Child Malnutrition Mortality at St Barnabas Hospital Is High – Is It Due to Practices and Attitudes of Staff?”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2018 Budget Review
Budget Review 2018 Naational Treasury Republic of South Africa 21 February 2018 ISBN: 978-0-621-46020-9 RP: 03/2018 The Budget Review is compiled using the latest available information from departmental and other sources. Some of this information is unaudited or subject to revision. To obtain additional copies of this document, please contact: Communications Directorate National Treasury Private Bag X115 Pretoria 0001 South Africa Tel: +27 12 315 5944 Fax: +27 12 407 9055 The document is also available on the internet at: www.treasury.gov.za. ii iii iii iv iv v v vi Foreword The 2018 Budget arrives at a moment of opportunity for South Africa. A renewed sense of optimism has provided a much-needed boost to confidence and investment. The economic outlook has improved. And government has expressed a new resolve to strengthen policy coordination. Yet this positive turn of events should not blind us to the enormous economic and fiscal challenges facing our country. Economic growth is far too low to reduce alarmingly high unemployment and inequality. Revenue collection, on which government depends to fund social and economic spending programmes, will fall short of projections by R48.2 billion in 2017/18. The finances of several state- owned companies are in a precarious state. The 2017 Medium Term Budget Policy Statement (MTBPS) pointed out that extraordinary measures would be needed to stabilise the public finances. Without such measures, we would only delay the debt reckoning, and a growing share of spending would be absorbed by interest payments. The 2018 Budget proposals address these concerns with resolve. -

28 July 2017
PROVINCIAL ADMINISTRATION: EASTERN CAPE DEPARMENT OF HEALTH The Department of Health is registered with the Department of Labour as a designated Employer and the filling of the following posts will be in line with the Employment Equity Act (including people with disabilities) CLOSING DATE: 28 JULY 2017 NOTE: Applications must be posted on the Z83 Form accompanied by copies of Qualification(s),Identity document (certified in the past 03 months), Proof of registration, proof of citizenship if not RSA citizen, a comprehensive CV, indicating three reference persons: Name and Contact Numbers, A relationship with reference, Reference checks will be done on nominated candidate(s). Note: Failure to submit these copies will result in the application not being considered. Please do not send any original certificates, diplomas or testimonials. Applicants must note that further checks will be conducted once they are short-listed and that their appointment is subject to the outcome of these checks include security clearance, security vetting, qualification verification and criminal checking. Note that correspondence will only be conducted with the short-listed candidates. If you have not been contacted by the dept. of Health within three (3) months of the closing date of the advertisement, please accept that your application was unsuccessful. We thank all applicants for their interest. All shortlisted candidates for SMS posts will be subjected to a technical exercise that intends to test relevant technical elements of the job, the logistics of which will be communicated by department. Following the interview and the technical exercise, the selection panel will recommend candidates to attend a generic managerial competency assessment (in compliance with the DPSA Directive on the implementation of competency based assessments). -

Health Professions Act: List of Approved Facilities for Purposes Of
114 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 No. 797 16 October 2017 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY SPEECH LANGUAGE AND HEARING THERAPISTS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of speech and hearing therapy. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE AMATOLE (Allocated professionals to rotate within the cluster) Buffalo City/Amahlathi Cluster Bhisho Hospital Cathcart Hospital Grey Hospital* Nompumelelo Hospital * S.S GidaHospital* East London Complex Cecilia Makiwane Hospital Empilweni Gompo Hospital Frere Hospital Bedfort Hospital Nkonkobe Cluster Fort Beaufort Hospital Victoria Hospital Tower Hospital(Psychiatry Hospital) Mbashe Cluster Madwaleni Hospital Butterworth Hospital Mnquma Cluster Ngqamakhwe CHC Tafalofefe Hospital ALFRED NZO (Allocated professionals to rotate within the cluster) Maluti Cluster Taylor Bequest(Matatiele) Umzimvubu Cluster Madzikane kaZulu Hospital Mt.Ayliff Hospital Sipetu Hospital CACADU (Allocated professionals to rotate within the cluster This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 16 OKTOBER 2013 No. 36936 115 Cambedoo Cluster Andries Vosloo Hospital Midlands Hospital Kouga Cluster Humansdorp Hospital Makana -

Health Professions Act: List of Approved Facilities for the Purposes
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 39 No. 791 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital** Taylor Bequest Hospital* (Matatiele) Amathole Bhisho CHH Cathcart Hospital * Amahlathi/Buffalo City Cecilia Makiwane Hospital Cluster Dimbaza CHC Duncan Village Day Hospital Empilweni Gompo CHC Fort Grey TB Hospital Frere Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Chris Hani All Saints Hospital** Engcobo/IntsikaYethu Cofimvaba Hospital** Martjie Venter FPA Hospital This gazette is also available free online at www.gpwonline.co.za 40 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 Sub-District Mjanyana Hospital * InxubaYethembaSub-Cradock Hospital** Wilhelm Stahl Hospital** District Inkwanca -

