Drug Induced QT Prolongation and Torsades De Pointes (Tdp)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Concentration Dependent Cardiotoxicity of Terodiline in Patients Treated for Urinary Incontinence
Br HeartJ7 1995;74:53-56 53 Concentration dependent cardiotoxicity of terodiline in patients treated for urinary incontinence Simon H L Thomas, P Daniel Higham, Kenneth Hartigan-Go, Farhad Kamali, Peter Wood, Ronald W F Campbell, Gary A Ford Abstract Terodiline hydrochloride is an antimuscarinic Objective-Terodiline, an antimuscarinic drug with calcium antagonist properties' and calcium antagonist drug, was used to which was used for treating urinary inconti- treat detrusor instability but was with- nence caused by detrusor instability.2 The drawn in 1991 after provoking serious drug was withdrawn in 1991 after reports of ventricular arrhythmias associated with cardiac dysrhythmia including bradycardia, increases in the corrected QT interval heart block, ventricular fibrillation, and ven- (QTc). This research was performed to tricular tachycardia, usually of the torsade de relate drug induced electrocardiographic pointes-type34 and associated with QT pro- changes in asymptomatic recipients to longation. Plasma terodiline concentrations plasma concentrations of the R( +) and were very high in one affected patient. S(-) terodiline enantiomers. Predisposing factors for terodiline associated Setting-Urological and geriatric clinics torsade de pointes were old age, coexisting and wards. ischaemic heart disease, co-prescription of Subjects-Asymptomatic patients taking other cardioactive drugs, and hypokalaemia. terodiline in stable dose. Torsade de pointes is associated with Methods-Electrocardiograms (50 mm/s) abnormal prolongation of the ventricular were collected from patients while they refractory period which results in a long QT were taking terodiline and compared with interval on the electrocardiogram and is often ECGs obtained before or after terodiline. drug induced.5 Increased dispersion of ven- QT interval, heart rate corrected QT tricular recovery may be important in the interval (QTc), and QT dispersion (QTd) development of this arrhythmia and indirect were measured. -

Effect of Oxybutynin on the Qtc Interval in Elderly Patients with Urinary Incontinence
Br J Clin Pharmaco/1996; 41: 73-75 Effect of oxybutynin on the QTc interval in elderly patients with urinary incontinence R. M. HUSSAIW, K. HARTIGAN-G02, S. H. L. THOMAS2 & G. A. FORDL2 Departments of 1 Medicine (Geriatrics) and 2Pharmacological Sciences, University of Newcastle upon Tyne, UK. I Terodiline, an anticholinergic drug with calcium antagonist properties, is associated with QT prolongation and ventricular arrhythmias. It is not known if oxybutynin, a drug with a similar pharmacological profile, causes QT prolongation. ECGs were obtained before and at least 4 weeks after commencement of oxybutynin (mean daily dose 7.6, range 2.5-10 mg), in 21 elderly (mean age 75, range 58-88 years) patients treated for urinary incontinence. Heart rate, (mean±s.d.) 74± 11 vs 69± 11 beats min- 1, -6 (-13,2), before vs during oxybutynin therapy, mean difference (95% confidence intervals); PR interval, 168±27 vs 156±27 ms, -11 (-26,3); QTc 454±27 vs 447±31 ms 112, -9 (-23,5), and QTc dispersion, QTc max-QTc min, 68±24 vs 63±26 ms 112, -1 (-15,14) were all unaltered by oxybutynin therapy. The lack of an effect on resting heart rate suggests that oxybutynin has little anticholinergic action at cardiac M2 receptors at usually administered doses. Oxybutynin therapy is not associated with QTc interval prolongation and is unlikely to produce ventricular arrhythmias. Keywords QT interval oxybutynin agemg Introduction prevalence of cardiovascular disease and are therefore at particular risk of cardiovascular adverse drug reac Urinary incontinence is a common disability in the tions. -

