Balsall Common and Meriden Group Practice Scheduled Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Balsall Common Transport Study Baseline and Constraints Report October 2020 Mott Macdonald 35 Newhall Street Birmingham B3 3PU United Kingdom
Balsall Common Transport Study Baseline and Constraints Report October 2020 Mott MacDonald 35 Newhall Street Birmingham B3 3PU United Kingdom T +44 (0)121 234 1500 mottmac.com Solihull Metropolitan Borough Council Council House Balsall Common Transport Manor Square Solihull Study B91 3QB Baseline & Constraints Report October 2020 Mott MacDonald Limited. Registered in England and Wales no. 1243967. Registered office: Mott MacDonald House, 8-10 Sydenham Road, Croydon CR0 2EE, United Kingdom Mott MacDonald | Balsall Common Transport Study Baseline & Constraints Report Issue and Revision Record Revision Date Originator Checker Approver Description A May 2017 Will Oliver Paresh Draft to Client Hodgson Hague Shingadia Rev A Alex Paul Clewett Ellingham B July 2018 Will Oliver Paresh Draft to Client Hodgson Hague Shingadia Rev B Alex Paul Clewett Ellingham C September 2020 Emily Oliver Tony Draft to Client Callard Hague Sheach Rev C. Weller Updated with Fred Jones local plan allocations D October 2020 Emily Oliver Tony Final to Client Callard – Hague Sheach following Weller client comments Document reference: 415790 | 001 | D 415790-MMD-BCTS-CC-TN-TP-001 Information class: Standard This document is issued for the party which commissioned it and for specific purposes connected with the above- captioned project only. It should not be relied upon by any other party or used for any other purpose. We accept no responsibility for the consequences of this document being relied upon by any other party, or being used for any other purpose, or containing any error or omission which is due to an error or omission in data supplied to us by other parties. -

10 Meadow Rise, Balsall Common Cv7 7Rt Asking Price of £439,950
10 MEADOW RISE, BALSALL COMMON CV7 7RT ASKING PRICE OF £439,950 Three Storey Property New Central Heating System Large Workroom/Utility Four Bedrooms New High Gloss Kitchen Garage/Store Completely Refurbished Open Plan Living/Dining Room Excellent Location PROPERTY OVERVIEW Conveniently located opposite Lavender Hall Park, this stunning three storey property has been completely refurbished and updated throughout to include new central heating system, new high gloss breakfast kitchen with quartz worksurface and breakfast bar, three luxury bathrooms all with power showers, newly installed driveway and landscaped rear garden and new carpets throughout. In addition, the property has been internally remodelled to provide a large utility / work room and garage / store. Briefly the property affords:- entrance hallway, luxury guest cloaks with shower, stunning breakfast kitchen with Juliet balcony, three bedrooms to the second floor (master with luxury en-suite), bed four / study to ground floor, open plan living / dining, utility / work room, garage / store and landscaped rear garden with paved patio area. PROPERTY LOCATION Balsall Common is a well established village in a rural setting within easy access of Solihull, Coventry and Birmingham, providing excellent access to road, rail and airport links. The village benefits from well regarded primary and secondary schools and local leisure amenities include cricket, tennis and golf clubs. There is a thriving village centre with a wide variety of shops, a supermarket and numerous quality restaurants -

