826.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fig. L COMPOSITIONS and METHODS to INHIBIT STEM CELL and PROGENITOR CELL BINDING to LYMPHOID TISSUE and for REGENERATING GERMINAL CENTERS in LYMPHATIC TISSUES
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ 23 February 2012 (23.02.2012) WO 2U12/U24519ft ft A2 (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61K 31/00 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US201 1/048297 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 18 August 201 1 (18.08.201 1) NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (25) Filing Language: English TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (26) Publication Language: English ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/374,943 18 August 2010 (18.08.2010) US kind of regional protection available): ARIPO (BW, GH, 61/441,485 10 February 201 1 (10.02.201 1) US GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, 61/449,372 4 March 201 1 (04.03.201 1) US ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (72) Inventor; and EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, ΓΓ, LT, LU, (71) Applicant : DEISHER, Theresa [US/US]; 1420 Fifth LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, Avenue, Seattle, WA 98101 (US). -
Report, Please Call the Telephone Number Listed
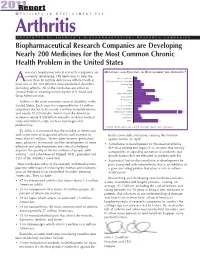
201R1e port M E D I C I N E S I N D E V E L O P M E N T F O R Arthritis P R E S E N T E D B Y A M E R I C A ’ S B I O P H A R M A C E U T I C A L R E S E A R C H C O M P A N I E S Biopharmaceutical Research Companies are Developing Nearly 200 Medicines for the Most Common Chronic Health Problem in the United States merica’s biopharmaceutical research companies are MEDICINES AND VACCINES IN DEVELOPMENT FOR ARTHRITIS* currently developing 198 medicines to help the Behcet’s Syndrome 3 more than 50 million Americans afflicted with at A Duchenne Muscular Dystrophy 6 least one of the 100 different musculoskeletal disorders, Fibromyalgia 9 including arthritis. All of the medicines are either in Gout 7 clinical trials or awaiting review by the U.S. Food and Lupus 19 Muscle Disorders 11 Drug Administration. Osteoarthritis 19 Osteoporosis 23 Arthritis is the most common cause of disability in the Pain 15 United States. Each year, it is responsible for 44 million Psoriatic Arthritis 7 outpatient doctor visits, nearly 1 million hospitalizations, Raynaud’s Disease 4 and nearly 10,000 deaths. And it costs the American Rheumatoid Arthritis 67 Scleroderma 6 economy nearly $128 billion annually in direct medical Spondylitis 7 costs and indirect costs, such as lost wages and Other 22 productivity. * Some medicines are listed in more than one category. -

Looking for Therapeutic Antibodies in Next Generation Sequencing Repositories
bioRxiv preprint doi: https://doi.org/10.1101/572958; this version posted March 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Title: Looking for Therapeutic Antibodies in Next Generation Sequencing Repositories. Authors: Konrad Krawczyk1*, Matthew Raybould2, Aleksandr Kovaltsuk2, Charlotte M. Deane2 1 NaturalAntibody, Hamburg, Germany 2 Oxford University Department of Statistics, Oxford, UK *Correspondence to [email protected] Abstract: Recently it has become possible to query the great diversity of natural antibody repertoires using Next Generation Sequencing (NGS). These methods are capable of producing millions of sequences in a single experiment. Here we compare Clinical Stage Therapeutic antibodies to the ~1b sequences from 60 independent sequencing studies in the Observed Antibody Space Database. Of the 242 post Phase I antibodies, we find 16 with sequence identity matches of 95% or better for both heavy and light chains. There are also 54 perfect matches to therapeutic CDR-H3 regions in the NGS outputs, suggesting a nontrivial amount of convergence between naturally observed sequences and those developed artificially. This has potential implications for both the discovery of antibody therapeutics and the legal protection of commercial antibodies. Introduction Antibodies are proteins in jawed vertebrates that recognize noxious molecules (antigens) for elimination. An organism expresses millions of diverse antibodies to increase the chances that some of them will be able to bind the foreign antigen, initiating the adaptive immune response. -
![Insulin Is Necessary but Not Sufficient: Changing the Therapeutic Paradigm in Type 1 Diabetes [Version 1; Peer Review: 5 Approved] Sandra Lord , Carla J](https://docslib.b-cdn.net/cover/5644/insulin-is-necessary-but-not-sufficient-changing-the-therapeutic-paradigm-in-type-1-diabetes-version-1-peer-review-5-approved-sandra-lord-carla-j-1015644.webp)
Insulin Is Necessary but Not Sufficient: Changing the Therapeutic Paradigm in Type 1 Diabetes [Version 1; Peer Review: 5 Approved] Sandra Lord , Carla J
F1000Research 2020, 9(Faculty Rev):827 Last updated: 30 JUL 2020 REVIEW Insulin is necessary but not sufficient: changing the therapeutic paradigm in type 1 diabetes [version 1; peer review: 5 approved] Sandra Lord , Carla J. Greenbaum Benaroya Research Institute at Virginia Mason, Seattle, WA, 98101, USA First published: 30 Jul 2020, 9(Faculty Rev):827 Open Peer Review v1 https://doi.org/10.12688/f1000research.21801.1 Latest published: 30 Jul 2020, 9(Faculty Rev):827 https://doi.org/10.12688/f1000research.21801.1 Reviewer Status Abstract Invited Reviewers Despite the clear evidence that type 1 diabetes (T1D) begins well before 1 2 3 4 5 hyperglycemia is evident, there are no clinically available disease-modifying therapies for early-stage disease. However, following the exciting results of version 1 the Teplizumab Prevention Study, the first study to demonstrate that overt 30 Jul 2020 T1D can be delayed with immunotherapy, there is renewed optimism that in the future, T1D will be treated before hyperglycemia develops. A different treatment paradigm is needed, as a majority of people with T1D do not meet the glycemic targets that are associated with a lower risk of T1D Faculty Reviews are review articles written by the complications and therefore remain vulnerable to complications and prestigious Members of Faculty Opinions. The shortened life expectancy. The following review will outline the history and articles are commissioned and peer reviewed before current status of immunotherapy for T1D and highlight some challenges publication to ensure that the final, published version and ideas for the future. Although such efforts have been worldwide, we will focus particularly on the activities of Diabetes TrialNet, a National Institutes is comprehensive and accessible. -