Drugs for Primary Prevention of Atherosclerotic Cardiovascular Disease: an Overview of Systematic Reviews
Supplementary Online Content Karmali KN, Lloyd-Jones DM, Berendsen MA, et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. Published online April 27, 2016. doi:10.1001/jamacardio.2016.0218. eAppendix 1. Search Documentation Details eAppendix 2. Background, Methods, and Results of Systematic Review of Combination Drug Therapy to Evaluate for Potential Interaction of Effects eAppendix 3. PRISMA Flow Charts for Each Drug Class and Detailed Systematic Review Characteristics and Summary of Included Systematic Reviews and Meta-analyses eAppendix 4. List of Excluded Studies and Reasons for Exclusion This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. 1 Downloaded From: https://jamanetwork.com/ on 09/28/2021 eAppendix 1. Search Documentation Details. Database Organizing body Purpose Pros Cons Cochrane Cochrane Library in Database of all available -Curated by the Cochrane -Content is limited to Database of the United Kingdom systematic reviews and Collaboration reviews completed Systematic (UK) protocols published by by the Cochrane Reviews the Cochrane -Only systematic reviews Collaboration Collaboration and systematic review protocols Database of National Health Collection of structured -Curated by Centre for -Only provides Abstracts of Services (NHS) abstracts and Reviews and Dissemination structured abstracts Reviews of Centre for Reviews bibliographic -
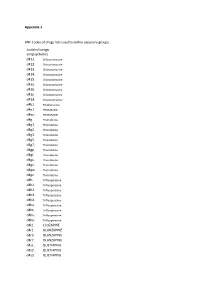
Appendix 1 BNF Codes of Drugs Lists Used to Define Exposure Groups
Appendix 1 BNF Codes of drugs lists used to define exposure groups. Anticholinergic antipsychotics d411. Chlorpromazine d412. Chlorpromazine d413. Chlorpromazine d414. Chlorpromazine d415. Chlorpromazine d41a. Chlorpromazine d41b. Chlorpromazine d41c. Chlorpromazine d41d. Chlorpromazine d4b1. Perphenazine d4e1. PROMAZINE d4ex. PROMAZINE d4g.. Thioridazine d4g1. Thioridazine d4g2. Thioridazine d4g3. Thioridazine d4g5. Thioridazine d4g7. Thioridazine d4gp. Thioridazine d4gt. Thioridazine d4gu. Thioridazine d4gv. Thioridazine d4gw. Thioridazine d4gz. Thioridazine d4h.. Trifluoperazine d4h1. Trifluoperazine d4h2. Trifluoperazine d4h3. Trifluoperazine d4h4. Trifluoperazine d4hs. Trifluoperazine d4ht. Trifluoperazine d4hu. Trifluoperazine d4hx. Trifluoperazine d4l2. CLOZAPINE d4r1. OLANZAPINE d4r3. OLANZAPINE d4r7. OLANZAPINE d4s1. QUETIAPINE d4s2. QUETIAPINE d4s3. QUETIAPINE d4s5. QUETIAPINE d4ss. QUETIAPINE d4sx. QUETIAPINE Tricyclic antidepressants d7... d71.. Amitriptyline d711. Amitriptyline d712. Amitriptyline d713. Amitriptyline d719. Amitriptyline d71a. Amitriptyline d71b. Amitriptyline d71c. Amitriptyline d71d. Amitriptyline d71e. Amitriptyline d71f. Amitriptyline d71u. Amitriptyline d71v. Amitriptyline d71w. Amitriptyline d71y. Amitriptyline d71z. Amitriptyline d73.. Clomipramine d731. Clomipramine d732. Clomipramine d733. Clomipramine d736. Clomipramine d73s. Clomipramine d73t. Clomipramine d73u. Clomipramine d73v. Clomipramine d73w. Clomipramine d73z. Clomipramine d75.. DOSULEPIN d751. DOSULEPIN d752. DOSULEPIN d755. DOSULEPIN d756. -

Drug Misuse and Dependence : UK Guidelines on Clinical Management
Drug misuse and dependence UK guidelines on clinical management Title: Drug misuse and dependence: UK guidelines on clinical management Recommended citation: Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group (2017) Drug misuse and dependence: UK guidelines on clinical management. London: Department of Health Author: Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group Publisher: Global and Public Health / Population Health / Healthy Behaviours / 25460 Document purpose: Guidance Publication date: July 2017 Target audience: Healthcare professionals Providers and commissioners of treatment for people who misuse or are dependent on drugs Professional and regulatory bodies Service users and carers Contact details: Alcohol, Drugs & Tobacco Division Public Health England [email protected] You may re-use the text of this document (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit www.nationalarchives.gov.uk/ doc/open-government-licence/ © Crown copyright Published to gov.uk www.gov.uk/dh Drug misuse and dependence UK guidelines on clinical management Prepared by Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group Contents 1 Contents Preface 5 Professor Sir John Strang 5 Chapter 1: Introduction 9 Chapter 2: Essential elements of treatment provision 15 2.1 Key points 15 2.2 Assessment, planning care and treatment 15 2.3 Delivery -