Ashwood Lawns Turnpike Close, Balsall Common CV7 7SD
Ashwood Lawns • An Exclusive Development of Two Executive Four Turnpike Close, Balsall Common Bedroom Detached Homes CV7 7SD • Stunning Breakfast Kitchen/Family Room Purchase Price £549,950 each • 2 En-Suite Facilities & Family Bathroom Freehold • Village Location T: 0121 703 1860 E: [email protected] W: www.johnshepherd.com Balsall Common is a popular village some 7 miles from Solihull centre. The village sits amidst delightful countryside and enjoys excellent local amenities, all of which contribute to a real sense of community. There is outstanding schooling for all age groups, together with a regular bus and train service, both of which afford easy and convenient access to Coventry, Leamington Spa and, of course, Birmingham City Centre. Balsall Common is well placed to benefit from the superb Midland's motorway network and Birmingham International Airport. A development of two detached family homes located in the heart of Balsall common village in a quiet cul de sac of just a few family homes. Each home boasts a number of features including a spacious sitting room with contemporary fire and bay window, a professionally designed contemporary kitchen with granite/silestone worksurfaces, stainless steel appliances and chrome plated mixer taps. Feature flooring from Porcelanosa tiling ranges to kitchen/breakfast area and utility and under floor heating flooring throughout the ground floor. The properties are complete with luxury bathrooms and en-suite's with Porcelanosa tiling, chrome mixer taps and chrome towel rails. The properties have bespoke interior doors throughout and oak staircases. ON THE GROUND FLOOR ENTRANCE HALL GUEST CLOAKROOM LIVING ROOM 16' 6" x 11' 1" (5.03m x 3.40 excl. -

Nissan Figaro 30Th Birthday Party Weekend 2021 All Tours Will Leave from the Venue Hotel Walton Hall Hotel & Spa
Nissan Figaro 30th Birthday Party Weekend 2021 All tours will leave from the Venue Hotel Walton Hall Hotel & Spa STONELEIGH TOUR Schedule Saturday 26th June 2021 09.30 Meet in the Hotel Reception 09.45 Depart Hotel and drive to start point (19 Kms) - AGree who will lead the convoy Start Point - 69 St Johns Car ParK, WarwicK, CV34 4NL Tour Route Distance – 75 Kms Route to start point from Hotel Head north-west on Kineton Rd/B4086 towards Jubilee Dr 1.57 km Turn right onto Newbold Rd/B4087Continue to follow B4087 5.82 Km Turn left onto Banbury Rd/B4100Continue to follow Banbury Rd 2.20 Km At the roundabout, take the 2nd exit onto Banbury Rd/A425 3.37 km Turn right 225 m 69 St Johns Ct, WarwicK CV34 4NL, UK THIS IS WHERE THE TOUR STARTS The Stoneleigh tour starts from St Nicholas’ Park in Warwick and takes you through the historic town and the north of Royal Leamington Spa. It then leads you through the rolling countryside and picturesque villages of central Warwickshire and the market town of Southam before heading north to take in Stoneleigh and Kenilworth. It returns via Honiley and the craft and antiques centre at Hatton Country World – before bringing you back past the Racecourse into Warwick. The historic town of Warwick is well worth exploring. Here you can browse antique, china and gift shops and visit a number of museums. For refreshment there are some good pubs, fine restaurants and tearooms in the town. Leaving the car park at St Nicholas’ Park in Warwick, turn right onto the A425 signed Birmingham. -

Balsall Common and Hampton-In-Arden HS2 London-West Midlands May 2013
PHASE ONE DRAFT ENVIRONMENTAL STATEMENT Community Forum Area Report 23 | Balsall Common and Hampton-in-Arden HS2 London-West Midlands May 2013 ENGINE FOR GROWTH DRAFT ENVIRONMENTAL STATEMENT Community Forum Area Report ENGINE FOR GROWTH 23 I Balsall Common and Hampton-in-Arden High Speed Two (HS2) Limited, 2nd Floor, Eland House, Bressenden Place, London SW1E 5DU Telephone 020 7944 4908 General email enquiries: [email protected] Website: www.hs2.org.uk © Crown copyright, 2013, except where otherwise stated Copyright in the typographical arrangement rests with the Crown. You may re-use this information (not including logos or third-party material) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit www.nationalarchives.gov.uk/doc/open-government-licence/ or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or e-mail: [email protected]. Where we have identified any third-party copyright information you will need to obtain permission from the copyright holders concerned. To order further copies contact: DfT Publications Tel: 0300 123 1102 Web: www.dft.gov.uk/orderingpublications Product code: ES/13 Printed in Great Britain on paper containing at least 75% recycled fibre. CFA Report – Balsall Common and Hampton-in-Arden/No 23 I Contents Contents Draft Volume 2: Community Forum Area Report – Balsall Common and Hampton-in-Arden/No 23 5 Structure of the HS2 draft Environmental Statement 5 Part A: Introduction 6 1 Introduction 7 -

