Inflammation and Neuropathic Attacks in Hereditary Brachial Plexus Neuropathy C J Klein,Pjbdyck, S M Friedenberg, T M Burns, a J Windebank, P J Dyck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys
SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 5:44-47, 2003 Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys SUMMARY Aim and purpose of the study were: 1) to study and compare unfavorable factors playing role in the development of upper teeth plexitis and upper teeth plexopathy; 2) to study peculiarities of clinical manifestation of upper teeth plexitis and upper teeth plexopathy, and to establish their diagnostic value; 3) to optimize the treatment. The results of examination and treatment of 79 patients with upper teeth plexitis (UTP-is) and 63 patients with upper teeth plexopathy (UTP-ty) are described in the article. Questions of the etiology, pathogenesis and differential diagnosis are discussed, methods of complex medicamental and surgical treatment are presented. Keywords: atypical facial neuralgia, atypical odontalgia, atypical facial pain, vascular toothache. PREFACE Besides the common clinical tests, in order to ana- lyze in detail the etiology and pathogenesis of the afore- Usually the injury of the trigeminal nerve is re- mentioned disease, its clinical manifestation and pecu- lated to the pathology of the teeth neural plexuses. liarities, we performed specific examinations such as According to the literature data, injury of the upper orthopantomography of the infraorbital canals, mea- teeth neural plexuses makes more than 7% of all sured the velocity of blood flow in the infraorbital blood neurostomatologic diseases. Many terms are used in vessels (doplerography), examined the pain threshold literature to characterize the clinical symptoms com- of facial skin and oral mucous membrane in acute pe- plex of the above-mentioned pathology. Some authors riod and remission, and evaluated the role that the state (1, 2, 3) named it dental plexalgia or dental plexitis. -

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Dr Peter Heppner Consultant Neurosurgeon Auckland City Hospital Starship Childrens Hospital Ascot Hospital
Dr Peter Heppner Consultant Neurosurgeon Auckland City Hospital Starship Childrens Hospital Ascot Hospital 14:00 - 14:55 WS #55: Case Studies on Managing Cervical Radiculopathy 15:05 - 16:00 WS #67: Case Studies on Managing Cervical Radiculopathy (Repeated) Case Studies on Managing Cervical Radiculopathy: Peter Heppner Neurosurgeon Auckland City Hospital Starship Childrens Hospital Ascot Private Hospital www.neurosurgeon.org.nz DISCLOSURES I have no actual or potential conflict of interest in relation to this presentation WHAT ARE THE TAKE HOME POINTS? Evidence relating to cervical radiculopathy management is poor Natural history is generally very good In the absence of red flags, initial management with analgesia and physiotherapy appropriate NRIs can be a useful therapeutic and diagnostic tool Surgery ideally considered between 3-6 months from onset Either anterior or posterior surgical approaches can be selected depending on specifics of the case CASE 1 58 yr old lady 2 weeks radiating left arm pain (?after pilates) Taking paracetamol and NSAID Mild parasthesia in thumb Neuro exam normal Neck Disability Index 28% (mild) Clinically: Mild C6 radiculopathy of short duration CERVICAL RADICULOPATHY Radiating arm pain in a nerve distribution due to mechanical compression/chemical irritation of the nerve root Referred pain to inter-scapular and lateral neck common Weakness usually mild Pain or parasthesia non-dermatomal in almost half of patients Reduced reflex best predictor of imaging findings>motor weakness>sensory -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

Carpal Tunnel Syndrome: a Review of the Recent Literature I
The Open Orthopaedics Journal, 2012, 6, (Suppl 1: M8) 69-76 69 Open Access Carpal Tunnel Syndrome: A Review of the Recent Literature I. Ibrahim*,1, W.S. Khan1, N. Goddard2 and P. Smitham1 1University College London Institute of Orthopaedics and Musculoskeletal Sciences, Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, HA7 4LP, UK 2 Department of Trauma & Orthopaedics, Royal Free Hospital, Pond Street, London, NW3 2QG, UK Abstract: Carpal Tunnel Syndrome (CTS) remains a puzzling and disabling condition present in 3.8% of the general population. CTS is the most well-known and frequent form of median nerve entrapment, and accounts for 90% of all entrapment neuropathies. This review aims to provide an overview of this common condition, with an emphasis on the pathophysiology involved in CTS. The clinical presentation and risk factors associated with CTS are discussed in this paper. Also, the various methods of diagnosis are explored; including nerve conduction studies, ultrasound, and magnetic resonance imaging. Keywords: Carpal tunnel syndrome, median nerve, entrapment neuropathy, pathophysiology, diagnosis. WHAT IS CARPAL TUNNEL SYNDROME? EPIDEMIOLOGY First described by Paget in 1854 [1], Carpal Tunnel CTS is the most frequent entrapment neuropathy [2], Syndrome (CTS) remains a puzzling and disabling condition believed to be present in 3.8% of the general population [14]. 1 commonly presented to Rheumatologists and Orthopaedic in every 5 subjects who complains of symptoms such as pain, Hand clinicians. It is a compressive neuropathy, which is numbness and a tingling sensation in the hands is expected to defined as a mononeuropathy or radiculopathy caused by have CTS based on clinical examination and electrophysio- mechanical distortion produced by a compressive force [2]. -

