Morphine Tolerance and Reward but Not Expression Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment Protocol Copyright © 2018 Kostoff Et Al
Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al PREVENTION AND REVERSAL OF ALZHEIMER'S DISEASE: TREATMENT PROTOCOL by Ronald N. Kostoffa, Alan L. Porterb, Henry. A. Buchtelc (a) Research Affiliate, School of Public Policy, Georgia Institute of Technology, USA (b) Professor Emeritus, School of Public Policy, Georgia Institute of Technology, USA (c) Associate Professor, Department of Psychiatry, University of Michigan, USA KEYWORDS Alzheimer's Disease; Dementia; Text Mining; Literature-Based Discovery; Information Technology; Treatments Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al CITATION TO MONOGRAPH Kostoff RN, Porter AL, Buchtel HA. Prevention and reversal of Alzheimer's disease: treatment protocol. Georgia Institute of Technology. 2018. PDF. https://smartech.gatech.edu/handle/1853/59311 COPYRIGHT AND CREATIVE COMMONS LICENSE COPYRIGHT Copyright © 2018 by Ronald N. Kostoff, Alan L. Porter, Henry A. Buchtel Printed in the United States of America; First Printing, 2018 CREATIVE COMMONS LICENSE This work can be copied and redistributed in any medium or format provided that credit is given to the original author. For more details on the CC BY license, see: http://creativecommons.org/licenses/by/4.0/ This work is licensed under a Creative Commons Attribution 4.0 International License<http://creativecommons.org/licenses/by/4.0/>. DISCLAIMERS The views in this monograph are solely those of the authors, and do not represent the views of the Georgia Institute of Technology or the University of Michigan. This monograph is not intended as a substitute for the medical advice of physicians. The reader should regularly consult a physician in matters relating to his/her health and particularly with respect to any symptoms that may require diagnosis or medical attention. -

Cerebellar Toxicity of Phencyclidine
The Journal of Neuroscience, March 1995, 75(3): 2097-2108 Cerebellar Toxicity of Phencyclidine Riitta N&kki, Jari Koistinaho, Frank Ft. Sharp, and Stephen M. Sagar Department of Neurology, University of California, and Veterans Affairs Medical Center, San Francisco, California 94121 Phencyclidine (PCP), clizocilpine maleate (MK801), and oth- Phencyclidine (PCP), dizocilpine maleate (MK801), and other er NMDA antagonists are toxic to neurons in the posterior NMDA receptor antagonistshave attracted increasing attention cingulate and retrosplenial cortex. To determine if addition- becauseof their therapeutic potential. These drugs have neuro- al neurons are damaged, the distribution of microglial ac- protective properties in animal studies of focal brain ischemia, tivation and 70 kDa heat shock protein (HSP70) induction where excitotoxicity is proposedto be an important mechanism was studied following the administration of PCP and of neuronal cell death (Dalkara et al., 1990; Martinez-Arizala et MK801 to rats. PCP (10-50 mg/kg) induced microglial ac- al., 1990). Moreover, NMDA antagonists decrease neuronal tivation and neuronal HSP70 mRNA and protein expression damage and dysfunction in other pathological conditions, in- in the posterior cingulate and retrosplenial cortex. In ad- cluding hypoglycemia (Nellgard and Wieloch, 1992) and pro- dition, coronal sections of the cerebellar vermis of PCP (50 longed seizures(Church and Lodge, 1990; Faingold et al., 1993). mg/kg) treated rats contained vertical stripes of activated However, NMDA antagonists are toxic to certain neuronal microglial in the molecular layer. In the sagittal plane, the populations in the brain. Olney et al. (1989) demonstratedthat microglial activation occurred in irregularly shaped patch- the noncompetitive NMDA antagonists,PCP, MK801, and ke- es, suggesting damage to Purkinje cells. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Interplay Between Gating and Block of Ligand-Gated Ion Channels
