Immusant(1).Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Report, Please Call the Telephone Number Listed
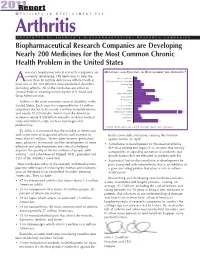
201R1e port M E D I C I N E S I N D E V E L O P M E N T F O R Arthritis P R E S E N T E D B Y A M E R I C A ’ S B I O P H A R M A C E U T I C A L R E S E A R C H C O M P A N I E S Biopharmaceutical Research Companies are Developing Nearly 200 Medicines for the Most Common Chronic Health Problem in the United States merica’s biopharmaceutical research companies are MEDICINES AND VACCINES IN DEVELOPMENT FOR ARTHRITIS* currently developing 198 medicines to help the Behcet’s Syndrome 3 more than 50 million Americans afflicted with at A Duchenne Muscular Dystrophy 6 least one of the 100 different musculoskeletal disorders, Fibromyalgia 9 including arthritis. All of the medicines are either in Gout 7 clinical trials or awaiting review by the U.S. Food and Lupus 19 Muscle Disorders 11 Drug Administration. Osteoarthritis 19 Osteoporosis 23 Arthritis is the most common cause of disability in the Pain 15 United States. Each year, it is responsible for 44 million Psoriatic Arthritis 7 outpatient doctor visits, nearly 1 million hospitalizations, Raynaud’s Disease 4 and nearly 10,000 deaths. And it costs the American Rheumatoid Arthritis 67 Scleroderma 6 economy nearly $128 billion annually in direct medical Spondylitis 7 costs and indirect costs, such as lost wages and Other 22 productivity. * Some medicines are listed in more than one category. -

Modulating Igg Effector Function by FC Engineering and Glycoengineering Andy Racher † & Olga Obrezanova ‡
Modulating IgG effector function by FC engineering and glycoengineering Andy Racher † & Olga Obrezanova ‡ Lonza Biologics, 228 Bath Road, Slough, Berkshire, SL1 4DX, UK † Corresponding author: [email protected] ‡ Current address: AstraZeneca, Cambridge, UK 2 Summary several Fc engineered and glycoengineered antibodies in late stage clinical trials. Several proprietary technologies were Antibodies are the fastest growing group of biotherapeutics. In developed for glycoengineering of monoclonal antibodies early 2020 more than 100 antibody-based molecules, including including Potelligent® technology (KHK / BioWa), GlycoMAb® biosimilars, had been approved globally. Oncology and (GlycArt / Roche), EMABLing® (LFB), GlycoExpress™ (Glycotope) inflammatory disorders remain the major therapeutic areas for and GlymaxX® (ProBioGen). antibody-based molecules but there is a growing interest in using mAbs for treating infectious disease. During the last 10 Encouraging clinical results and prospects in multiple disease years antibody engineering focussed on development of “fit- areas make it likely that more Fc engineered and for-purpose” antibodies with modulated effector functions glycoengineered antibodies will enter clinical trials and such as increased or muted antibody-dependent cell-mediated subsequently be approved. According to market research cytotoxicity (ADCC), antibody-dependent cellular phagocytosis studies, the glycoengineered antibodies are likely to emerge as (ADCP), complement dependent cytotoxicity (CDC), and to the forerunner in the short term (84% of the market share by increase half-life. This paper summarises approaches for 2021) and, subsequently, the Fc protein engineered antibodies modulating antibody effector functions and pharmacokinetics, are likely to gain a higher proportion (55% by 2026). and provides examples of antibodies in clinical studies Glycoengineering strategies focussing on enhancing ADCC employing such approaches. -