New Insights in Lumbosacral Plexopathy
New Insights in Lumbosacral Plexopathy Kerry H. Levin, MD Gérard Said, MD, FRCP P. James B. Dyck, MD Suraj A. Muley, MD Kurt A. Jaeckle, MD 2006 COURSE C AANEM 53rd Annual Meeting Washington, DC Copyright © October 2006 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 PRINTED BY JOHNSON PRINTING COMPANY, INC. C-ii New Insights in Lumbosacral Plexopathy Faculty Kerry H. Levin, MD P. James. B. Dyck, MD Vice-Chairman Associate Professor Department of Neurology Department of Neurology Head Mayo Clinic Section of Neuromuscular Disease/Electromyography Rochester, Minnesota Cleveland Clinic Dr. Dyck received his medical degree from the University of Minnesota Cleveland, Ohio School of Medicine, performed an internship at Virginia Mason Hospital Dr. Levin received his bachelor of arts degree and his medical degree from in Seattle, Washington, and a residency at Barnes Hospital and Washington Johns Hopkins University in Baltimore, Maryland. He then performed University in Saint Louis, Missouri. He then performed fellowships at a residency in internal medicine at the University of Chicago Hospitals, the Mayo Clinic in peripheral nerve and electromyography. He is cur- where he later became the chief resident in neurology. He is currently Vice- rently Associate Professor of Neurology at the Mayo Clinic. Dr. Dyck is chairman of the Department of Neurology and Head of the Section of a member of several professional societies, including the AANEM, the Neuromuscular Disease/Electromyography at Cleveland Clinic. Dr. Levin American Academy of Neurology, the Peripheral Nerve Society, and the is also a professor of medicine at the Cleveland Clinic College of Medicine American Neurological Association. -