Public Service Vacancy Circular
PUBLIC SERVICE VACANCY CIRCULAR PUBLICATION NO 27 OF 2019 DATE ISSUED: 26 JULY 2019 1. Introduction 1.1 This Circular is, except during December, published on a weekly basis and contains the advertisements of vacant posts and jobs in Public Service departments. 1.2 Although the Circular is issued by the Department of Public Service and Administration, the Department is not responsible for the content of the advertisements. Enquiries about an advertisement must be addressed to the relevant advertising department. 2. Directions to candidates 2.1 Applications on form Z83 with full particulars of the applicants’ training, qualifications, competencies, knowledge and experience (on a separate sheet if necessary or a CV) must be forwarded to the department in which the vacancy/vacancies exist(s). 2.2 Applicants must indicate the reference number of the vacancy in their applications. 2.3 Applicants requiring additional information regarding an advertised post must direct their enquiries to the department where the vacancy exists. The Department of Public Service and Administration must not be approached for such information. 2.4 It must be ensured that applications reach the relevant advertising departments on or before the applicable closing dates. 3. Directions to departments 3.1 The contents of this Circular must be brought to the attention of all employees. 3.2 It must be ensured that employees declared in excess are informed of the advertised vacancies. Potential candidates from the excess group must be assisted in applying timeously for vacancies and attending where applicable, interviews. 3.3 Where vacancies have been identified to promote representativeness, the provisions of sections 15 (affirmative action measures) and 20 (employment equity plan) of the Employment Equity Act, 1998 should be applied. -
Division of Revenue Act: Publication of Health Infrastructure Projects List
STAATSKOERANT, 13 SEPTEMBER 2011 No.34603 3 GOVERNMENT NOTICE DEPARTMENT OF HEALTH No. 740 13 September 2011 PUBLICATION OF HEALTH INFRASTRUCTURE PROJECTS LIST FUNDED THROUGH HEALTH INFRASTRUCTURE GRANT (HIG) IN TERMS OF SECTION 9, OF THE DIVISION OF REVENUE ACT, 2011 (ACT NO.6 OF 2011) I, Dr Aaron Motsoaledi, Minister of Health, hereby publish in the gazette Health Infrastructure Projects list funded through Health Infrastructure Grant which will be imple111 nted during 2011/12 financial year as submitted by provinces. ON MOTSOALEDI, MP MINISTER OF HEALTH DATE: 5/9/2011 Correspondence on the published Health Infrastructure Projects list can directed to the Director-General of Health for the attention of the Programme Manager: Health Planning and System Enablement, Dr A Pillay or Sub Programme Manager: Health Facilities and Infrastructure Management, Mr NN Mphaphuli at Department of Health, P/Bag X828, Pretoria, 0001 4 No. 34603 GOVERNMENT GAZETTE, 13 SEPTEMBER 2011 List of projects funded under Health Infrastructure Grant (HIG)-2011 Project name Project Description MTEF 2011/12 Province ROOD' Cecilia Makiwane Hospital- Phase Completion of Main Kitchen and mortuary EC 2B: Service Buildings 4 Cecilia Makiwane Hospital (CMH)- Phase 3a • 3d: Student Nurses Replacement Nursing college and accommodation Training College & EC Accommodation including fees 40,000 CMH Nurses Temporary Payment of temporary student Nurses accommodation EC Accommodation 7,569 Procurement of Project Management support team on New and replacement assets EC HIG projects -

Health Professions Act: List of Approved Facilities for Purposes Of
40 No. 35624 GOVERNMENT GAZETTE, 27 AUGUST 2012 No. 676 27 August 2012 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2013 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital ** Taylor Bequest Hospital* (Matatiele) Amato le Cathcart Hospital * Cecilia Makiwane Hospital Amahlathi/Buffalo City Dimbaza CHC Cluster Fort Grey TB Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakhwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Zitulele Hospital * Chris Hani All Saints Hospital ** Cofimvaba Hospital ** Engcobo/IntsikaYethu Martjie Venter FPA Hospital Sub-District Mjanyana Hospital * STAATSKOERANT, 27 AUGUSTUS 2012 No. 35624 41 lnxubaYethemba Sub-Cradock Hospital ** Wilhelm Stahl Hospital ** District Inkwanca Molteno FPA Hospital Lukhanji Frontier Hospital* Hewu Hospital * Komani Hospital* Sakhisizwe/Emalahleni Cala Hospital ** Dordrecht FPA Hospital Glen Grey Hospital ** Indwe FPA Hospital Ngonyama CHC* Nelson Mandela Metro Dora Nginza Hospital Empilweni TB Hospital PE Metro Jose Pearson TB Hospital Orsmond TB Hospital Letticia Barn CHC PE Provincial Uitenhage Hospital Kouga Sub-District Humansdorp Hospital BJ Voster FPA Hospital O.R.Tambo Dr Lizo Mpehle Memorial Hospital ** Nessie Knight Hospital ** Mhlontlo Sub-District Qaukeni North Sub-Greenville Hospital ** Holly Cross Hospital ** District Isipethu Hospital* Port St Johns CHC* St. -