Modulating Igg Effector Function by FC Engineering and Glycoengineering Andy Racher † & Olga Obrezanova ‡
Modulating IgG effector function by FC engineering and glycoengineering Andy Racher † & Olga Obrezanova ‡ Lonza Biologics, 228 Bath Road, Slough, Berkshire, SL1 4DX, UK † Corresponding author: [email protected] ‡ Current address: AstraZeneca, Cambridge, UK 2 Summary several Fc engineered and glycoengineered antibodies in late stage clinical trials. Several proprietary technologies were Antibodies are the fastest growing group of biotherapeutics. In developed for glycoengineering of monoclonal antibodies early 2020 more than 100 antibody-based molecules, including including Potelligent® technology (KHK / BioWa), GlycoMAb® biosimilars, had been approved globally. Oncology and (GlycArt / Roche), EMABLing® (LFB), GlycoExpress™ (Glycotope) inflammatory disorders remain the major therapeutic areas for and GlymaxX® (ProBioGen). antibody-based molecules but there is a growing interest in using mAbs for treating infectious disease. During the last 10 Encouraging clinical results and prospects in multiple disease years antibody engineering focussed on development of “fit- areas make it likely that more Fc engineered and for-purpose” antibodies with modulated effector functions glycoengineered antibodies will enter clinical trials and such as increased or muted antibody-dependent cell-mediated subsequently be approved. According to market research cytotoxicity (ADCC), antibody-dependent cellular phagocytosis studies, the glycoengineered antibodies are likely to emerge as (ADCP), complement dependent cytotoxicity (CDC), and to the forerunner in the short term (84% of the market share by increase half-life. This paper summarises approaches for 2021) and, subsequently, the Fc protein engineered antibodies modulating antibody effector functions and pharmacokinetics, are likely to gain a higher proportion (55% by 2026). and provides examples of antibodies in clinical studies Glycoengineering strategies focussing on enhancing ADCC employing such approaches. -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -
(12) Patent Application Publication (10) Pub. No.: US 2015/0250896 A1 Zhao (43) Pub
US 20150250896A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0250896 A1 Zhao (43) Pub. Date: Sep. 10, 2015 (54) HYDROPHILIC LINKERS AND THEIR USES Publication Classification FOR CONUGATION OF DRUGS TO A CELL (51) Int. Cl BNDING MOLECULES A647/48 (2006.01) (71) Applicant: Yongxin R. ZHAO, Henan (CN) Ek E. 30.8 C07D 207/216 (2006.01) (72) Inventor: R. Yongxin Zhao, Lexington, MA (US) C07D 40/12 (2006.01) C07F 9/30 (2006.01) C07F 9/572 (2006.01) (73) Assignee: Hangzhou DAC Biotech Co., Ltd., (52) U.S. Cl. Hangzhou City, ZJ (CN) CPC ........... A61K47/48715 (2013.01); C07F 9/301 (2013.01); C07F 9/65583 (2013.01); C07F (21) Appl. No.: 14/432,073 9/5721 (2013.01); C07D 207/46 (2013.01); C07D 401/12 (2013.01); A61 K3I/454 (22) PCT Filed: Nov. 24, 2012 (2013.01) (86). PCT No.: PCT/B2O12/0567OO Cell(57) binding- agent-drugABSTRACT conjugates comprising hydrophilic- S371 (c)(1), linkers, and methods of using Such linkers and conjugates are (2) Date: Mar. 27, 2015 provided. Patent Application Publication Sep. 10, 2015 Sheet 1 of 23 US 2015/0250896 A1 O HMDS OSiMe 2n O Br H-B-H HPC 3 2 COOEt essiop-\5. E B to NH 120 °C, 2h OsiMe3 J 50 °C, 2h eSiO OEt 120 oC, sh 1 2 3. 42% from 1 Bra-11a1'oet - Brn 11-1 or a 1-1 or ÓH 140 °C ÓEt ÓEt 4 5 6 - --Messio. 8 B1a-Br aus 20 cc, hP-1}^-'ot Br1-Y. -

