Pramipexole Dihydrochloride) Tablets, for Oral Use None (4) Initial U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -
Pramipexole V2.1 Last Reviewed: 22/04/2021 Review Date: 22/04/2024
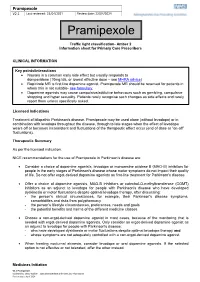
Pramipexole V2.1 Last reviewed: 22/04/2021 Review date: 22/04/2024 Pramipexole Traffic light classification- Amber 2 Information sheet for Primary Care Prescribers CLINICAL INFORMATION Key points/interactions Nausea is a common early side effect but usually responds to domperidone (10mg tds, or lowest effective dose – see MHRA advice) Ropinirole MR is first line dopamine agonist. Pramipexole MR should be reserved for patients in whom this is not suitable- see formulary. Dopamine agonists may cause compulsive/addictive behaviours such as gambling, compulsive shopping and hyper sexuality. Patients rarely recognise such changes as side effects and rarely report them unless specifically asked. Licensed Indications Treatment of idiopathic Parkinson's disease. Pramipexole may be used alone (without levodopa) or in combination with levodopa throughout the disease, through to late stages when the effect of levodopa wears off or becomes inconsistent and fluctuations of the therapeutic effect occur (end of dose or “on-off” fluctuations). Therapeutic Summary As per the licensed indication. NICE recommendations for the use of Pramipexole in Parkinson’s disease are: Consider a choice of dopamine agonists, levodopa or monoamine oxidase B (MAO-B) inhibitors for people in the early stages of Parkinson's disease whose motor symptoms do not impact their quality of life. Do not offer ergot-derived dopamine agonists as first-line treatment for Parkinson's disease. Offer a choice of dopamine agonists, MAO-B inhibitors or catechol-O-methyltransferase (COMT) -

List Item Pramipexole Teva
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Pramipexole Teva 0.088 mg tablets Pramipexole Teva 0.18 mg tablets Pramipexole Teva 0.35 mg tablets Pramipexole Teva 0.7 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Pramipexole Teva 0.088 mg tablets Each tablet contains 0.125 mg pramipexole dihydrochloride monohydrate equivalent to 0.088 mg pramipexole. Pramipexole Teva 0.18 mg tablets Each tablet contains 0.25 mg pramipexole dihydrochloride monohydrate equivalent to 0.18 mg pramipexole. Pramipexole Teva 0.35 mg tablets Each tablet contains 0.5 mg pramipexole dihydrochloride monohydrate equivalent to 0.35 mg pramipexole. Pramipexole Teva 0.7 mg tablets Each tablet contains 1.0 mg pramipexole dihydrochloride monohydrate equivalent to 0.7 mg pramipexole. Please note: Pramipexole doses as published in the literature refer to the salt form. Therefore, doses will be expressed in terms of both pramipexole base and pramipexole salt (in brackets). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet Pramipexole Teva 0.088 mg tablets White, round, flat face bevel edge tablet, 5.55 mm diameter, embossed with “93” on one side and “P1” on the other side. Pramipexole Teva 0.18 mg tablets White, round, flat face bevel edge tablet, 7.00 mm diameter, embossed with "P2" over "P2" on the scored side and "93" on the other side. The tablet can be divided into equal halves. Pramipexole Teva 0.35 mg tablets White to off-white, oval, biconvex tablets, engraved with 9 vertical scoreline 3 on the scored side, and 8023 on the other side. -
Effects of Ketamine and Ketamine Metabolites on Evoked Striatal Dopamine Release, Dopamine Receptors, and Monoamine Transporters
1521-0103/359/1/159–170$25.00 http://dx.doi.org/10.1124/jpet.116.235838 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 359:159–170, October 2016 U.S. Government work not protected by U.S. copyright Effects of Ketamine and Ketamine Metabolites on Evoked Striatal Dopamine Release, Dopamine Receptors, and Monoamine Transporters Adem Can,1 Panos Zanos,1 Ruin Moaddel, Hye Jin Kang, Katinia S. S. Dossou, Irving W. Wainer, Joseph F. Cheer, Douglas O. Frost, Xi-Ping Huang, and Todd D. Gould Department of Psychiatry (A.C., P.Z., J.F.C., D.O.F., T.D.G.), Department of Pharmacology (D.O.F, T.D.G), and Department of Anatomy and Neurobiology (J.F.C, T.D.G), University of Maryland School of Medicine, Baltimore, Maryland; Department of Psychology, Notre Dame of Maryland University, Baltimore, Maryland (A.C.); Biomedical Research Center, National Institute on Aging, National Institutes of Health, Baltimore, Maryland (R.M., K.S.S.D., I.W.W.); National Institute of Mental Health Psychoactive Drug Screening Program, Department of Pharmacology, University of North Carolina Chapel Hill Medical School, Chapel Hill, North Carolina (H.J.K., X.-P.H.); and Mitchell Woods Pharmaceuticals, Shelton, Connecticut (I.W.W.) Received June 14, 2016; accepted July 27, 2016 ABSTRACT Following administration at subanesthetic doses, (R,S)-ketamine mesolimbic DA release and decay using fast-scan cyclic (ketamine) induces rapid and robust relief from symptoms of voltammetry following acute administration of subanesthetic depression in treatment-refractory depressed patients. Previous doses of ketamine (2, 10, and 50 mg/kg, i.p.). -

