Paraneoplastic Neuropathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys
SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 5:44-47, 2003 Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys SUMMARY Aim and purpose of the study were: 1) to study and compare unfavorable factors playing role in the development of upper teeth plexitis and upper teeth plexopathy; 2) to study peculiarities of clinical manifestation of upper teeth plexitis and upper teeth plexopathy, and to establish their diagnostic value; 3) to optimize the treatment. The results of examination and treatment of 79 patients with upper teeth plexitis (UTP-is) and 63 patients with upper teeth plexopathy (UTP-ty) are described in the article. Questions of the etiology, pathogenesis and differential diagnosis are discussed, methods of complex medicamental and surgical treatment are presented. Keywords: atypical facial neuralgia, atypical odontalgia, atypical facial pain, vascular toothache. PREFACE Besides the common clinical tests, in order to ana- lyze in detail the etiology and pathogenesis of the afore- Usually the injury of the trigeminal nerve is re- mentioned disease, its clinical manifestation and pecu- lated to the pathology of the teeth neural plexuses. liarities, we performed specific examinations such as According to the literature data, injury of the upper orthopantomography of the infraorbital canals, mea- teeth neural plexuses makes more than 7% of all sured the velocity of blood flow in the infraorbital blood neurostomatologic diseases. Many terms are used in vessels (doplerography), examined the pain threshold literature to characterize the clinical symptoms com- of facial skin and oral mucous membrane in acute pe- plex of the above-mentioned pathology. Some authors riod and remission, and evaluated the role that the state (1, 2, 3) named it dental plexalgia or dental plexitis. -

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Patients and Experiences from the First Danish Flavour Clinic
DANISH MEDICAL JOURNAL Patients and experiences from the first Danish flavour clinic Alexander Fjaeldstad1, 2, 3, Jelena Stankovic2, Mine Onat2, Dovile Stankevice1 & Therese Ovesen1, 2 ABSTRACT duced sense of smell (hyposmia) [1, 2], making olfac INTRODUCTION: Chemosensory dysfunction is common. tory dysfunction a very common disorder. Apart from ORIGINAL ARTICLE Although patients complain of taste loss, the most common these quantitative olfactory disorders, olfactory dis 1) Flavour Clinic, Ear cause of a diminished taste experience is olfactory orders can have a qualitative nature where stimuli are Nose and Throat dysfunction. Department, Holstebro distorted (parosmia) or emerge without apparent stim Regional Hospital, METHODS: Since January 2017, patients with complaints ulation (phantosmia). Around 10% of patients with dis Denmark about smell and/or taste loss have been referred to the torted flavour perception have an actual taste disorder, 2) Flavour Institute, Flavour Clinic by ear, nose and throat (ENT) practitioners. Prior while only a few percent have isolated taste disorders. Department of Clinical to referral, CT, endoscopy of the nasal cavity and allergy Medicine, Aarhus These include loss of taste (ageusia), reduced sense of testing were required. Patients underwent full olfactory and University, Denmark taste (hypogeusia) or distorted sense of taste (parageu 3) Hedonia Research gustatory testing, complete ENT and neurological examination sia). Group, Department of and review of medicine and medical history. Patients also In all cases, the sensory loss can cause a wide range Psychiatry, University of completed different questionnaires such as the Mini Mental Oxford, United Kingdom of complications and consequences for patients. Status Examination, the Sino-Nasal Outcome Test and the Patients often complain of a reduced quality of life due Major Depression Inventory. -

