Neuroprotective Effect of Citicoline on Retinal Cell Damage Induced by Kainic Acid in Rats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Citicoline in the Management of Traumatic Brain Injury
pharmaceuticals Review Role of Citicoline in the Management of Traumatic Brain Injury Julio J. Secades Medical Department, Ferrer, 08029 Barcelona, Spain; [email protected] Abstract: Head injury is among the most devastating types of injury, specifically called Traumatic Brain Injury (TBI). There is a need to diminish the morbidity related with TBI and to improve the outcome of patients suffering TBI. Among the improvements in the treatment of TBI, neuroprotection is one of the upcoming improvements. Citicoline has been used in the management of brain ischemia related disorders, such as TBI. Citicoline has biochemical, pharmacological, and pharmacokinetic characteristics that make it a potentially useful neuroprotective drug for the management of TBI. A short review of these characteristics is included in this paper. Moreover, a narrative review of almost all the published or communicated studies performed with this drug in the management of patients with head injury is included. Based on the results obtained in these clinical studies, it is possible to conclude that citicoline is able to accelerate the recovery of consciousness and to improve the outcome of this kind of patient, with an excellent safety profile. Thus, citicoline could have a potential role in the management of TBI. Keywords: CDP-choline; citicoline; pharmacological neuroprotection; brain ischemia; traumatic brain injury; head injury Citation: Secades, J.J. Role of 1. Introduction Citicoline in the Management of Traumatic brain injury (TBI) is among the most devastating types of injury and can Traumatic Brain Injury. result in a different profile of neurological and cognitive deficits, and even death in the most Pharmaceuticals 2021, 14, 410. -
Eletriptan Smpc
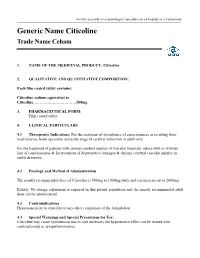
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

More Treatments on Deck for Alcohol Use Disorder
News & Analysis Medical News & Perspectives More Treatments on Deck for Alcohol Use Disorder Jeff Lyon hirteen years have passed since the Raye Z. Litten, PhD, acting director of the ment for AUD were actually prescribed an US Food and Drug Administration NIAAA’s Division of Medications Develop- AUD medication. T (FDA) last approved a new medica- ment and principal investigator of the trial, It is a complicated problem, says John tion to help the nation’s millions of people says the agency is “excited.” Rotrosen, MD, a psychiatrist and addiction withalcoholusedisorder(AUD)stopormod- Nevertheless, the science of alcohol ad- specialist at New York University School of erate their drinking. diction has seen its share of medicines that Medicine. “To a large extent primary care Only 3 such formulations exist, and 1, failed to live up to their early promise dur- physicians don’t screen for alcoholism,” he disulfiram, dates to the Prohibition era. ing full-scale testing. So Litten said the said. “When they do, they may note it, but Known commercially as Antabuse and agency isn’t putting all its eggs in one bas- don’t really do anything about it.” introduced in 1923, it makes people memo- ket. “You need as many weapons as pos- As far as the failure to prescribe exist- rably ill if they ingest alcohol, but it doesn’t sible to treat a complex disease like alcohol ing medications for AUD, Rotrosen blames stop the cravings. The other 2, naltrexone use disorder,” he said. a lack of knowledge. “A lot of doctors in and acamprosate, approved in 1994 and But therein lies a second difficulty. -

Effect of Combined Therapy with Thrombolysis and Citicoline in a Rat
Journal of the Neurological Sciences 247 (2006) 121–129 www.elsevier.com/locate/jns Effect of combined therapy with thrombolysis and citicoline in a rat model of embolic stroke ⁎ María Alonso de Leciñana a,e, , María Gutiérrez a,d, Jose María Roda a,c, Fernando Carceller a,c, Exuperio Díez-Tejedor a,b a Cerebrovascular Research Unit, La Paz University Hospital, Universidad Autónoma de Madrid, Madrid, Spain b Department of Neurology, La Paz University Hospital, Madrid, Spain c Department of Neurosurgery, La Paz University Hospital, Madrid, Spain d Cerebrovascular Experimental Lab, La Paz University Hospital, Madrid, Spain e Department of Neurology, Ramón y Cajal University Hospital, Madrid, Spain Received 28 April 2005; received in revised form 3 January 2006; accepted 3 March 2006 Available online 22 June 2006 Abstract An approach combining reperfusion mediated by thrombolytics with pharmacological neuroprotection aimed at inhibiting the physiopathological disorders responsible for ischemia-reperfusion damage, could provide an optimal treatment of ischemic stroke. We investigate, in a rat embolic stroke model, the combination of rtPA with citicoline as compared to either alone as monotherapy, and whether the neuroprotector should be provided before or after thrombolysis to achieve a greater reduction of ischemic brain damage. One hundred and nine rats have been studied: four were sham-operated and the rest embolized in the right internal carotid artery with an autologous clot and divided among 5 groups: 1) control; 2) iv rtPA 5 mg/kg 30 min post-embolization 3) citicoline 250 mg/kg ip ×3 doses, 10 min, 24 h and 48 h post-embolization; 4) citicoline combined with rtPA following the same pattern; 5) rtPA combined with citicoline, with a first dose 10 min after thrombolysis. -