Sustained Administration of Pramipexole Modifies the Spontaneous Firing of Dopamine, Norepinephrine, and Serotonin Neurons in the Rat Brain
Neuropsychopharmacology (2009) 34, 651–661 & 2009 Nature Publishing Group All rights reserved 0893-133X/09 $32.00 www.neuropsychopharmacology.org Sustained Administration of Pramipexole Modifies the Spontaneous Firing of Dopamine, Norepinephrine, and Serotonin Neurons in the Rat Brain ,1 1 1,2 O Chernoloz* , M El Mansari and P Blier 1 2 Institute of Mental Health Research, University of Ottawa, Ottawa, Ontario, Canada; Department of Cellular and Molecular Medicine, University of Ottawa, Ontario, Canada Pramipexole (PPX) is a D2/D3 receptor agonist that has been shown to be effective in the treatment of depression. Serotonin (5-HT), norepinephrine (NE) and dopamine (DA) systems are known to be involved in the pathophysiology and treatment of depression. Due to reciprocal interactions between these neuronal systems, drugs selectively targeting one system-specific receptor can indirectly modify the firing activity of neurons that contribute to firing patterns in systems that operate via different neurotransmitters. It was thus hypothesized that PPX would alter the firing rate of DA, NE and 5-HT neurons. To test this hypothesis, electrophysiological experiments were carried out in anesthetized rats. Subcutaneously implanted osmotic minipumps delivered PPX at a dose of 1 mg/kg per day for 2 or 14 days. After a 2-day treatment with PPX the spontaneous neuronal firing of DA neurons was decreased by 40%, NE neuronal firing by 33% and the firing rate of 5-HT neurons remained unaltered. After 14 days of PPX treatment, the firing rate of DA had recovered as well as that of NE, whereas the firing rate of 5-HT neurons was increased by 38%. -

DRUG TREATMENTS for Parkinson's
DRUG TREATMENTS FOR Parkinson’s 1 There is no cure yet for Parkinson’s but there are The content in this booklet is designed to be dipped in and out many different drugs that can of – don’t feel like you need to help manage the symptoms. read everything in one go. This is particularly true because what This booklet is for people works for you when starting with Parkinson’s and their treatment for Parkinson’s may family, friends and carers. change later on. It provides information Reading the bits of this about the drugs most information that you need will commonly used to help also make this booklet more manage the condition. manageable and relevant for you. This booklet starts with some key practical points about the drugs used for treating Parkinson’s, then gives further details about categories of drugs and individual drugs. There is also a summary that gives an overview list of Parkinson’s drugs. Choosing the right medication is always a decision you should make with your specialist or Parkinson’s nurse. You can show this booklet to your specialist or Parkinson’s nurse and ask them questions about the information here. You may also find it a useful starting point when you are talking about the next steps in your treatment. Contents Section 1 This gives an overview of Parkinson’s medication and is recommended for anyone with the condition. Parkinson’s drugs: an introduction .........................................................6 This includes how drugs work, their names and what treatment to take. Other ways to manage your Parkinson’s .............................................9 This includes exercise and therapies. -

Drug Information Quarterly
Whiskey & Taylor Pramipexole in treatment of depression drug information quarterly Psychiatric Bulletin (2004), 28,438^440 EROMONA WHISKEY AND DAVID TAYLOR Pramipexole in unipolar and bipolar depression AIMS AND METHOD RESULTS CLINICAL IMPLICATIONS To review the evidence for this use of There are limited data on the clinical use In view of the fact that the evidence pramipexole in the treatment of of pramipexole in affective disorders. for the use of pramipexole is still unipolar and bipolar depression, a Only two double-blind trials in bipolar limited at the time of writing, its literature search on Embase and depressionandoneinunipolardepression routine clinical use cannot be Medline was conducted in December were retrieved. Most information is in the recommended.The data appear 2003.The search was updated in July form of case reports and open studies. No promising, but further research is 2004.The reference sections of dose-response relationships have been required to determine its role in retrieved papers were searched for established and a wide range of doses has affective disorders. further relevant references. been employed in the reports. The monoamine hypothesis of depression has been the agonists (Maj & Rogoz, 1999; Renard et al,2001).In driving force behind antidepressant drug development for humans, the dopamine agonist bromocriptine has been several decades. The theory holds that lower levels of shown to be as effective as imipramine in the treatment serotonin, noradrenaline and dopamine may be involved of depression (Willner, 1983). For a review of dopamine in in the pathophysiology of depression. The place of sero- depression, see Willner (1995) and Rampello et al (2000). -