826.Full.Pdf
Emerging Treatments and Technologies ORIGINAL ARTICLE Failure to Preserve -Cell Function With Mycophenolate Mofetil and Daclizumab Combined Therapy in Patients With New- Onset Type 1 Diabetes 1 6 PETER A. GOTTLIEB, MD DESMOND A. SCHATZ, MD tions Trial (DCCT) demonstrated that im- 2 7 SCOTT QUINLAN, MS ANTOINETTE M. MORAN, MD proved metabolic control reduces chronic 2 2 HEIDI KRAUSE-STEINRAUF, MS JOHN M. LACHIN, SCD 3 8 complications in type 1 diabetes (5). A CARLA J. GREENBAUM, MD JAY S. SKYLER, MD 4 post hoc analysis of DCCT found that DARRELL M. WILSON, MD FOR THE TYPE 1DIABETES TRIALNET 5 those with residual -cell function, man- HENRY RODRIGUEZ, MD MMF/DZB STUDY GROUP* ifested by C-peptide values Ͼ0.2 pmol/ ml, had both less hypoglycemia and fewer complications than those without resid- OBJECTIVE — This trial tested whether mycophenolate mofetil (MMF) alone or with dacli-  ual function (6). Thus an intervention zumab (DZB) could arrest the loss of insulin-producing -cells in subjects with new-onset type that prolongs -cell function would be 1 diabetes. expected to improve metabolic control RESEARCH DESIGN AND METHODS — A multi-center, randomized, placebo- and reduce complications (7). controlled, double-masked trial was initiated by Type 1 Diabetes TrialNet at 13 sites in North Mycophenolic acid (MPA) was dis- America and Europe. Subjects diagnosed with type 1 diabetes and with sufficient C-peptide covered in 1896 and characterized in within 3 months of diagnosis were randomized to either MMF alone, MMF plus DZB, or placebo, 1952. Mycophenolate mofetil (MMF) is and then followed for 2 years. -

Teplizumab Surprise Puts Spotlight on Type 1 Diabetes Antibodies
August 09, 2013 Teplizumab surprise puts spotlight on type 1 diabetes antibodies Jonathan Gardner Type 1 diabetes has proven an R&D graveyard, with approaches ranging from therapeutic vaccines to anti- inflammatory compounds failing to have a disease-modifying effect on the autoimmune disease. So positive phase II results for a once-abandoned antibody could raise hopes of some progress in preserving pancreatic function. In an investigator-led study, MacroGenics’ teplizumab slowed the decline in patients’ blood levels of C-peptide, a biomarker for insulin production. A scan of pipeline data in EvaluatePharma finds three other candidates still listed in active development for type 1 diabetes in the same drug class, an anti-CD3 monoclonal antibody, and all are preclinical (see table). Thus, if Macrogenics or its academic or potential commercial partners can design a successful study, the project might have an open field, although it still seems a long shot. If at first you don't succeed MacroGenics’ partner Lilly had handed back rights to teplizumab in 2010 after failure of the phase III Protégé trial – two 14-day courses had no effect on insulin use or blood sugar one year after completion of dosing. This presaged the failure of a similar candidate, Tolerx and GlaxoSmithKline’s otelixizumab, in 2011 (Otelixizumab another disappointment in type 1 diabetes, March 14, 2011). Anti-CD3 antibodies bind to an epitope on T-cells, modulating their activity in attacking insulin-secreting beta cells, although the trials so far have not shown any significant effect on outcomes. But the new study, backed by Yale University and the National Institutes of Health, dosed 63 patients with teplizumab for 14 days at the beginning of treatment and again after one year. -

Zacks Small-Cap Research April 12, 2021
Zacks Small-Cap Research April 12, 2021 Sponsored – Impartial – Comprehensive John D. Vandermosten, CFA 312-265-9588 / [email protected] scr.zacks.com 10 S. Riverside Plaza, Suite 1600, Chicago, IL 60606 Tiziana Life Sciences PLC (TLSA - NASDAQ) INITIATION In A Tizzy about Tiziana Tiziana is a research and development company developing three main candidates for a variety of indications in autoimmune disease, cancer and COVID. The lead candidate, foralumab, is a fully human anti-CD3 Based on our DCF model and a 15% discount rate, Tiziana is antibody, being investigated in multiple sclerosis (MS), Crohn’s disease valued at approximately $7.50 per ADR share. Our model ap- (CD) and COVID, administered intranasally and orally via enteric coated capsules. milciclib is the second candidate and is being investigated as a plies a 15% probability of ultimate approval and commercializa- tion for the portfolio of assets including foralumab and milciclib. combination product in multiple oncology indications. The third candi- The model includes contributions from the United States and date, TZLS-501, is an anti-IL-6R receptor antibody expected to be the subject of an IND submitted in 2021. TZLS-501 is being investigated as a global developed markets. treatment for COVID and other pulmonary diseases such as ARDS. Ph2 foralumab clinical trials for MS and CD are targeted for 2021 & Ph2 combination trials for milciclib in coming quarters. Tiziana differentiates Current Price (4/9/2021) $2.67 itself in the use of intranasal, oral and inhaled formulations of mAbs that are able to avoid shortcomings of infused & subcutaneous administra- Valuation $7.50 tion. -