brain sciences Review Interplay between Gating and Block of Ligand-Gated Ion Channels Matthew B. Phillips 1,2, Aparna Nigam 1 and Jon W. Johnson 1,2,* 1 Department of Neuroscience, University of Pittsburgh, Pittsburgh, PA 15260, USA; [email protected] (M.B.P.); [email protected] (A.N.) 2 Center for Neuroscience, University of Pittsburgh, Pittsburgh, PA 15260, USA * Correspondence: [email protected]; Tel.: +1-(412)-624-4295 Received: 27 October 2020; Accepted: 26 November 2020; Published: 1 December 2020 Abstract: Drugs that inhibit ion channel function by binding in the channel and preventing current flow, known as channel blockers, can be used as powerful tools for analysis of channel properties. Channel blockers are used to probe both the sophisticated structure and basic biophysical properties of ion channels. Gating, the mechanism that controls the opening and closing of ion channels, can be profoundly influenced by channel blocking drugs. Channel block and gating are reciprocally connected; gating controls access of channel blockers to their binding sites, and channel-blocking drugs can have profound and diverse effects on the rates of gating transitions and on the stability of channel open and closed states. This review synthesizes knowledge of the inherent intertwining of block and gating of excitatory ligand-gated ion channels, with a focus on the utility of channel blockers as analytic probes of ionotropic glutamate receptor channel function. Keywords: ligand-gated ion channel; channel block; channel gating; nicotinic acetylcholine receptor; ionotropic glutamate receptor; AMPA receptor; kainate receptor; NMDA receptor 1. Introduction Neuronal information processing depends on the distribution and properties of the ion channels found in neuronal membranes. -

From NMDA Receptor Hypofunction to the Dopamine Hypothesis of Schizophrenia J
REVIEW The Neuropsychopharmacology of Phencyclidine: From NMDA Receptor Hypofunction to the Dopamine Hypothesis of Schizophrenia J. David Jentsch, Ph.D., and Robert H. Roth, Ph.D. Administration of noncompetitive NMDA/glutamate effects of these drugs are discussed, especially with regard to receptor antagonists, such as phencyclidine (PCP) and differing profiles following single-dose and long-term ketamine, to humans induces a broad range of exposure. The neurochemical effects of NMDA receptor schizophrenic-like symptomatology, findings that have antagonist administration are argued to support a contributed to a hypoglutamatergic hypothesis of neurobiological hypothesis of schizophrenia, which includes schizophrenia. Moreover, a history of experimental pathophysiology within several neurotransmitter systems, investigations of the effects of these drugs in animals manifested in behavioral pathology. Future directions for suggests that NMDA receptor antagonists may model some the application of NMDA receptor antagonist models of behavioral symptoms of schizophrenia in nonhuman schizophrenia to preclinical and pathophysiological research subjects. In this review, the usefulness of PCP are offered. [Neuropsychopharmacology 20:201–225, administration as a potential animal model of schizophrenia 1999] © 1999 American College of is considered. To support the contention that NMDA Neuropsychopharmacology. Published by Elsevier receptor antagonist administration represents a viable Science Inc. model of schizophrenia, the behavioral and neurobiological KEY WORDS: Ketamine; Phencyclidine; Psychotomimetic; widely from the administration of purportedly psychot- Memory; Catecholamine; Schizophrenia; Prefrontal cortex; omimetic drugs (Snyder 1988; Javitt and Zukin 1991; Cognition; Dopamine; Glutamate Jentsch et al. 1998a), to perinatal insults (Lipska et al. Biological psychiatric research has seen the develop- 1993; El-Khodor and Boksa 1997; Moore and Grace ment of many putative animal models of schizophrenia. -

Chapter 1—— IBOGAINE: a REVIEW