A Phase 2A Study to Evaluate the Kappa Opioid Receptor As a Target
Study Title: A Phase 2a Study to Evaluate the Kappa Opioid Receptor As a Target for the Treatment of Mood and Anxiety Spectrum Disorders by Evaluation of Whether CERC-501 Engages Key Neural Circuitry Related to the Hedonic Response Version Date: October 06, 2016 NCT02218736 FAST-MAS KOR Phase 2a Study Protocol Version 6.0 Task Order #: HHSN27100004 Version Date 10/06/16 Contract #: HHSN271201200006I CLINICAL STUDY PROTOCOL Study Title: A Phase 2a Study to Evaluate the Kappa Opioid Receptor As a Target for the Treatment of Mood and Anxiety Spectrum Disorders by Evaluation of Whether CERC-501 Engages Key Neural Circuitry Related to the Hedonic Response Abbreviated Title: FAST-MAS KOR Phase 2a Protocol Version: 6.0 Version Date: October 06, 2016 Contract Title: New Experimental Medicine Studies: Fast-Fail Trials in Mood and Anxiety Spectrum Disorders (FAST-MAS) Contract #: HHSN271201200006I Contractor: Duke University Contract PI: Andrew D. Krystal, M.D., M.S. Professor, Department of Psychiatry and Behavioral Sciences Duke University Medical Center Box 3309 Durham, NC 27710 Task Order #: HHSN27100004 Overall Study PI: Andrew D. Krystal, M.D., M.S. Supported by: National Institute of Mental Health (NIMH) Confidential: This document and its contents are the property of the Duke Clinical Research Institute. The information contained herein is confidential and is to be used only in connection with matters authorized by Duke Clinical Research Institute. No portion of this document is to be disclosed to others without prior written permission of Duke Clinical Research Institute. Page 1 of 75 FAST-MAS KOR Phase 2a Study Protocol Version 6.0 Task Order #: HHSN27100004 Version Date 10/06/16 Contract #: HHSN271201200006I Abbreviated Study Title: FAST-MAS KOR Phase 2a Contract #: HHSN271201200006I Task Order #: HHSN27100004 Coordinating Center [CC]: Duke Clinical Research Institute (DCRI) Data center [DCC]: Duke Clinical Research Institute (DCRI) Phase of Study: Phase 2a Target enrollment: 90 Patients FDA Approval(s) IND No Yes Drug: CERC-501 IND #: 121225 held by Dr. -

Acute Management of In-Patient Parkinson's Disease Patients
NHS Fife Acute Management of Patient’s with Parkinson’s Disease Acute management of in-patient Parkinson’s Disease patients Contents Pages Introduction and Admission advice 2 Nil by Mouth Guidance 3 – 5 Complex therapy advice (Apomorphine, DBS, Duodopa) 6 Surgical peri-operative advice 7 Contacts/Directory 7 Author:- Ewan Tevendale, Nicola Chapman, Lynda Kearney Approved by the Managed Services Drug and Therapeutics Committee August 2017. (Review date August 2019) Page 1 NHS Fife Acute Management of Patient’s with Parkinson’s Disease Introduction Medication is crucial in optimal management of Parkinson’s. If medication is not given this can result in compromised swallow (increasing risk of aspiration), delirium, speech difficulties, immobility and hence more dependence. It can also lead to increased falls in a population at high risk of fractures. At worst they may develop a Neuroleptic Malignant Type Syndrome which can be fatal. People with Parkinson’s are admitted to hospital for numerous reasons. Often these are unrelated to their Parkinson’s but if not managed appropriately on admission this can lead to delayed recovery, delayed discharge and poor outcomes for patients and their families. This document has been devised to provide guidance to staff who are involved in the care of someone with Parkinson’s admitted to hospital for whatever reason should the Parkinson’s Specialist Team be unavailable. (e.g. weekend or out of hours) It should be highlighted that these guidelines provide advice to medical and nursing staff to ensure people with Parkinson’s are managed appropriately on admission i.e. receive some anti- parkinsonian medication until they can be seen by a member of the Parkinson’s Team to provide specialist advice on complex medicines management. -