101 Meeting House Lane Balsall Common | Coventry | Warwickshire | CV7 7GD 101 MEETING HOUSE LANE
101 Meeting House Lane Balsall Common | Coventry | Warwickshire | CV7 7GD 101 MEETING HOUSE LANE As one of four houses built in 1996 by a local builder, this individual family home is located within the Berkswell parish adjoining Balsall Common, a large village between Solihull and Coventry. Ideally located for accessing a wealth of towns and cities, the property enjoys a wonderfully tranquil position with uninterrupted views across the countryside. The current owners, who have lived here for 22 years and have now retired, have enjoyed bringing their family up at number 101 Meeting House Lane. ACCOMMODATION Entering the property, you are immediately greeted within a very spacious and bright hallway. Off the hall to the right are double doors to the main sitting room which has dual aspect views, paragon gas fire with slate hearth and French doors allowing you to open the sitting room up to the garden, great for those summer evenings. The sitting room has interconnecting doors which give access to the snug, which also has a french door opening onto the patio area. Great for entertaining! Also, off the hallway to the left is the dining room which has an outlook to the enclosed private courtyard the front of the property. The dining room flows seamlessly into the breakfast kitchen. This stylish Shaker style kitchen benefits from an array of modern appliances, a Ringmaster Toledo double oven, Domino gas hob, Induction hob, a breakfast table and AMTICO flooring. The AMTICO floor continues into the utility room which also allows you to access the side of the property. -

Balsall Common and Meriden Group Practice
BALSALL COMMON AND MERIDEN GROUP PRACTICE BALSALL COMMON SURGERY Balsall Common Health Centre 1 Ashley Drive Balsall Common CV7 7RW MERIDEN SURGERY Old School House 200 Main Road Meriden CV7 7NG WELCOME TO BALSALL COMMON AND MERIDEN GROUP PRACTICE (this is not a limited partnership) Balsall Common Health Centre Old School House 1 Ashley Drive 200 Main Road Balsall Common Meriden CV7 7RW & CV7 7NG DOCTORS • Dr Bhandal: (Male) MB ChB 1993 Edinburgh MRCGP • Dr Barratt: (Female) MB ChB 1986 Sheffield MRCGP • Dr Carlile: (Female) MB ChB 1984 Glasgow MRCGP DRCOG • Dr Nadeem: (Male) MB BS, MRCS (Ed), MRCGP, DRCOG, DFSRH, DPD • Dr Horsley: (Male) MB ChB 2003 Sheffield MRCGP • Dr Palmer: (Female) MB ChB 2006 Birmingham MRCGP SURGERY OPENING HOURS BALSALL COMMON SURGERY Monday, Tuesday, Wednesday and Friday 8.30am - 6.00pm Thursday 8.30am - 12 noon MERIDEN SURGERY Monday, Tuesday, Thursday and Friday 8.30am - 6.00pm Wednesday 8.30am - 12 noon Reception staff are available to patients either by telephone or in person during these times. When the surgery is closed, a doctor will be on call for emergencies. Emergencies for both surgeries: 01676 935000 REGISTERING WITH THE PRACTICE To register with the practice you should live in the practice area detailed towards the back of this booklet (a more detailed map is available at both surgeries). Visit the Balsall Common or Meriden surgery appropriate to your postal address either in person or register via the Practice web site www.balsallcommongrouppractice.co.uk. Bring with you your medical card. If this is not available, a form will be provided for your completion. -