Taste and Smell Disorders in Clinical Neurology
TASTE AND SMELL DISORDERS IN CLINICAL NEUROLOGY OUTLINE A. Anatomy and Physiology of the Taste and Smell System B. Quantifying Chemosensory Disturbances C. Common Neurological and Medical Disorders causing Primary Smell Impairment with Secondary Loss of Food Flavors a. Post Traumatic Anosmia b. Medications (prescribed & over the counter) c. Alcohol Abuse d. Neurodegenerative Disorders e. Multiple Sclerosis f. Migraine g. Chronic Medical Disorders (liver and kidney disease, thyroid deficiency, Diabetes). D. Common Neurological and Medical Disorders Causing a Primary Taste disorder with usually Normal Olfactory Function. a. Medications (prescribed and over the counter), b. Toxins (smoking and Radiation Treatments) c. Chronic medical Disorders ( Liver and Kidney Disease, Hypothyroidism, GERD, Diabetes,) d. Neurological Disorders( Bell’s Palsy, Stroke, MS,) e. Intubation during an emergency or for general anesthesia. E. Abnormal Smells and Tastes (Dysosmia and Dysgeusia): Diagnosis and Treatment F. Morbidity of Smell and Taste Impairment. G. Treatment of Smell and Taste Impairment (Education, Counseling ,Changes in Food Preparation) H. Role of Smell Testing in the Diagnosis of Neurodegenerative Disorders 1 BACKGROUND Disorders of taste and smell play a very important role in many neurological conditions such as; head trauma, facial and trigeminal nerve impairment, and many neurodegenerative disorders such as Alzheimer’s, Parkinson Disorders, Lewy Body Disease and Frontal Temporal Dementia. Impaired smell and taste impairs quality of life such as loss of food enjoyment, weight loss or weight gain, decreased appetite and safety concerns such as inability to smell smoke, gas, spoiled food and one’s body odor. Dysosmia and Dysgeusia are very unpleasant disorders that often accompany smell and taste impairments. -

The Relationship Among Pain, Sensory Loss, and Small Nerve Fibers in Diabetes
Pathophysiology/Complications ORIGINAL ARTICLE The Relationship Among Pain, Sensory Loss, and Small Nerve Fibers in Diabetes 1,2 LEA SORENSEN, RN, BHSC ing our own, have shown this not to be 1 LYNDA MOLYNEAUX, RN the case (9–11). However, in view of the 1,2 DENNIS K. YUE, MD, PHD, FRACP pivotal role played by small nerve fibers in the transmission of pain sensation, fur- ther studies are obviously of importance. OBJECTIVE — Many individuals with diabetes experience neuropathic pain, often without Direct examination of intraepidermal objective signs of large-fiber neuropathy. We examined intraepidermal nerve fibers (IENFs) to nerve fibers (IENF) using skin biopsy evaluate the role of small nerve fibers in the genesis of neuropathic pain. technique is a proven procedure to iden- tify small-fiber abnormalities. Several RESEARCH DESIGN AND METHODS — Twenty-five diabetic subjects with neuro- studies using this technique have shown pathic pain and 13 without were studied. The pain was present for at least 6 months for which the density of IENF to be reduced in id- no other cause could be found. Punch skin biopsies were obtained from the distal leg. IENFs were stained using antibody to protein gene product 9.5 and counted with confocal microscopy. iopathic and nondiabetic neuropathies Neuropathy was graded by vibration perception and cold detection thresholds and the Michigan (12–14). This technique has also shown Neuropathy Screening Instrument. that people with diabetes have reduced IENF and altered nerve morphology RESULTS — In the total cohort, IENF density was significantly lower in those with pain (14,15). However, to our knowledge, no compared with those without (3 [1–6] vs. -

Understanding Perceptions of Variation in Sensory Experience
What do people know about the senses? Understanding perceptions of variation in sensory experience Christine Cuskley*1 and Charalampos Saitis2 1Linguistics and Centre for Behaviour and Evolution, Newcastle University, Newcastle Upon Tyne, UK 2Centre for Digital Music, Queen Mary University London, London, UK *Corresponding author: [email protected] Abstract: Academic disciplines spanning cognitive science, art, and music have made strides in understanding how humans sense and experience the world. We now have a better scientific understanding of how human sensation and perception function both in the brain and in interaction than ever before. However, there is little research on how this high level scientific understanding is translated into knowledge for the public more widely. We present descriptive results from a simple survey and compare how public understanding and perception of sensory experience lines up with scientific understanding. Results show that even in a sample with fairly high educational attainment, many respondents were unaware of fairly common forms of sensory variation. In line with the well- documented under representation of sign languages within linguistics, respondents tended to under- estimate the number of sign languages in the world. We outline how our results represent gaps in public understanding of sensory variation, and argue that filling these gaps can form an important early intervention, acting as a basic foundation for improving acceptance, inclusivity, and accessibility for cognitively diverse populations. Introduction Our senses form our window into the world. Understanding human sensory experience, and how it supports uniquely human endeavours like music and language, is key to a better understanding of what it means to be human. -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