New Mechanisms and Expanded Indications for Biologic Therapies: a Perspective on Immunology Research and Development
New mechanisms_Layout 1 27/09/2010 13:57 Page 87 Therapeutics New mechanisms and expanded indications for biologic therapies: a perspective on immunology research and development Over the past decade, the introduction of biologic therapies has had a profound impact for millions of patients with immune-mediated arthritides, inflammatory bowel diseases and plaque psoriasis. Today, five anti-Tumor Necrosis Factor (TNF) therapies are approved in the United States and many countries around the world, and innovations in the TNF class continue more than a decade after the initial approval. Several other biologic therapies targeting distinct immune cell receptors or cytokines have been approved for immunologically mediated diseases, and many promising new biologic medicines are in various stages of clinical development. n this article I will provide an overview of adalimumab (HUMIRA®) for rheumatoid arthri- By Dr Susan B. Dillon some of the current trends influencing the tis (RA) in 1998 and 2002, respectively, the devel- I development of new biologics for immune- opment of anti-TNF biologics has continued. mediated and inflammatory diseases including Infliximab is now approved for 15 indications in 1) the continued clinical development of biologics the US (Table 1)1. In 2009, golimumab (SIM- targeting TNF-␣; 2) new mechanisms in inflamma- PONI®), a human monoclonal antibody (mAb) tion that are being explored in clinical trials and with once-monthly subcutaneous (SC) dosing 3) recent advances in the application of new bio- received approvals for RA, psoriatic arthritis logic therapies to an expanded list of indications (PsA) and ankylosing spondylitis (AS). Another with high unmet medical need. -

Assessment of the Evolution of Cancer Treatment Therapies
Cancers 2011, 3, 3279-3330; doi:10.3390/cancers3033279 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Assessment of the Evolution of Cancer Treatment Therapies Manuel Arruebo 1,2, Nuria Vilaboa 2,3, Berta Sáez-Gutierrez 1,4,5, Julio Lambea 1,4,5, Alejandro Tres 1,4,5, Mónica Valladares 6 and África González-Fernández 7,* 1 Instituto de Nanociencia de Aragón (INA), Mariano Esquillor, Edif. I+D, University of Zaragoza, Zaragoza 50018, Spain; E-Mails: [email protected] (M.A.); [email protected] (B.S.); [email protected] (J.L.); [email protected] (A.T.) 2 CIBER de Bioingeniería, Biomateriales y Nanomedicina (CIBER-BBN), Zaragoza 50018, Spain; E-Mail: [email protected] (N.V.) 3 Hospital Universitario La Paz-IdiPAZ, Paseo de la Castellana 261, Madrid 28046, Spain 4 Servicio de Oncología Médica, Hospital Clínico Universitario Lozano Blesa, Avda. San Juan Bosco 50009, Zaragoza, Spain 5 Instituto Aragonés de Ciencias de la Salud (I+CS), Avda. Gómez Laguna, 25, Zaragoza 50009, Spain 6 Lonza Biologics Porriño, A relva s/n, Porriño (Pontevedra) 36410, Spain; E-Mail: [email protected] (M.V.) 7 Immunology Department, Biomedical Research Center (CINBIO), University of Vigo, Campus Lagoas Marcosende, Vigo (Pontevedra) 36310, Spain * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +34-986812625; Fax: +34-986-812556. Received: 16 June 2011; in revised form: 7 July 2011 / Accepted: 8 August 2011 / Published: 12 August 2011 Abstract: Cancer therapy has been characterized throughout history by ups and downs, not only due to the ineffectiveness of treatments and side effects, but also by hope and the reality of complete remission and cure in many cases. -