Balsall Common Cv7 7Ar
THE Grove BALSALL COMMON CV7 7AR Your doorway to style, craftsmanship and luxury living. A boutique development of two 3-bedroom and THE two 4-bedroom detached Grove homes. BALSALL COMMON CV7 7AR PicturesqueLOCATION MEETSwhere COMFORT luxury Perfeclty positioned within Balsall Common, each individually designed home at The Grove offers a rare opportunity to enjoy modern luxury living in the heart of Warwickshire countryside. Set back from the road and accessed by a quiet lane, this boutique development is the perfect location for those wanting quick access to restaurants, shopping, historical landmarks and schools, whilst enjoying a serene countryside setting. STR H A OL T Y HE F A O D R R D D R D K E N BALSALL COVENTRY I L SOLIHULL W COMMON O R T 2 H 4 R M D K KNOWLE EN PA S HW Y BURTON The Grove is ideally situated near up-market GREEN D R D N DORRIDGE E towns within Warwickshire and offers convenient R E E M STONELEIGH MEER END connections for commuters travelling to the CBD’s of D R KENILWORTH Y E London and Birmingham. L WROXALL I N O S H S LAPWORTH A P Y B K BEAUSALE IC M W 40 R A W Kenilworth Coventry Birmingham 5.1 miles 8.9 miles 17 miles B S IR S MING PA H BY A K ROYAL HENLEY- M IC RD W AR IN-ARDEN W LEAMINGTON SPA Knowle Solihull Leamington Spa London CLAVERDON 3.4 miles 7.5 miles 10.5 miles 106 miles WARWICKN VO A R E V I R M WOOTTON 4 WAWEN 0 MODERN DESIGN BUILT FOR Living SIGNATURE SPECIFICATION Each beautiful home at The Grove exemplifies the Mackenzie Miller Homes signature specification. -

Camp Hill House BEAUSALE, WARWICK, WARWICKSHIRE Camp Hill House BEAUSALE, WARWICK, WARWICKSHIRE
Camp Hill House BEAUSALE, WARWICK, WARWICKSHIRE Camp Hill House BEAUSALE, WARWICK, WARWICKSHIRE Approximate distances: Kenilworth 5 miles, Warwick 5 miles, Warwick Parkway Station 4 miles, Balsall Common 5 miles, Berkswell Station 6 miles, Royal Leamington Spa 8 miles, Coventry 12 miles, Stratford-upon-Avon 12 miles, Birmingham International 12 miles Extensive period living with land and income stream LOT 1: CAMP HILL HOUSE Reception hall, drawing room, dining room, sitting room, study, kitchen and breakfast room, utility room, pantry, cloakroom, cellar, six principal bedrooms, three bath/shower rooms (1 en suite), two secondary attic bedrooms, two dressing rooms, games room and box room. Range of outbuildings including extensive garage block with triple garage and double open garage. Extensive off-road parking. Stores. Landscaped and well-tended gardens and grounds. Historic moat. In all about 1.5 acres. LOT 2: THE GRANARY CAMP HILL Separate three-bedroom barn conversion with garden and double garage. LOT 3: THE COTTAGE CAMP HILL Separate two-bedroom cottage with garden and double garage. LOT 4: LAND Pasture of about 4.1 acres. Total land area about 6 acres. For sale as a whole or in 4 lots. SAVILLS BANBURY 36 South Bar, Banbury, Oxfordshire, OX16 9AE 01295 228 000 Nick Rudge [email protected] Your attention is drawn to the Important Notice on the last page of the text SITUATION Camp Hill House is situated in a sought after rural area with views over undulating Warwickshire countryside. Within close proximity to the excellent transport links provided by Warwick Parkway Station, Berkswell Station and the M40. -
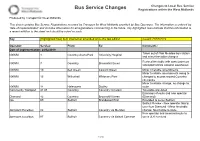
Bus Service Changes Registrations Within the West Midlands
Changes to Local Bus Service Bus Service Changes Registrations within the West Midlands Produced by Transport for West Midlands This sheet contains Bus Service Registrations received by Transport for West Midlands provided by Bus Operators. The information is ordered by 'date of implementation' and includes information for all registrations commencing in the future. Any highlighted rows indicate that this information is a recent addition to the sheet and should be noted as such. Key [Highlighted Row] Item inserted or amended since the last edition Issued: 27/02/2019 Operator: Service: From: To: Comments: Date of implementation: 24/02/2019 Taken out of Pool Meadow bus station NXWM 4 Coventry Arena Park University Hospital and minor timetable changes Revised timetable with some journeys NXWM 7 Coventry Brownshill Green extended to/from Amazon warehouse NXWM 10 Bell Green Eastern Green Minor timetable amendments Minor timetable amendments owing to NXWM 13 Willenhall Whitmore Park changes to access around Coventry city centre Minor timetable change, no change to NXWM 14 Halesowen Dudley route Community Transport 41 47 Coventry Coventry Circulars Timetable amended Extension of route and new operator Diamond 42 Coventry Brownshill Green (Diamond) iGo 69 Solihull Brandwood End Extended to serve Solihull Solihull Review - New operator taking over from Diamond - Minor timetable Johnsons Excelbus 82 Solihull Coventry via Meriden change. No change to route. New operator and amended route to Johnsons Excelbus 87 Solihull Coventry via Balsall Common serve JLR Fen End 1 of 4 Changes to Local Bus Service Bus Service Changes Registrations within the West Midlands New operator and split into two routes, one along existing 87 route and one along existing 88 route. -