Concentration Dependent Cardiotoxicity of Terodiline in Patients Treated for Urinary Incontinence Br Heart J: First Published As 10.1136/Hrt.74.1.53 on 1 July 1995
Br HeartJ7 1995;74:53-56 53 Concentration dependent cardiotoxicity of terodiline in patients treated for urinary incontinence Br Heart J: first published as 10.1136/hrt.74.1.53 on 1 July 1995. Downloaded from Simon H L Thomas, P Daniel Higham, Kenneth Hartigan-Go, Farhad Kamali, Peter Wood, Ronald W F Campbell, Gary A Ford Abstract Terodiline hydrochloride is an antimuscarinic Objective-Terodiline, an antimuscarinic drug with calcium antagonist properties' and calcium antagonist drug, was used to which was used for treating urinary inconti- treat detrusor instability but was with- nence caused by detrusor instability.2 The drawn in 1991 after provoking serious drug was withdrawn in 1991 after reports of ventricular arrhythmias associated with cardiac dysrhythmia including bradycardia, increases in the corrected QT interval heart block, ventricular fibrillation, and ven- (QTc). This research was performed to tricular tachycardia, usually of the torsade de relate drug induced electrocardiographic pointes-type34 and associated with QT pro- changes in asymptomatic recipients to longation. Plasma terodiline concentrations plasma concentrations of the R( +) and were very high in one affected patient. S(-) terodiline enantiomers. Predisposing factors for terodiline associated Setting-Urological and geriatric clinics torsade de pointes were old age, coexisting and wards. ischaemic heart disease, co-prescription of Subjects-Asymptomatic patients taking other cardioactive drugs, and hypokalaemia. terodiline in stable dose. Torsade de pointes is associated with Methods-Electrocardiograms (50 mm/s) abnormal prolongation of the ventricular were collected from patients while they refractory period which results in a long QT were taking terodiline and compared with interval on the electrocardiogram and is often ECGs obtained before or after terodiline. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Genetic and Molecular Aspects of Drug-Induced QT Interval Prolongation
International Journal of Molecular Sciences Review Genetic and Molecular Aspects of Drug-Induced QT Interval Prolongation Daniela Baracaldo-Santamaría 1 , Kevin Llinás-Caballero 2,3 , Julián Miguel Corso-Ramirez 1 , Carlos Martín Restrepo 2 , Camilo Alberto Dominguez-Dominguez 1 , Dora Janeth Fonseca-Mendoza 2 and Carlos Alberto Calderon-Ospina 2,* 1 School of Medicine and Health Sciences, Universidad del Rosario, Bogotá 111221, Colombia; [email protected] (D.B.-S.); [email protected] (J.M.C.-R.); [email protected] (C.A.D.-D.) 2 GENIUROS Research Group, Center for Research in Genetics and Genomics (CIGGUR), School of Medicine and Health Sciences, Universidad del Rosario, Bogotá 111221, Colombia; [email protected] (K.L.-C.); [email protected] (C.M.R.); [email protected] (D.J.F.-M.) 3 Institute for Immunological Research, University of Cartagena, Cartagena 130014, Colombia * Correspondence: [email protected]; Tel.: +57-1-2970200 (ext. 3318) Abstract: Long QT syndromes can be either acquired or congenital. Drugs are one of the many etiologies that may induce acquired long QT syndrome. In fact, many drugs frequently used in the clinical setting are a known risk factor for a prolonged QT interval, thus increasing the chances of developing torsade de pointes. The molecular mechanisms involved in the prolongation of the QT interval are common to most medications. However, there is considerable inter-individual variability Citation: Baracaldo-Santamaría, D.; Llinás-Caballero, K.; Corso-Ramirez, in drug response, thus making the application of personalized medicine a relevant aspect in long QT J.M.; Restrepo, C.M.; syndrome, in order to evaluate the risk of every individual from a pharmacogenetic standpoint. -

Sudden Death in a Patient Taking Antipsychotic Drugs
Adverse drug reactions 445 Sudden death in a patient taking antipsychotic Postgrad Med J: first published as 10.1136/pgmj.74.873.445 on 1 July 1998. Downloaded from drugs S H L Thomas, P N Cooper Cardiac arrhythmias are sometimes caused by disease. Thioridazine was considered as a pos- drugs. One mechanism for drug-induced sible contributing factor and a Yellow Card was pro-arrhythmia is delayed ventricular repolari- sent to the Committee on Safety of Medicines sation, reflected on the surface electrocardio- (CSM). gram (ECG) as prolongation of the QT interval, which is associated with a number of Discussion drugs (box 1). Patients with drug-induced QT prolongation are at risk of the polymorphic Spontaneous reporting schemes, such as the ventricular tachycardia torsade de pointes. While Yellow Card scheme in the UK, are of value in usually self-limiting, this may degenerate into detecting serious adverse reactions to drugs, ventricular fibrillation.' but one limitation of these schemes, even for fatal adverse events, is under-reporting. It has Case summary been estimated that only 15% of fatal episodes of thromboembolism in women taking com- A 68-year-old man with a 5-year history of bined oral contraceptives,2 and 11% of fatal Alzheimer's disease and cervical spondylosis blood dyscrasias associated with phenylbuta- was admitted to a psychogeriatric ward be- zone or oxyphenbutazone,' were reported by cause of a deterioration in his mental state. He doctors or coroners. One possible reason for had no history of heart disease or epilepsy. this is that a cause and effect relationship may Because of violent outbursts he was treated be uncertain. -