The Emerging Threat of Drug-Resistant Tuberculosis in Southern Africa Global and Local Challenges and Solutions
The Emerging Threat of Drug-Resistant Tuberculosis in Southern Africa Global and Local Challenges and Solutions Summary of a Joint WorkShop by the Institute of Medicine and the Academy of Science of South Africa Steve Olson, Yeonwoo Lebovitz, and Anne Claiborne, Rapporteurs Forum on Drug Discovery, Development, and Translation Board on Health Sciences Policy and ACADEMY OF SCIENCE OF SOUTH AFRICA THE NATIONAL ACADEMIES PRESS 500 Fifth Street, N.W. Washington, DC 20001 NOTICE: The project that is the subject of this report was approved by the Govern- ing Board of the National Research Council, whose members are drawn from the councils of the National Academy of Sciences, the National Academy of Engineer- ing, and the Institute of Medicine. This study was supported by Department of Health and Human Services (Contract Nos. N01-OD-4-2139 and 223001003T), the U.S. State Department (S-LMAQM- 08-GR-071), the American Diabetes Association, the American Society for Micro- biology, Amgen Inc., the Association of American Medical Colleges, Bristol-Myers Squibb, the Burroughs Wellcome Fund, Celtic Therapeutics, LLLP, the Critical Path Institute, the Doris Duke Charitable Foundation, Eli Lilly & Co., GlaxoSmithKline, Howard Hughes Medical Institute, Johnson & Johnson, Novartis Pharmaceuticals Corporation, and Pfizer, Inc. Any opinions, findings, conclusions, or recommenda- tions expressed in this publication are those of the author(s) and do not necessarily reflect the view of the organizations or agencies that provided support for this project. International Standard Book Number-13: 978-0-309-16024-7 International Standard Book Number-10: 0-309-16024-3 Additional copies of this report are available from the National Academies Press, 500 Fifth Street, N.W., Lockbox 285, Washington, DC 20055; (800) 624-6242 or (202) 334-3313 (in the Washington metropolitan area); Internet, http://www.nap.edu. -

COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized Hcws
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 36, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 5 September 2020 on the DATCOV platform. HIGHLIGHTS As of 5 September 2020, 2 686 (4.2%) of the 64 705 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 247 facilities (81 public-sector and 166 private-sector) in all nine provinces of South Africa. Among 801/2686 (29.8%) HCWs with available data on type of work, 391/801 (48.8%) were nurses, 168/801 (21.0%) were categorized as other HCWs, 111/801 (13.9%) porters or administrators, 57/801 (7.1%) allied HCWs, 52/801 (6.5%) doctors, 15/801 (1.9%) paramedics, and 7/801 (0.9%) laboratory scientists. There was an increase of 157 new HCW admissions since week 35. There were 360 (13.4%) and 2326 (86.6%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (834, 31.1%), KwaZulu-Natal (656, 24.4%), Eastern Cape (465, 17.3%) and Western Cape (281, 10.5%). The median age of COVID-19 HCW admissions was 49 years, there were 482 (17.9%) admissions in HCWs aged 60 years and older. A total of 1912 (71.2%) were female. -
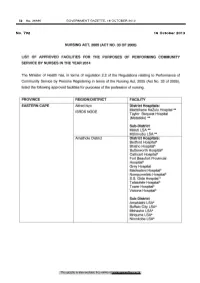
Nursing Act: List of Approved Facilities for the Purposes of Performing Community Service by Nurses in the Year 2014
52 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 No. 792 16 October 2013 NURSING ACT, 2005 (ACT NO. 33 OF 2005) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY NURSES IN THE YEAR 2014 The Minister of Health has, in terms of regulation 2.2 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Nursing Act, 2005 (Act No. 33 of 2005), listed the following approved facilities for purposes of the profession of nursing. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo District Hospitals: Madzikane Ka Zulu Hospital** ISRDS NODE Taylor Bequest Hospital (Matatiele) ** Sub-District Maluti LSA** Mzimvubu LSA*" Amathole District District Hospitals: Bedford Hospital* Bhisho Hospital* Butterworth Hospital* Cathcart Hospital* Fort Beaufort Provincial Hospital* Grey Hospital Madwaleni Hospital* Nompumelelo Hospital* S.S. Gida Hospital * Tafalofefe Hospital* Tower Hospital* Victoria Hospital* Sub-District Amahiathi LSA* Buffalo City LSA* Mbhashe LSA* Mnquma LSA* Nkonkobe LSA* This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 16 OKTOBER 2013 No. 36936 53 Cacadu District District Hospitals Andries Vosloo Hospital* Humansdorp Hospital* Midlands Hospital* Port Alfred Hospital* Settlers Hospital* Sub-Districts Camdeboo LSA* Kouga LSA* Makana LSA* Chris Hani District District Hospitals: All Saints Hospital ** ISRDS NODE Cala Hospital** Cofimvaba Hospital ** Cradock Hospital** Dodrecht Hospital Elliot Hospital ** Glen Grey Hospital ** Hewu -