New Insights in Lumbosacral Plexopathy
New Insights in Lumbosacral Plexopathy Kerry H. Levin, MD Gérard Said, MD, FRCP P. James B. Dyck, MD Suraj A. Muley, MD Kurt A. Jaeckle, MD 2006 COURSE C AANEM 53rd Annual Meeting Washington, DC Copyright © October 2006 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 PRINTED BY JOHNSON PRINTING COMPANY, INC. C-ii New Insights in Lumbosacral Plexopathy Faculty Kerry H. Levin, MD P. James. B. Dyck, MD Vice-Chairman Associate Professor Department of Neurology Department of Neurology Head Mayo Clinic Section of Neuromuscular Disease/Electromyography Rochester, Minnesota Cleveland Clinic Dr. Dyck received his medical degree from the University of Minnesota Cleveland, Ohio School of Medicine, performed an internship at Virginia Mason Hospital Dr. Levin received his bachelor of arts degree and his medical degree from in Seattle, Washington, and a residency at Barnes Hospital and Washington Johns Hopkins University in Baltimore, Maryland. He then performed University in Saint Louis, Missouri. He then performed fellowships at a residency in internal medicine at the University of Chicago Hospitals, the Mayo Clinic in peripheral nerve and electromyography. He is cur- where he later became the chief resident in neurology. He is currently Vice- rently Associate Professor of Neurology at the Mayo Clinic. Dr. Dyck is chairman of the Department of Neurology and Head of the Section of a member of several professional societies, including the AANEM, the Neuromuscular Disease/Electromyography at Cleveland Clinic. Dr. Levin American Academy of Neurology, the Peripheral Nerve Society, and the is also a professor of medicine at the Cleveland Clinic College of Medicine American Neurological Association. -
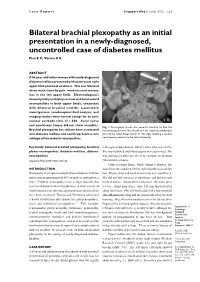
Bilateral Brachial Plexopathy As an Initial Presentation in a Newly-Diagnosed, Uncontrolled Case of Diabetes Mellitus Pica E C, Verma K K
Case Report Singapore Med J 2008; 49(2) : e29 Bilateral brachial plexopathy as an initial presentation in a newly-diagnosed, uncontrolled case of diabetes mellitus Pica E C, Verma K K ABSTRACT A 55-year-old Indian woman with newly-diagnosed diabetes mellitus presented with acute onset right upper limb proximal weakness. This was followed three weeks later by pain, weakness and sensory loss in the left upper limb. Electrodiagnosis showed patchy multiple proximal and distal axonal neuropathies in both upper limbs, consistent with bilateral brachial neuritis. Laboratory investigations, cerebrospinal fluid analysis, and imaging studies were normal except for an anti- nuclear antibody titre of 1:640. Sural nerve and quadriceps biopsy did not show vasculitis. Fig. 1 Photograph shows the patient’s inability to flex the Brachial plexopathy has seldom been associated interphalangeal joint of the thumb and the distal interphalangeal with diabetes mellitus and could represent a rare joint of the index finger (pinch or OK sign) implying a median subtype of the diabetic neuropathies. nerve lesion proximal to the wrist bilaterally. Keywords: bilateral brachial plexopathy, brachial with signs of dehydration. HbA1c at the time was 14.2%. plexus neuropathies, diabetes mellitus, diabetic She was hydrated and blood sugars were optimised. She neuropathies was discharged after one week to continue medication Singapore Med J 2008; 49(2): e29-e32 (Metformin) at home. Upon reaching home, while taking a shower, she INTRODUCTION found that she could not lift her right shoulder to wash her Neuropathy is a frequent complication of diabetes mellitus hair. Elbow, wrist and hand movements were unaffected. -
Accessibility Guide for Sensory Loss
A simple touch leads to endless possibilities Accessibility Guidelines for Sensory Loss 2020 3rd Edition Table of Contents Introduction .............................................................................................................................. 1 DeafBlind Ontario Services .................................................................................................. 2 About the Accessibility Guidelines for Sensory Loss ....................................................... 3 Acknowledgements .............................................................................................................. 3 Copyright ............................................................................................................................. 3 Accessibility Guidelines ....................................................................................................... 3 Quick Design Tips ................................................................................................................ 4 DIY Orientation and Accessibility Enhancements ................................................................ 4 Deafblindness ....................................................................................................................... 5 What is Deafblindness? ....................................................................................................... 5 Deafblindness and Communication ..................................................................................... 5 Types of Deafblindness ...................................................................................................... -