——Chapter 1—— IBOGAINE: A REVIEW Kenneth R. Alper Departments of Psychiatry and Neurology New York University School of Medicine New York, NY 10016 I. Introduction, Chemical Properties, and Historical Time Line .................................... A. Introduction............................................................................................................ B. Chemical Structure and Properties ........................................................................ C. Historical Time Line.............................................................................................. II. Mechanisms of Action ................................................................................................. A. Neurotransmitter Activities.................................................................................... B. Discrimination Studies........................................................................................... C. Effects on Neuropeptides....................................................................................... D. Possible Effects on Neuroadaptations Related to Drug Sensitization or Tolerance ........................................................................................................... III. Evidence of Efficacy in Animal Models....................................................................... A. Drug Self-Administration ...................................................................................... B. Acute Opioid Withdrawal..................................................................................... -
Cognitive Functions Enhancers Racetams
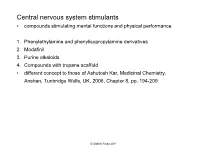
Central nervous system stimulants • compounds stimulating mental functions and physical performance 1. Phenylethylamine and phenylisopropylamine derivatives 2. Modafinil 3. Purine alkaloids 4. Compounds with tropane scaffold ● different concept to those of Ashutosh Kar, Medicinal Chemistry, Anshan, Tunbridge Wells, UK, 2006, Chapter 8, pp. 194-209 © Oldřich Farsa 2011 1. Phenylethylamine and phenylisopropylamine derivatives • natural catecholamines analogues OH H HO N NH R 2 CH HO 3 amphetamine R = H noradrenaline R = CH3 adrenaline Phenylethylamine and phenylisopropylamine derivatives = indirect adrenergics – do not interact directly with adrenergic receptors in the brain but inhibit reuptake of catecholamines or increse their release from synapses; some of them act similarly also in serotoninergic system •centrally stimulating and anorectic effects -OH group in α-position toward the aromatic ring is missing or O is the part of a cycle (morpholine) -OH group on the benzene ring are missing or etherified phenylethylamine moiety can also be a part of a cycle R1 R1 R2 N H 1. Phenylethylamine and phenylisopropylamine derivatives Compounds used as therapeutics H H N H C 2 3 N O (R,S)-1-phenyl-2-aminopropane 2-phenyl-3- amphetamine methylmorpholine phenmethrazine •supression of fatigue, feelings of hunger and thirst, increase of performance •mobilization of energy reserves of organism •indications: narcolepsy, obesity (obsolete) •overdosage: total exhausting, dehydratation, circulation breakdown •see further centrally acting anobesics (anorectics) -

Presence of Methoxetamine in Drug Samples Delivered As Ketamine for Substance Analysis
Is this really ketamine? Presence of methoxetamine in drug samples delivered as ketamine for substance analysis P. Quintana2, Á. Palma1,5, M. Grifell1,2, J. Tirado3,5, C. Gil2, M. Ventura2, I. Fornís3, S. López2, V. Perez1,5, M. Torrens1,3,5, M. Farré3,4,5, L. Galindo1,3,5 1Institut de Neuropsiquiatria i Addiccions, Parc de Salut Mar, Barcelona, Spain 2Asocicación Bienestar y Desarrollo, Energy Control, Barcelona, Spain 3IMIM (Hospital del Mar Medical Research Institute), Barcelona, Spain 4Hospital Germans Trías i Pujol, Servei de Farmacología Clínica, Barcelona, Spain 5Departament de Psiquiatria, Universitat Autònoma de Barcelona, Barcelona, Spain Introduction New psychoactive substances (NPS) are drugs that have recently become available, and are not world-wide regulated. They often intend to mimic the effect of controlled drugs (1), becoming a public health concern. In 2014, 101 new substances were reported for the first time in the EU (2). Methoxetamine, an NPS, is a dissociative hallucinogenic acting as a NMDA receptor antagonist, clinically and pharmacologically similar to Ketamine (3). It differs from ketamine on its higher potency and duration as well as on its possible serotonergic activity, probably leading to more severe side effects. It has been one of the 6 substances requiring risk assessment by EMCDDA during 2014(3), and several case reports have described fatal outcomes related with its use(4). Objective Material and methods The aim of this study was 1) to explore the presence of methoxetamine from the All samples analyzed from January 2010 to March 2015 in which methoxetamine was samples handled to, and analyzed by Energy Control and 2) to determine whether found were studied. -