Anti-CD3 Drug Keeps Diabetes at Bay No Drug Has Ever Delayed Islet Cell Destruction
news IN this section β-thalassemia Gilead, Galapagos Biotech news from gene therapy in $5.1 billion tie around the world approved p1102 p1104 p1106 Anti-CD3 drug keeps diabetes at bay No drug has ever delayed islet cell destruction. Now that teplizumab has, the challenge turns to identifying eligible recipients for the treatment. he first drug to ever slow the progression from pre-diabetes to Tclinical type 1 diabetes is one step closer to reaching the market. On August 5, the US Food and Drug Administration (FDA) granted breakthrough therapy designation to teplizumab, a CD3-targeted antibody from Provention Bio, to prevent or delay type 1 diabetes onset among children and adults at high risk of developing the disease. The regulatory distinction comes after a June report showing that teplizumab postponed the onset of symptomatic disease by a median of two years compared with placebo in patients who took the drug for 14 days (N. Engl. J. Med. 381, 608–613, 2019). “It’s a very prolonged effect after a single two-week course of the antibody,” says Lucienne Chatenoud, an immunologist from the Necker Hospital for Sick Children in Paris who was not involved in the study. “This is, in view of all clinical diabetologists, a real measure Should a treatment to push back the age of type 1 diabetes onset become available, screening programs of robustness... You are really delaying the to identify children at a markedly elevated risk will be critical. One such European effort is the Global onset of insulin therapy.” Platform for the Prevention of Autoimmune Diabetes, which has undertaken to screen 100,000 Although some researchers maintain newborns for disease-associated variants, including polymorphisms in human leukocyte antigens (HLA) that larger confirmatory trials are still of the DR and DQ isotypes. -

Immusant(1).Pdf
CORPORATE OVERVIEW Developing a new class of targeted tolerizing treatments for autoimmune diseases Immusan-T Corporate Highlights Antigen-specific immunotherapy is considered to be the definitive treatment of autoimmune disease Platform • Discovery and development of tolerizing antigen-specific immunotherapies for auto- Technology immune diseases and beyond • Up-dosing followed by ongoing weekly subcutaneous self administration Proof of Concept • Dosed over 150 celiac patients with Nexvax2 and demonstrated greatly reduced gluten-mediated Demonstrated in immune responses and disease symptoms Celiac Disease • Currently conducting Phase 2 clinical program, Fast track designation granted Major Unmet • Celiac disease (CeD) represents a >$1B market in US with no approved pharmaceutical treatment Need and Market available Opportunities • Type 1 Diabetes represents a ~$5B market with a CAGR of 5.2% by 2028 in US alone Patent • Robust patent IP estate of >130 granted, pending and licensed patents Protection Corporate • Founded in 2010 History • Major investors: Vatera Healthcare Partners, ARCH Ventures, JDRF T1D Fund 2 Experienced Leadership Team • Founded Immusan-T in 2010 • Over 25 years of experience in healthcare, executive Leslie Williams, BS, RN, MBA management, commercial product development and marketing: Chief Executive Officer & INO Therapeutics, Merck, GSK, DatexOhmeda President • Former President & CEO, Ventaira Pharmaceuticals • Venture Partner, Battelle Ventures • Clinical experience – Critical Care, Duke University • Inventor of -