Dopminergic Treatment of Treatment Refractory Mood Disorders
8/12/2014 Jan Fawcett, M.D. Professor of Psychiatry University of New Mexico School of Medicine Conflicts: More enjoyment than facts … …on Amazon! 1 8/12/2014 ABBREVIATIONS BPD Borderline Personality Disorder DSM-V Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ECT Electroconvulsive therapy MAOI Monoamine oxidase inhibitors MDD Major depressive disorder NGA New generation antidepressants NNT Number needed to treat OCD Obsessive-Compulsive Disorder PPX Pramipexole SNRI Serotonin–norepinephrine reuptake inhibitors SSRI Selective serotonin reuptake inhibitors SUD Substance use disorder TCA Tricyclic antidepressants TRD Treatment-resistant depression VNS Vagus nerve stimulation Failed Remission and High Relapse Rates Are Common in Mood Disorders MAJOR DEPRESSION: STAR*D OUTCOMES: Sequenced Treatment Alternatives to Relieve Depression (STAR*D) was a collaborative study on the treatment of depression, funded by the National Institute of Mental Health Treatment step 1 – citalopram 36.8 % remission Overall Remission Rates steps 1-4 67% Treatment Resistant 33% after four steps of treatment BUT Four Month Recurrence rates step 1-4 40.2%- 71% Recovery rates 67% x 60% = 40.2% “Recovered” at 4 months Recovery: no episode of depression for 6 months; recovery is a more reliable outcome than remission Recurrence: an episode of MDD after six months – assumed to be a “new” episode. 2 8/12/2014 What about Bipolar Depression? Sienaert P., Bipolar Disorder 2013 Response: Best Data Quetiapine- Bipolar Depression 60% response- no follow up recovery data Lithium, lamotrigine, olanzepine, olanzepine + flouxetine combination – less favorable Antidepressants – 25% six week response Zarate et al: Ketamine 79% response same as placebo at 7 days Frye et al: Modafinil remission 44% vs 23%, ES = .47 Goldberg et al (2004): pramipexole (1.7 mg) 67% response vs. -

Behavioral Pharmacology of Dopamine D2 and D3 Receptor Agonists and Antagonists in Rats
Behavioral Pharmacology of Dopamine D2 and D3 Receptor Agonists and Antagonists in Rats. by Gregory T. Collins A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Pharmacology) in The University of Michigan 2008 Doctoral Committee: Professor James H. Woods, Chair Professor Margaret E. Gnegy Professor Shaomeng Wang Assistant Professor Roger K. Sunahara © Gregory T. Collins 2008 DEDICATION This thesis is dedicated to my parents, Thomas and Shirley Collins, without whom none of this would have been possible. Your continual support and encouragement throughout all of my endeavors has meant more than you will ever know. Thank you. ii ACKNOWLEDGMENTS First and foremost, I would like to thank my mentor, James Woods. You have been an exceptional mentor to me; I have learned more than I could have ever hoped. It has been a pleasure to work with someone who is so passionate and knowledgable, someone who has not only continued to challenge me, but has also provided an outstanding environment in which to study behavioral pharmacolgy. I truly feel lucky to have been able to learn from you. Of course, I also have to thank Gail Winger who has been a second mentor to me throughout the years. The support, encouragement, guidance, and patience that the two of you have provided has made for an exceptional experience. Thank you. I would also like to thank my committee, James Woods, Roger Sunahara, Peggy Gnegy and Shaomeng Wang. I am grateful to have been able to work with and learn from all of you over the years. -

Medications for Ataxia Symptoms
NATIONALFA ATAXIAQ FOUNDATION FREQUENTLY ASKED QUESTIONS ABOUT... Medications for Ataxia Symptoms DISCLAIMER: This fact sheet is designed for educational purposes Depression: SSRI’s (Selective serotonin reuptake only and is not intended to serve as medical advice. The information inhibitors), SNRI’s (Selective norepinephrine-serotonin provided here should not be used for diagnosing or treating a health reuptake inhibitors)--classes of drugs for anxiety or problem or disease. It is not a substitute for professional care. All of these depression medications may have serious side effects and should only be used under a doctor’s supervision. NAF makes no representation or promise regarding the Dizziness/Vertigo: Acetazolamide (Diamox), effectiveness of any drug listed below. 4-aminopyridine, Baclofen, Clonazepam, Flunarizine, Gabapentin (Neurontin), Meclizine, Memantine, At this time, the goals of treatment of ataxia are to Ondansetron (Zofran), Scopolamine (eg. Transderm improve the quality of life for the person with ataxia. Scop Patch for motion sickness) For certain types of ataxia, such as ataxia due to Vitamin E deficiency, specific treatment of the underlying Excessive daytime sleepiness: Modafinil (Provigil) or problem may improve the ataxia itself. But for most Armodafinil (Nuvigil) kinds of ataxia, a treatment or cure for the disease is not yet available, so the focus is on identifying symp- Erectile Dysfunction: Cialis, Levitra, Viagra toms related to or caused by the ataxia, and treating those symptoms. Fatigue: Amantadine, Atomoxetine