Anticraving Therapy for Alcohol Use Disorder: a Clinical Review
Received: 10 April 2018 | Revised: 11 June 2018 | Accepted: 11 June 2018 DOI: 10.1002/npr2.12028 INVITED REVIEW Anticraving therapy for alcohol use disorder: A clinical review Winston W. Shen1,2 1Department of Psychiatry, Wan Fang Medical Center, Taipei Medical University, Abstract Taipei, Taiwan Aim: In this review, the author focused on anticraving therapy for alcohol use disor- 2Department of Psychiatry, College of der (AUD) defined by DMS‐5. A comprehensive review was carried out on the avail- Medicine, Taipei Medical University, Taipei, Taiwan able published papers on anticraving drugs for treating AUD patients. Methods: The author described all drugs with anticraving benefits for treating Correspondence Winston W. Shen, Department of AUD patients approved by the Food and Drug Administration of the United States Psychiatry, Wan Fang Medical Center, No. (US FDA) and European Medicines Agency of the European Union. Then, the com- 111, Section 3, Hsing Long Road, Taipei 116, Taiwan. monly prescribed anticraving drugs and those under development were also Email: [email protected] described. Results: The US FDA‐approved anticraving drugs included acamprosate and naltrex- one, and those approved by European Medicines Agency were gamma‐hydroxybuty- rate and nalmefene. The author also highlighted topiramate, gabapentin, ondansetron, LY196044, ifenprodil, varenicline, ABT‐436, mifepristone, citicoline, and baclofen. The putative mechanisms of action of and the use in clinical practice of those anticraving drugs were also described. Conclusion: Although slowly developing, the field of anticraving drugs is getting into shape as a promising entity of a pharmaceutical class of drugs. Then, the author addressed on the underused issues of those recommended, and suggested anticraving drugs by the practice guideline of the American Psychiatric Association. -

The Effect of Rosmarinic Acid on Apoptosis and Nnos Immunoreactivity Following Intrahippocampal Kainic Acid Injections in Rats
Basic and Clinical January, February 2020, Volume 11, Number 1 Research Paper: The Effect of Rosmarinic Acid on Apoptosis and nNOS Immunoreactivity Following Intrahippocampal Kainic Acid Injections in Rats Safoura Khamse1* , Seyed Shahabeddin Sadr1,2 , Mehrdad Roghani3* , Mina Rashvand1 , Maryam Mohammadian4 , Narges Mare- fati1 , Elham Harati1 , Fatemeh Ebrahimi1 1. Department of Physiology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran. 2. Electrophysiology Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran. 3. Neurophysiology Research Center, Shahed University, Tehran, Iran. 4. Department of Physiology, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran. Use your device to scan and read the article online Citation: Khamse, S., Sadr, Sh., Roghani, M., Rashvand, M., Mohammadian, M., & Marefati, N., et al. The Effect of Ros- marinic Acid on Apoptosis and nNOS Immunoreactivity Following Intrahippocampal Kainic Acid Injections in Rats Basic and Clinical Neuroscience, 11(1), 41-48. http://dx.doi.org/10.32598/bcn.9.10.340 http://dx.doi.org/10.32598/bcn.9.10.340 A B S T R A C T Introduction: Kainic Acid (KA) is an ionotropic glutamate receptor agonist. KA can induce neuronal overactivity and excitotoxicity. Rosmarinic Acid (RA) is a natural polyphenolic Article info: compound with antioxidant, anti-apoptotic, anti-neurodegenerative, and anti-inflammatory Received: 12 Apr 2018 properties. This study aimed to assess the effect of RA on apoptosis, nNOS-positive neurons First Revision: 10 May 2018 number, as well as Mitogen-Activated Protein Kinase (MAPK) and Cyclooxygenase-2 (COX- Accepted: 27 Oct 2018 2) immunoreactivity, following intrahippocampal Kainic acid injection in rats. -