Care Home List
Care Home List Age UK Solihull The Core Central Solihull Library Building Solihull B91 3RG Tel: 0121 704 7840 www.ageuksolihull.org.uk E-mail: [email protected] Updated June 2021 Age UK Solihull does not make recommendations and take no responsibility for the information contained in this list or the care received at individual homes. This list is updated regularly. Please read information on the final page of this list. Name and Address Contact Facility Information Client Group Alexandra House 0121 245 1081 ‘Not for profit’ Older People Hillborough Road www.sjmt.org.uk Sir Josiah Mason’s Trust Early Onset Dementia Solihull Total: 36 Care West Midlands Respite if vacancies allow B27 6PF Birchmere House 01564 732 400 Private Care Home Older People 1270 Warwick Road 68 Beds including couples Residential, Nursing and Knowle www.averyhealthcare.co.uk/care-homes/west- suites Respite Care Solihull midlands/solihull/birchmere B93 9LQ Birchmere Mews 01564 732 660 Private Care Home Older People 1270A Warwick Road 63 Beds including couples Providing Residential, Knowle www.averyhealthcare.co.uk/care-homes/west- suites Dementia and Respite Solihull midlands/solihull/birchmere Care B93 9LQ BUPA Ardenlea 0121 705 9222 Private Care Home Older people Grove Total Beds: 60 Care Home with Nursing 19-21 Lode Lane www.bupa.co.uk Dementia - 18 Physical Disability Solihull Dementia care West Midlands, B91 Respite if vacancies allow 2AB BUPA Ardenlea 0121 711 7773 Private Care Home Older people Court Nursing Total Beds: 55 Care Home with Nursing Home -

112 Kelsey Lane Balsall Common | Warwickshire | CV7 7GT
112 Kelsey Lane Balsall Common | Warwickshire | CV7 7GT 112 Kelsey Lane Cover.indd 3 14/02/2019 17:08 112 KELSEY LANE 112 Kelsey Lane Cover.indd 4 14/02/2019 17:08 112 Kelsey Lane Pages.indd 1 14/02/2019 17:07 112 Kelsey Lane Pages.indd 2 14/02/2019 17:07 This stunning five-bedroom property, offers versatile accommodation in the very popular location of Balsall Common, 112 Kelsey Lane is situated on the outskirts of Coventry and is less than 8 miles from Solihull. Deceptively spacious, this home is well proportioned and makes a perfect family home. The accommodation ranges over an impressive 3002 square feet in total it consists of a sitting room, dining room, home study, breakfast kitchen, utility room, work shop, art studio, conservatory, five double bedrooms, three with ensuite, single bedroom and a family bathroom. Overall the property has huge potential and is well worth viewing. The property also benefits from having solar panels installed which currently generates an income in excess of £1700 per year. Entering the property through the storm porch then through the front door into the hallway, you are immediately greeted with a large and spacious hallway boasting solid wooden flooring. Off the hallway to the left, through double doors is the main sitting room, benefiting from a huge bay window which allows a flood of light to fill the room. This room also boasts a feature fire place with gas fire. The sitting room gives access to a home study through double doors that then leads through to the conservatory.