District Hospital Performance Assessment Re
District Hospital Performance Assessment Eastern Cape 2008-2010 [Part 2: Ukhahlamba (DC14), OR Tambo (DC15), Alfred Nzo (DC44) and Nelson Mandela Metropolitan (NMM) Districts] Sizulu Moyo, Thokozani Mbatha, Catherine Ogunmefun, Peter Bock, Rene English District Hospital Performance Assessment Eastern Cape 2008-2010 [Part 2: Ukhahlamba (DC14), OR Tambo (DC15), Alfred Nzo (DC44) and Nelson Mandela Metropolitan (NMM) Districts] Sizulu Moyo, Thokozani Mbatha, Catherine Ogunmefun, Peter Bock, Rene English Published by Health Systems Trust 34 Essex Terrace Tel: +27 (0)31 266 9090 Westville Fax: +27 (0)31 266 9199 3630 Email: [email protected] South Africa http://www.hst.org.za Published: November 2011 Suggested citation: Moyo S, Mbatha T, Ogunmefun C, Bock P, English R. District Hospital Performance Assessment: Eastern Cape Province 2008-1010 Part 2. Health Systems Trust; Durban, 2012 The information contained in this publication may be freely distributed and reproduced, as long as the source is acknowledged, and it is used for non-commercial purposes. Contents D UKHAHLAMBA DISTRICT - DC-14 .................................................................... 1 1. Aliwal North Hospital ...................................................................................................... 1 i: Description ................................................................................................................... 1 ii: Input and process indicators ....................................................................................... 1 iii: -

2016 Province District List of Facilities Number of Posts 1. Eastern
Available funded posts for Pharmacist Community Service -2016 Number Province District List of facilities of posts 1. Eastern Cape Amathole Adelaide Hospital (1) Komga Hospital (1) Stutterheim Hospital (1) Bedford Hospital (1) Madwaleni Hospital (1) Tafalofefe Hospital (1) Butterworth Hospital (1) Nompumelelo Hospital (1) Tower TB Hospital (1) Carthcart Hospital (1) Nqamakhwe CHC (1) Victoria Hospital (1) 14 Fort Beaufort Hospital (1) SS Gida Hospital (1) Alfred Nzo Maluti CHC (1) Mount Ayliff Hospital (1) Taylor Bequest Hospital (1) 03 Buffalo City Bhisho (1) Empilweni Gompo Day Grey Hospital (1) Dimbaza CHC (1) Hospital (1) Nkqubela TB Hospital (1) Duncan Village Day Fort Grey (1) 07 Hospital (1) Cacadu Andries Vosloo (1) Midlands Hospital (1) Settlers CHC (1) Fort England Hospital (1) Port Alfred Hospital (1) Temba TB Hospital (1) Humansdorp Hospital (1) PZ Meyer TB Hospital (1) Wilhelm Stahl Hospital (1) 12 Margery Parkes (1) Settlers Hospital (1) Willowmore Hospital (1) Chris Hani All Saints Hospital (1) Dordrecht Hospital (1) Indwe Hospital (1) Cala Hospital (1) Elliot Hospital (1) Komani Hospital (1) Cofimvaba Hospital (1) Frontier Hospital (1) Maclear Hospital (1) 12 Cradock Hospital (1) Clen Grey Hospital (1) Moltena Hospital (1) Joe Gqabi Aliwal North Hospital (1) Empilisweni Hospital (1) Tayler Bequest Hospital (1) Burgersdorp Hospital (1) Lady Grey Hospital (1) Umlamli Hospital (1) 07 Cloete Jourbet Hospital (1) Nelson Mandela PE Pharmaceutical Depot (1) Kwa Zwakhele CHC (1) Orsmond TB Hospital (1) Metro Empilweni Hospital