A Historical Approach to Hereditary Spastic Paraplegia
r e v u e n e u r o l o g i q u e 1 7 6 ( 2 0 2 0 ) 2 2 5 – 2 3 4 Available online at ScienceDirect www.sciencedirect.com History of Neurology A historical approach to hereditary spastic paraplegia O. Walusinski Private practice, 20, rue de Chartres, 28160 Brou, France i n f o a r t i c l e a b s t r a c t Article history: Hereditary spastic paraplegia (HSP) is a group of rare neurological disorders, characterised Received 12 August 2019 by their extreme heterogeneity in both their clinical manifestations and genetic origins. Received in revised form Although Charles-Prosper Ollivier d’Angers (1796–1845) sketched out a suggestive descrip- 25 November 2019 tion in 1827, it was Heinrich Erb (1840–1921) who described the clinical picture, in 1875, for Accepted 26 November 2019 ‘‘spastic spinal paralysis’’. Jean-Martin Charcot (1825–1893) began teaching the disorder as a Available online 3 January 2020 clinical entity this same year. Adolf von Stru¨mpell (1853–1925) recognised its hereditary nature in 1880 and Maurice Lorrain (1867–1956) gained posthumous fame for adding his Keywords: name to that of Stru¨mpell and forming the eponym after his 1898 thesis, the first review Hereditary spastic paraplegia covering twenty-nine affected families. He benefited from the knowledge accumulated over Weakness a dozen years on this pathology by his teacher, Fulgence Raymond (1844–1910). Here I Motor neuron disease present a history across two centuries, leading to the clinical, anatomopathological, and Neurodegeneration genetic description of hereditary spastic paraplegia which today enables a better unders- Stru¨mpell-Lorrain syndrome tanding of the causative cellular dysfunctions and makes it possible to envisage effective History of neurology treatment. -
101-Carpal Tunnel Syndrome
Focus on CME at the University of Calgary Carpal Tunnel Syndrome The non-idiopathic causes of carpal tunnel syndrome (CTS) involve intrinsic and extrinsic conditions responsible for nerve compression. To establish a work-related association, there should be a history of excessive or unusual hand use of a nature known to be associated with CTS prior to the onset of symptoms. By Ron Gorsché, MD, MMedSc (Occupational Health), CCFP arpal tunnel syndrome (CTS) is responsible about CTS and it is among the most controversial C for the most time lost in the workplace, yet of disorders. This article focuses on how recent lit- there is little consensus regarding work as a erature has contributed to the theories of patho- causative factor of the syndrome. Little is known physiology and pathogenesis of CTS, and pro- vides clinicians with a more scientific approach Dr. Gorsché is clinical associate pro- to causative factors and treatment. fessor, departments of family medi- cine and community health sciences, faculty of medicine, University of Historical Perspectives Calgary, and director, Work-Related In 1860, Paget reported the first cases of median Upper Limb Disorders Research nerve compression of the wrist — one case attrib- Unit, Calgary, Alberta. He is also uted the disorder to a tight band wrapped around active staff, High River General the wrist and the other cited complications asso- Hospital, High River, Alberta. ciated with a fractured distal radius.1 In 1941, The Canadian Journal of CME / October 2001 101 Carpal Tunnel Syndrome Woltman first postulated the possibility of nerve toms of CTS. This approach works well for the compression within the carpal tunnel as a cause of clinician attempting to explain the syndrome to a “median neuritis,” after reporting 12 cases associ- patient, but requires further classification for epi- ated with acromegaly.2 demiological study. -
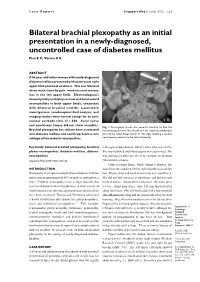
Bilateral Brachial Plexopathy As an Initial Presentation in a Newly-Diagnosed, Uncontrolled Case of Diabetes Mellitus Pica E C, Verma K K
Case Report Singapore Med J 2008; 49(2) : e29 Bilateral brachial plexopathy as an initial presentation in a newly-diagnosed, uncontrolled case of diabetes mellitus Pica E C, Verma K K ABSTRACT A 55-year-old Indian woman with newly-diagnosed diabetes mellitus presented with acute onset right upper limb proximal weakness. This was followed three weeks later by pain, weakness and sensory loss in the left upper limb. Electrodiagnosis showed patchy multiple proximal and distal axonal neuropathies in both upper limbs, consistent with bilateral brachial neuritis. Laboratory investigations, cerebrospinal fluid analysis, and imaging studies were normal except for an anti- nuclear antibody titre of 1:640. Sural nerve and quadriceps biopsy did not show vasculitis. Fig. 1 Photograph shows the patient’s inability to flex the Brachial plexopathy has seldom been associated interphalangeal joint of the thumb and the distal interphalangeal with diabetes mellitus and could represent a rare joint of the index finger (pinch or OK sign) implying a median subtype of the diabetic neuropathies. nerve lesion proximal to the wrist bilaterally. Keywords: bilateral brachial plexopathy, brachial with signs of dehydration. HbA1c at the time was 14.2%. plexus neuropathies, diabetes mellitus, diabetic She was hydrated and blood sugars were optimised. She neuropathies was discharged after one week to continue medication Singapore Med J 2008; 49(2): e29-e32 (Metformin) at home. Upon reaching home, while taking a shower, she INTRODUCTION found that she could not lift her right shoulder to wash her Neuropathy is a frequent complication of diabetes mellitus hair. Elbow, wrist and hand movements were unaffected. -