NPS) Via Online Drugsmarkten
Een studie naar de motieven achter de aankoop van New Psychoactive Substances (NPS) via online drugsmarkten Masterproef neergelegd tot het behalen van de graad van Master in de Criminologische Wetenschappen door (01404422) Noninckx Robi Academiejaar 2017-2018 Promotor : Commissaris : Colman Charlotte Bawin Frédérique INHOUDSOPGAVE Afkortingenlijst ...................................................................................................................... III Woord vooraf .......................................................................................................................... IV DEEL I: INLEIDING EN METHODOLOGIE .................................................................... 1 1.1. Situering van het fenomeen NPS 1 1.2. Probleemstelling 3 1.3. Opzet 4 1.3.1. Doelstelling 4 1.3.2. Onderzoeksvragen 6 1.4. Methodologie 7 1.4.1. Literatuurstudie 7 1.4.2. Kwalitatief luik 10 DEEL II: NEW PSYCHOACTIVE SUBSTANCES........................................................... 17 2.1. Definitie 17 2.2. Categorisering en verschillende soorten NPS 19 2.2.1. Stoffen die niet (meer) toebehoren tot de categorie NPS 19 2.2.2. Stoffen die wel toebehoren tot de categorie NPS 22 2.3. Beleidsmatig en wettelijk kader 35 2.3.1. Internationaal niveau: de Verenigde Naties 35 2.3.2. Regionaal niveau: de Europese Unie 38 2.3.3. Nationaal niveau: het wettelijk en beleidsmatig kader in België 41 DEEL III: DE HANDEL VAN NPS VIA ONLINE DRUGSMARKTEN ........................ 47 3.1. Clearnetmarkets 47 3.2. Darknetmarkets of Cryptomarkets 48 3.3. NPS op online drugsmarkten 51 3.3.1. De handel van NPS op het clearnet 51 3.3.2. De handel van NPS op het darknet 56 I DEEL IV: HET GEBRUIK VAN NPS EN DE NPS-GEBRUIKER ................................. 58 4.1. Het gebruik van NPS in de literatuur 59 4.1.1. De prevalentie van het NPS-gebruik 59 4.1.2. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -

Hallucinogens & Dissociative Drugs
® DRUG FACT SHEET Hallucinogens & Dissociative Drugs Some effects of PCP including depression and memory loss may last six months to a year following prolonged daily use. Class of drug: Hallucinogens (most common form is LSD) Dissociative drugs (most commonly form is PCP) Main active ingredient: Hallucinogens: Lysergic acid diethylamide, mescaline, psilocybin, ibogaine Dissociative: Phencyclidine What it looks like: LSD: Clear, odorless liquid, brightly colored tablets, impregnated blotter paper, thin squares of gelatin PCP: liquid, capsules, white crystalline powder, gum There are hundreds of synthetic hallu - Street names: Lysergic acid diethylamide: LSD, Acid, Blotter, cinogens on the market today including Phencyclidine: PCP, Angel Dust, Loveboat, Wack 25I-NBOMe (N-Bomb) and 2C-I (Smiles) which have been attributed to How it is used: Both hallucinogens and dissociative drugs can be multiple deaths and significant injuries. swallowed, injected or smoked. LSD liquid and gelatin They are generally found as powders, liq - forms can be put in the eyes. PCP is often sprinkled uids, soaked into blotter paper or laced on or sprayed on cigarettes, parsley and marijuana. something edible. Both drugs are classi - fied as Schedule I substances, making Duration of high: Hallucinogens: effects begin within 30 to 90 minutes possession, distribution and manufacture and last from six to twelve hours illegal. PCP: effects begin within minutes and last for hours Withdrawal symptoms: Depression, memory loss U.S. information Effects: Physical (both) —increased heart rate and blood pressure, elevated body temperature, loss of In 2014, nearly 1.3 million appetite, loss of muscle coordination, slurred speech Americans aged 12 and older Hallucinogens reported using LSD in the past Mental —hallucinations; intensified senses; distortion year and 90,000 reported using of time, reality and environment; confusion; mood PCP in the past year. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209