Antigen-Targeted Monoclonal Antibody Otelixizumab and C
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2018/10/17/jpet.115.224899.DC1 1521-0103/355/2/199–205$25.00 http://dx.doi.org/10.1124/jpet.115.224899 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 355:199–205, November 2015 Copyright ª 2015 by The American Society for Pharmacology and Experimental Therapeutics Temporal Pharmacokinetic/Pharmacodynamic Interaction between Human CD3« Antigen–Targeted Monoclonal Antibody Otelixizumab and CD3« Binding and Expression in Human Peripheral Blood Mononuclear Cell Static Culture s Kevin R. Page, Enrica Mezzalana, Alexander J. MacDonald, Stefano Zamuner, Giuseppe De Nicolao, and Andre van Maurik GlaxoSmithKline, Stevenage, United Kingdom (K.R.P., A.J.M., S.Z., A.vM.); University of Pavia, Pavia PV, Italy (E.M., G.D.N.) Received April 22, 2015; accepted August 17, 2015 Downloaded from ABSTRACT Otelixizumab is a monoclonal antibody (mAb) directed to human a shorter apparent half-life at low concentration. Correspondingly, CD3«, a protein forming part of the CD3/T-cell receptor (TCR) a rapid, otelixizumab concentration–, and time-dependent re- complex on T lymphocytes. This study investigated the temporal duction in CD3/TCR expression was observed. These combined interaction between varying concentrations of otelixizumab, bind- observations were consistent with the phenomenon known as jpet.aspetjournals.org ing to human CD3 antigen, and expression of CD3/TCR complexes target-mediated drug disposition (TMDD). A mechanistic, mathe- on lymphocytes in vitro, free from the confounding influence of matical pharmacokinetic/pharmacodynamic (PK/PD) model was changing lymphocyte frequencies observed in vivo. -

Clinical Immunology Helen Chapel, Mansel Haeney Siraj Misbah and Neil Snowden
ESSENTIALS OF CLINICAL IMMUNOLOGY HELEN CHAPEL, MANSEL HAENEY SIRAJ MISBAH AND NEIL SNOWDEN 6TH EDITION Available on Learn Smart. Choose Smart. Essentials of Clinical Immunology Helen Chapel MA, MD, FRCP, FRCPath Consultant Immunologist, Reader Department of Clinical Immunology Nuffield Department of Medicine University of Oxford Mansel Haeney MSc, MB ChB, FRCP, FRCPath Consultant Immunologist, Clinical Sciences Building Hope Hospital, Salford Siraj Misbah MSc, FRCP, FRCPath Consultant Clinical Immunologist, Honorary Senior Clinical Lecturer in Immunology Department of Clinical Immunology and University of Oxford John Radcliffe Hospital, Oxford Neil Snowden MB, BChir, FRCP, FRCPath Consultant Rheumatologist and Clinical Immunologist North Manchester General Hospital, Delaunays Road Manchester Sixth Edition This edition first published 2014 © 2014 by John Wiley & Sons, Ltd Registered office: John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offices: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 350 Main Street, Malden, MA 02148-5020, USA For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley. com/wiley-blackwell The right of the author to be identified as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

Antibody Engineering to Develop New Antirheumatic Therapies John D Isaacs
Available online http://arthritis-research.com/content/11/3/225 Review Antibody engineering to develop new antirheumatic therapies John D Isaacs Wilson Horne Immunotherapy Centre and Musculoskeletal Research Group, Institute of Cellular Medicine, Newcastle University, Framlington Place, Newcastle-Upon-Tyne, NE2 4HH, UK Corresponding author: John D Isaacs, [email protected] Published: 19 May 2009 Arthritis Research & Therapy 2009, 11:225 (doi:10.1186/ar2594) This article is online at http://arthritis-research.com/content/11/3/225 © 2009 BioMed Central Ltd Abstract the light chain two distinct domains, where a domain is a There has been a therapeutic revolution in rheumatology over the discrete, folded, functional unit (Figure 2a). The first domain past 15 years, characterised by a move away from oral immuno- in each chain is the V domain, VH and VL on the heavy and suppressive drugs toward parenteral targeted biological therapies. light chains, respectively. The rest of the heavy chain The potency and relative safety of the newer agents has facilitated comprises three (four for IgE) constant domains (CH1 to a more aggressive approach to treatment, with many more patients CH3), whilst the light chains have one constant domain (CL). achieving disease remission. There is even a prevailing sense that There is a flexible peptide segment (the hinge) between the disease ‘cure’ may be a realistic goal in the future. These develop- ments were underpinned by an earlier revolution in molecular CH1 and CH2 domains. biology and protein engineering as well as key advances in our understanding of rheumatoid arthritis pathogenesis. This review will The antibody V region is composed of the VH and VL focus on antibody engineering as the key driver behind our current domains.