POLYNEURITIS by G
413 Postgrad Med J: first published as 10.1136/pgmj.35.405.413 on 1 July 1959. Downloaded from POLYNEURITIS By G. S. GRAVESON, M.A., M.D., F.R.C.P. Consultant Neurologist, Wessex Regional Hospital Board (From the Southampton General Hospital) Diseases affecting the lower motor and sensory acid and vitamin B.I2. Thiamine is a constituent neurones, diffusely and usually symmetrically, are of the coenzyme cocarboxylase, which is necessary grouped together under the title polyneuritis. The for the oxidation of pyruvic acid formed in the term is imprecise, for many of these diseases affect metabolism of glucose by nerve cells. It is also structures other than peripheral nerves, e.g. concerned in the synthesis of acetylocholine in spinal nerve cells, roots and muscles, and few of nerve fibres. Its deficiency, therefore, results in them are really inflammatory disorders. To over- neuronal degeneration and the accumulation of an come this inaccuracy, such terms as polyradiculo- excess of pyruvate in the blood. This may be neuropathy and neuromyopathy have been coined present in the fasting state or it may be brought but the older word still serves, with better out by a loading dose of glucose. Joiner, McArdle euphony perhaps, provided it is used merely in and Thompson (1950) describe the use of such aProtected by copyright. the sense of a condition in which lesions of peri- 'pyruvate metabolism test ' in the investigation of pheral nerves occur. Its retention may be ad- cases of polyneuritis. Lack of thiamine may be a visable, too, until such time as the pathogenesis of contributory factor in the polyneuritis of chronic the various types of the disease have been more alcoholism and in those cases which complicate fully elucidated. -

Brachial Plexopathy Following High-Dose Melphalan and Autologous Peripheral Blood Stem Cell Transplantation
Bone Marrow Transplantation (2010) 45, 951–952 & 2010 Macmillan Publishers Limited All rights reserved 0268-3369/10 $32.00 www.nature.com/bmt LETTER TO THE EDITOR Brachial plexopathy following high-dose melphalan and autologous peripheral blood stem cell transplantation Bone Marrow Transplantation (2010) 45, 951–952; Tone and power were normal throughout, lower limb deep doi:10.1038/bmt.2009.243; published online 21 September 2009 tendon reflexes were absent and plantars were downgoing. Magnetic resonance imaging of the whole spine at this point revealed widespread myelomatous involvement of the Neuromuscular pathologies are a recognized complication bony spine but no cord compromise. Thalidomide was of SCT, often occurring as a result of infection or continued with no alteration in dosage. The patient haemorrhage, but also in association with GVHD follow- subsequently underwent a PBSCT with high-dose melpha- ing allogeneic SCT.1 The published literature on post- lan as the conditioning regime. transplant peripheral nervous system pathologies includes Within 14 days of stem-cell infusion the patient devel- descriptions of myasthenia gravis, Guillain-Barre´ oped progressive proximal weakness affecting predomi- syndrome, polymyositis and peripheral neuropathy.2–5 nantly the upper limbs. There was no neck pain or Ocular toxicity, radiculopathy and plexopathy have also involvement of bladder or bowel. Examination revealed rarely been reported. We report three cases of brachial bilateral wrist-drop with grade 3–4 weakness of the small plexopathy occurring after autologous peripheral blood muscles of the hand, elbow flexors and extensors and stem cell transplantation (PBSCT). shoulder abduction. Upper limb reflexes were absent. The neurological findings in the lower limbs were unchanged. -

Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies
Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies Zachary Simmons, MD* KEYWORDS Brachial plexus Brachial plexopathy Axillary nerve Musculocutaneous nerve Suprascapular nerve Nerve conduction studies Electromyography KEY POINTS The brachial plexus provides all motor and sensory innervation of the upper extremity. The plexus is usually derived from the C5 through T1 anterior primary rami, which divide in various ways to form the upper, middle, and lower trunks; the lateral, posterior, and medial cords; and multiple terminal branches. Traction is the most common cause of brachial plexopathy, although compression, lacer- ations, ischemia, neoplasms, radiation, thoracic outlet syndrome, and neuralgic amyotro- phy may all produce brachial plexus lesions. Upper extremity mononeuropathies affecting the musculocutaneous, axillary, and supra- scapular motor nerves and the medial and lateral antebrachial cutaneous sensory nerves often occur in the context of more widespread brachial plexus damage, often from trauma or neuralgic amyotrophy but may occur in isolation. Extensive electrodiagnostic testing often is needed to properly localize lesions of the brachial plexus, frequently requiring testing of sensory nerves, which are not commonly used in the assessment of other types of lesions. INTRODUCTION Few anatomic structures are as daunting to medical students, residents, and prac- ticing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, Conflicts of Interest: None. Neuromuscular Program and ALS Center, Penn State Hershey Medical Center, Penn State College of Medicine, PA, USA * Department of Neurology, Penn State Hershey Medical Center, EC 037 30 Hope Drive, PO Box 859, Hershey, PA 17033.