Kainic Acid-Induced Neurotoxicity: Targeting Glial Responses and Glia-Derived Cytokines
388 Current Neuropharmacology, 2011, 9, 388-398 Kainic Acid-Induced Neurotoxicity: Targeting Glial Responses and Glia-Derived Cytokines Xing-Mei Zhang1 and Jie Zhu1,2, 1Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Stockholm, Sweden; 2Department of Neurology, The First Hospital of Jilin University, Changchun, China Abstract: Glutamate excitotoxicity contributes to a variety of disorders in the central nervous system, which is triggered primarily by excessive Ca2+ influx arising from overstimulation of glutamate receptors, followed by disintegration of the endoplasmic reticulum (ER) membrane and ER stress, the generation and detoxification of reactive oxygen species as well as mitochondrial dysfunction, leading to neuronal apoptosis and necrosis. Kainic acid (KA), a potent agonist to the -amino- 3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA)/kainate class of glutamate receptors, is 30-fold more potent in neuro- toxicity than glutamate. In rodents, KA injection resulted in recurrent seizures, behavioral changes and subsequent degeneration of selective populations of neurons in the brain, which has been widely used as a model to study the mechanisms of neurode- generative pathways induced by excitatory neurotransmitter. Microglial activation and astrocytes proliferation are the other characteristics of KA-induced neurodegeneration. The cytokines and other inflammatory molecules secreted by activated glia cells can modify the outcome of disease progression. Thus, anti-oxidant and anti-inflammatory treatment could attenuate or prevent KA-induced neurodegeneration. In this review, we summarized updated experimental data with regard to the KA-induced neurotoxicity in the brain and emphasized glial responses and glia-oriented cytokines, tumor necrosis factor-, interleukin (IL)-1, IL-12 and IL-18. -

( 12 ) United States Patent
US010131766B2 (12 ) United States Patent (10 ) Patent No. : US 10 , 131, 766 B2 Hazen et al. (45 ) Date of Patent: Nov . 20 , 2018 ( 54 ) UNSATURATED POLYESTER RESIN 6 ,619 ,886 B1 9 /2003 Harrington 6 ,692 , 802 B1 2 / 2004 Nava SYSTEM FOR CURED IN - PLACE PIPING 7 , 135 ,087 B2 11/ 2006 Blackmore et al. 7 ,799 ,228 B2 9 /2010 Bomak et al . (71 ) Applicant : Interplastic Corporation , Saint Paul, 8 , 047, 238 B2 11/ 2011 Wiessner et al . MN (US ) 8 ,053 ,031 B2 11/ 2011 Stanley et al. 8 ,092 ,689 B2 1 / 2012 Gosselin (72 ) Inventors : Benjamin R . Hazen , Roseville , MN 8 , 298 , 360 B2 10 / 2012 Da Silveira et al. 8 ,418 , 728 B1 4 / 2013 Kiest , Jr . (US ) ; David J . Herzog , Maple Grove , 8 ,586 ,653 B2 11 / 2013 Klopsch et al. MN (US ) ; Louis R . Ross, Cincinnati , 8 ,636 , 869 B2 1 / 2014 Wiessner et al . OH (US ) ; Joel R . Weber , Moundsview , 8 ,741 , 988 B2 6 /2014 Klopsch et al. MN (US ) 8 , 877 , 837 B2 11/ 2014 Yu et al. 9 ,068 , 045 B2 6 /2015 Nava et al. 9 ,074 , 040 B2 7 / 2015 Turshani et al. ( 73 ) Assignee : Interplastic Corporation , St. Paul , MN 9 , 150 , 709 B2 10 / 2015 Klopsch et al . (US ) 9 , 207 , 155 B1 12 / 2015 Allouche et al. 9 ,273 ,815 B2 3 / 2016 Gillanders et al. ( * ) Notice : Subject to any disclaimer, the term of this 9 , 371, 950 B2 6 / 2016 Hairston et al. patent is extended or adjusted under 35 9 , 550 , 933 B2 1 /2017 Chatterji et al . -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