Biotechnology Presented by America’S Biopharmaceutical Research Companies
2011 REPORT 2011 Medicines in Development BIOTECHNOLOGY presented by america’s biopharmaceutical research companies Biotechnology Research Promises to Bolster the Future of Medicine with More Than 900 Medicines and Vaccines in Development In the human body there are Biotechnology Medicines 12 trillion cells, in Development 200,000 proteins and 25,000 genes 300 298 America’s biopharmaceutical research compa- The biotechnology medicines now in develop- nies are using biotechnology to develop 901 ment make use of these and other state-of- medicines and vaccines targeting more than the-art approaches. For example: 100 diseases. Biotechnology medicines are developed through biological processes using • A genetically-modified virus-based living cells or organisms, rather than the tra- vaccine to treat melanoma. ditional chemical synthesis approach. These • A monoclonal antibody for the treatment medicines in development are either in human of cancer and asthma. clinical trials or under review by the U.S. Food and Drug Administration. • An antisense medicine for the treatment of cancer. Biotechnology medicines use many different • A recombinant fusion protein to treat 78 cutting-edge approaches to treat disease. A age-related macular degeneration. 64 monoclonal antibody is a laboratory-made 50 version of the naturally occurring immune These are only a few examples of the new system protein that binds to and neutralizes ways America’s biopharmaceutical research foreign invaders. Interferons are proteins that companies are attacking disease through bio- 23 interfere with the ability of a cell to reproduce. technology. The 901 biotechnology medicines Antisense drugs are medicines that interfere and vaccines in development promise to push with the communication process that tells a the frontiers of science and potentially bring e y cell to produce an unwanted protein. -

Potential Application of Tregitopes As Immunomodulating Agents in Multiple Sclerosis
Hindawi Publishing Corporation Neurology Research International Volume 2011, Article ID 256460, 6 pages doi:10.1155/2011/256460 Review Article Potential Application of Tregitopes as Immunomodulating Agents in Multiple Sclerosis Wassim Elyaman,1 Samia J. Khoury,1 David W. Scott,2 and Anne S. De Groot3 1 Center for Neurologic Diseases, Brigham and Women’s Hospital and Harvard Medical School, 77 Avenue Louis Pasteur, NRB 641, Boston, MA 02115, USA 2 Uniformed Services University of the Health Sciences, Bethesda, MD 20814, USA 3 EpiVax Inc., University of Rhode Island, Providence, RI 02903, USA Correspondence should be addressed to Wassim Elyaman, [email protected] Received 19 April 2011; Accepted 14 July 2011 Academic Editor: Changiz Geula Copyright © 2011 Wassim Elyaman et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The induction of immunologic tolerance is an important clinical goal in autoimmunity. CD4+ regulatory T (Treg) cells, defined by the expression of the transcription factor forkhead box P3 (FoxP3), play a central role in the control of autoimmune responses. Quantitative and qualitative defects of Tregs have been postulated to contribute to failed immune regulation in multiple sclerosis (MS) and other autoimmune diseases. This paper highlights the potential uses of T regulatory cell epitopes (Tregitopes), natural Treg epitopes found to be contained in human immunoglobulins, as immunomodulating agents in MS. Tregitopes expand Treg cells and induce “adaptive Tregs” resulting in immunosuppression and, therefore, are being considered as a potential therapy for autoimmune diseases. -

2011 Medicines in Development for Women
201R1e port M E D I C I N E S I N D E V E L O P M E N T F O R Women P R E S E N T E D B Y A M E R I C A ’ S B I O P H A R M A C E U T I C A L R E S E A R C H C O M P A N I E S More Than 800 Medicines Are in Testing for Diseases Disproportionately Affecting American Women merica’s pharmaceutical research and biotech - MEDICINES AND VACCINES IN DEVELOPMENT FOR WOMEN* nology companies are developing 851 medicines Afor diseases that disproportionately affect American women. The medicines in the pipeline for women (either in clinical trials or awaiting review by the Food and Drug Administration) include: • 139 for cancers affecting women, including 91 for breast cancer, 49 for ovarian cancer, and 9 for cervical cancer. • 114 for arthritis/musculoskeletal disorders. Approximately 46 million Americans have some type of arthritis or related condition, and 60 percent of them are female. • 64 for obstetric/gynecologic conditions. • 110 for autoimmune diseases, which strike women three times more than men. • 72 for depression and anxiety. Almost twice as many women as men suffer from these disorders. * Some medicines are listed in more than one category. • 83 for Alzheimer’s disease. Two-thirds (3.4 million) of In separate reports, PhRMA has found that researchers the 5.4 million Americans living with Alzheimer’s are working on 299 medicines for heart disease and today are women.