Olfactory Dysfunction in Neurodegenerative Diseases
Eur J Gen Med 2004; 1(3): 1-11 REVIEW ARTICLE OLFACTORY DYSFUNCTION IN NEURODEGENERATIVE DISEASES M. Hakan Özdener, Nancy E. Rawson Monell Chemical Senses Center, University City Science Center Interest in olfactory dysfunction has increased tremendously in the past decade, in part due to observations that chemosensory impairment is an early symptom of many neurodegenerative diseases. Several features of the olfactory system make it particularly relevant to understanding neurodegeneration/regeneration. First, while being vulnerable to environmental and infectious exposure, the olfactory system has the unique property of ongoing replacement of the olfactory sensory neurons under physiological conditions and following injury. Second, the receptor neurons residing in the periphery are developmentally related to the central nervous system, yet are accessible relatively noninvasively via biopsy from living subjects. Third, olfactory performance can easily be tested in a variety of ways that provide insight into the function of brain areas involved in detection, identification and memory. In addition to providing insights into the etiology or diagnosis of disease, a better understanding of olfactory neurobiology is needed to develop ways to treat olfactory dysfunction, which affects both quality of life and personal safety. At least 3,000,000 Americans suffer from chemosensory disorders and that is likely to grow as the aging segment of the population increases. Olfactory impairment represents a danger to the individuals resulting from inability to detect hazards as natural gas and spoiled food and threatens quality of life through the loss of enjoyment of foods and fragrances. The neurological systems responsible for olfactory function represent perhaps the most diverse, complex and adaptable components of the nervous system. -

Paraneoplastic Neurological and Muscular Syndromes
Paraneoplastic neurological and muscular syndromes Short compendium Version 4.5, April 2016 By Finn E. Somnier, M.D., D.Sc. (Med.), copyright ® Department of Autoimmunology and Biomarkers, Statens Serum Institut, Copenhagen, Denmark 30/01/2016, Copyright, Finn E. Somnier, MD., D.S. (Med.) Table of contents PARANEOPLASTIC NEUROLOGICAL SYNDROMES .................................................... 4 DEFINITION, SPECIAL FEATURES, IMMUNE MECHANISMS ................................................................ 4 SHORT INTRODUCTION TO THE IMMUNE SYSTEM .................................................. 7 DIAGNOSTIC STRATEGY ..................................................................................................... 12 THERAPEUTIC CONSIDERATIONS .................................................................................. 18 SYNDROMES OF THE CENTRAL NERVOUS SYSTEM ................................................ 22 MORVAN’S FIBRILLARY CHOREA ................................................................................................ 22 PARANEOPLASTIC CEREBELLAR DEGENERATION (PCD) ...................................................... 24 Anti-Hu syndrome .................................................................................................................. 25 Anti-Yo syndrome ................................................................................................................... 26 Anti-CV2 / CRMP5 syndrome ............................................................................................