the blood Light atrium - the upper right in humans’ body never leaves the network of chamber of the heart blood vessels. In contrast, oxygen, carbon Right ventricle - the lower right dioxide and nutrients diffuse cross the blood chamber of the heart and cells. There is one atrium and one ventricle involved in each circulation in the human heart. For systemic circulation, the left ventricle and the right atrium play important roles. The left ventricle receives the oxygenated blood from the lungs. -

The Cerebrospinal Venous System: Anatomy, Physiology, and Clinical Implications Edward Tobinick, MD
5/8/2017 www.medscape.org/viewarticle/522597_print www.medscape.org The Cerebrospinal Venous System: Anatomy, Physiology, and Clinical Implications Edward Tobinick, MD Posted: 2/22/2006 Abstract and Introduction Abstract There is substantial anatomical and functional continuity between the veins, venous sinuses, and venous plexuses of the brain and the spine. The term "cerebrospinal venous system" (CSVS) is proposed to emphasize this continuity, which is further enhanced by the general lack of venous valves in this network. The first of the two main divisions of this system, the intracranial veins, includes the cortical veins, the dural sinuses, the cavernous sinuses, and the ophthalmic veins. The second main division, the vertebral venous system (VVS), includes the vertebral venous plexuses which course along the entire length of the spine. The intracranial veins richly anastomose with the VVS in the suboccipital region. Caudally, the CSVS freely communicates with the sacral and pelvic veins and the prostatic venous plexus. The CSVS constitutes a unique, largecapacity, valveless venous network in which flow is bidirectional. The CSVS plays important roles in the regulation of intracranial pressure with changes in posture, and in venous outflow from the brain. In addition, the CSVS provides a direct vascular route for the spread of tumor, infection, or emboli among its different components in either direction. Introduction "... we begin to wonder whether our conception of the circulation today is completely acceptable. As regards the venous part of the circulation, I believe our present conception is incorrect." Herlihy[1] "It seems incredible that a great functional complex of veins would escape recognition as a system until 1940.. -

Tumor Thrombus: Incidence, Imaging, Prognosis and Treatment
177 Review Article Tumor thrombus: incidence, imaging, prognosis and treatment Keith Bertram Quencer1, Tamir Friedman2, Rahul Sheth3, Rahmi Oklu4 1Department of Radiology, University of Utah, Salt Lake City, UT, USA; 2Division of Interventional Radiology, Department of Radiology, Cornell University, New York, NY, USA; 3Division of Interventional Radiology, Department of Radiology, MD Anderson Cancer, Houston, TX, USA; 4Division of Interventional Radiology, Department of Radiology, Mayo Clinic-Arizona, Phoenix, AZ, USA Contributions: (I) Conception and design: R Oklu, KB Quencer, T Friedman; (II) Administrative support: KB Quencer, R Oklu, R Sheth; (III) Provision of study material or patients: None; (IV) Collection and assembly of data: None; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Keith Bertram Quencer, MD. Department of Radiology, University of Utah, Salt Lake City, UT, USA. Email: [email protected]. Abstract: Intravascular tumor extension, also known as tumor thrombus, can occur in many different types of cancer. Those with the highest proclivity include Wilm’s tumor, renal cell carcinoma (RCC), adrenal cortical carcinoma (ACC) and hepatocellular carcinoma (HCC). The presence of tumor thrombus markedly worsens prognosis and impacts treatment approach. Imaging plays a key role in its diagnosis. Endovascular methods also play a large role in treatment. Keywords: Tumor thrombus; renal cell carcinoma (RCC); hepatocellular carcinoma (HCC) Submitted Jul 07, 2017. Accepted for publication Sep 12, 2017. doi: 10.21037/cdt.2017.09.16 View this article at: http://dx.doi.org/10.21037/cdt.2017.09.16 Introduction Intravascular tumor thrombus is defined as tumor extension into a vessel.