Electrophysiological Mechanisms of Kainic Acid- Induced Epileptiform Activity in the Rat Hippocampal Slice’
0270-6474/84/0405-1312$02,00/O The Journal of Neuroscience Copyright 0 Society for Neuroscience Vol. 4, No. 5, pp. 1312-1323 Printed in U.S.A. May 1984 ELECTROPHYSIOLOGICAL MECHANISMS OF KAINIC ACID- INDUCED EPILEPTIFORM ACTIVITY IN THE RAT HIPPOCAMPAL SLICE’ ROBERT S. FISHER’ AND BRADLEY E. ALGER Department of Physiology, University of Maryland School of Medicine, Baltimore, Maryland 21201 Received August 29, 1983; Revised December 28, 1983; Accepted January 4, 1984 Abstract Depression of GABA-mediated IPSPs has been proposed to be a crucial factor in the onset of epileptiform activity in most models of epilepsy. To test this idea, we studied epileptiform activity induced by bath application of the excitatory neurotoxin kainic acid (KA) in the rat hippocampal slice. Repetitive field potential firing, spontaneous or evoked, occurred during exposure to KA. Intracellular records from 52 CA1 pyramidal cells during changes from control saline to saline containing i PM KA indicated that KA depolarized cells an average of about 5 mV and caused a 15% decrease in input resistance. Action potentials and current-induced burst afterhyperpolariza- tions did not change significantly. In several cells the tonic effects of KA were preceded by a transient phase of sporadic, spontaneous depolarizations of 2 to 10 mV and 50 to 200 msec duration. These phasic depolarizations were blocked by hyperpolarization. The major effect of 1 PM KA was a depression of synaptic potentials. Initially, KA depressed fast GABA-mediated IPSPs and slow, non-GABA-mediated late hyperpolarizing potentials to 23% and 40% of control values, respectively. IPSP depression correlated closely with onset of burst potential firing in response to synaptic stimulation. -

Impact of Citicoline Over Cognitive Impairments After General Anesthesia
International Journal of Science and Research (IJSR) ISSN: 2319-7064 ResearchGate Impact Factor (2018): 0.28 | SJIF (2018): 7.426 Impact of Citicoline over Cognitive Impairments after General Anesthesia Kameliya Tsvetanova Department “Anesthesiology and Resuscitation“, Medical University – Pleven, Bulgaria Abstract: Postoperative cognitive delirium - POCD is chronic damage with deterioration of the memory, the attention and the speed of the processing of the information after anesthesia and operation. It is admitted that anesthetics and other perioperative factors are able to cause cognitive impairments through induction of apoptosis, neuro-inflammation, mitochondrial dysfunction and so on. More and more medicaments are used in modern medicine, as, for instance, Citicoline, which are in a position significantly to reduce this unpleasant complication of the anesthesia. Keywords: Postoperative cognitive delirium, anesthesia, Citicoline. 1. Introduction Therefore, Citocoline is the main intracellular precursor of phospholipid phosphatidyl choline. (13), (14), (15), (16), It is known that anesthetics and other perioperative factors (17), (18), (19), (20), (21), (22), (23), (24), (25), (26) are able to cause cognitive impairments through induction of apoptosis, neuro-inflammation, mitochondrial dysfunction It exerts impact over the cholinergic system and acts as a and so on. choline donor for the enhanced synthesis of acetylcholine. Chronic damage with deterioration of the memory, the attention and the speed of the processing of the information -

NMDA Agonists Using ALZET Osmotic Pumps
ALZET® Bibliography References on the Administration of NMDA Agonists Using ALZET Osmotic Pumps Aspartic Acid P7453: M. Domercq, et al. Excitotoxic oligodendrocyte death and axonal damage induced by glutamate transporter inhibition. Glia 2005;52(1):36-46 ALZET Comments: Oligonucleotide, antisense; oligonucleotide sense; kainate, dihydro-; aspartic acid, DL-threo-B-benzyloxy-; Saline, sterile; CSF/CNS (optic nerve); Rabbit; 1003D; 3 days; Controls received mp w/ vehicle, or contralateral nerves; antisense (glutamate transporters GLAST + GLT-1); animal info (adult, male, white New Zealand). P6888: J. Darman, et al. Viral-induced spinal motor neuron death is non-cell-autonomous and involves glutamate excitotoxicity. Journal of Neuroscience 2004;24(34):7566-7575 ALZET Comments: Aspartic acid, dl-threo-B-hydroxy; spermine, 1-naphthyl acetyl; CSF/CNS (intrathecal, subarachnoid space); Rat; 1007D; 7 days; Controls received mp w/ saline; enzyme inhibitors (GLT-1, GluR2). P3908: A. Hirata, et al. AMPA receptor-mediated slow neuronal death in the rat spinal cord induced by long-term blockade of glutamate transporters with THA. Brain Research 1997;771(37-44 ALZET Comments: Aspartic acid, dl-threo-B-hydroxy; Glutamate, l-; CSF, artificial;; CSF/CNS (subarachnoid space, intrathecal); Rat; 2ML1; no duration posted; dose-response; cannula position verified. P0289: R. M. Mangano, et al. Chronic infusion of endogenous excitatory amino acids into rat striatum and hippocampus. Brain Res. Bull 1983;10(47-51 ALZET Comments: Aminobutyric acid, Y-; Aspartic acid, dl-threo-B-hydroxy; Aspartic acid, l-; Cysteine sulfinic acid; Glutamic acid, l-; Radio-isotopes; 3H tracer; Acetate; Saline; CSF/CNS (corpus striatum); CSF/CNS (hippocampus); Rat; 2002; 2 weeks; comparison of injec.