Cardioid: Whole Human Heart Modeling and Simulation
Cardioid: Whole Human Heart Modeling and Simulation a collaboration between IBM and Lawrence Livermore National Laboratory Dr. Frederick Streitz Director, HPC Innovation Center Lawrence Livermore National Laboratory This work was performed under the auspices of the U.S. Department of Energy by Lawrence Livermore National Laboratory under contract DE-AC52-07NA27344 LLNL-PRES-603112 Partnership Overview • LLNL partnering with U.S. industry to promote U.S. competitiveness • Creates Livermore Valley Open Campus and the HPC Innovation Center • IBM partnering with LLNL to form Deep Computing Solutions in the HPCIC • Working together, IBM and LLNL create Cardioid code: aimed at accelerating cures for heart disease and aiding in drug screening and the development of new medical devices and patient-specific therapies. • Seeking partners for application and commercialization of Cardioid, as well as other projects Partnering with Lawrence Livermore National Laboratory • Livermore Valley Open Campus: research park environment with collaborative space • Ready access for all partners to world-renowned facilities and resources • HPCIC delivers computing solutions with access to computing and expertise HPCIC • Coming Soon: Institute for Translational Biomedicine • 25 year plan to develop 2.5M sq.ft. hosting 3,000 researchers HPCIC and Deep Computing Solutions • Innovation ecosystem focused on HPC solutions for industry problems Partnering with industry to develop, prove, • HPCIC offers access to world-class and deploy HPC solutions computing resources -

Pharmaceuticals (Monocomponent Products) ………………………..………… 31 Pharmaceuticals (Combination and Group Products) ………………….……
DESA The Department of Economic and Social Affairs of the United Nations Secretariat is a vital interface between global and policies in the economic, social and environmental spheres and national action. The Department works in three main interlinked areas: (i) it compiles, generates and analyses a wide range of economic, social and environmental data and information on which States Members of the United Nations draw to review common problems and to take stock of policy options; (ii) it facilitates the negotiations of Member States in many intergovernmental bodies on joint courses of action to address ongoing or emerging global challenges; and (iii) it advises interested Governments on the ways and means of translating policy frameworks developed in United Nations conferences and summits into programmes at the country level and, through technical assistance, helps build national capacities. Note Symbols of United Nations documents are composed of the capital letters combined with figures. Mention of such a symbol indicates a reference to a United Nations document. Applications for the right to reproduce this work or parts thereof are welcomed and should be sent to the Secretary, United Nations Publications Board, United Nations Headquarters, New York, NY 10017, United States of America. Governments and governmental institutions may reproduce this work or parts thereof without permission, but are requested to inform the United Nations of such reproduction. UNITED NATIONS PUBLICATION Copyright @ United Nations, 2005 All rights reserved TABLE OF CONTENTS Introduction …………………………………………………………..……..……..….. 4 Alphabetical Listing of products ……..………………………………..….….…..….... 8 Classified Listing of products ………………………………………………………… 20 List of codes for countries, territories and areas ………………………...…….……… 30 PART I. REGULATORY INFORMATION Pharmaceuticals (monocomponent products) ………………………..………… 31 Pharmaceuticals (combination and group products) ………………….……........ -

Practitioners' Section
427 428 SAFER MOLECULES THROUGH CHIRALITY PRACTITIONERS’ SECTION development of safer alternatives to existing racemates. DEVELOPMENT OF SAFER MOLECULES THROUGH CHIRALITY Basics of chirality[1-4] Compounds can be chiral or achiral (non-chiral). P. A. PATIL*, M. A. KOTHEKAR** Chiral compounds possess the property of handedness, i.e., they may be right-handed or Figure 1: Chiral structure of ibuprofen ABSTRACT left-handed. These two - left- and right-handed nomenclature are mutually exclusive. R - forms of a chiral compound are identical in Many of the drugs currently used in medical practice are mixtures of enantiomers enantiomer of one compound may be their structural formulas but differ in spatial (racemates). Many a times, the two enantiomers differ in their pharmacokinetic and dextrorotatory, while another compound may arrangement so that one form is exactly a mirror pharmacodynamic properties. Replacing existing racemates with single isomers has have its S enantiomer as dextrorotatory. resulted in improved safety and/or efficacy profile of various racemates. In this review, image of the other but the two forms are not superimposable on one another. This is akin to pharmacokinetic and pharmacodynamic implications of chirality are discussed in brief, A collection containing only one enantiomeric pair of gloves, socks or hands. An achiral followed by an overview of some important chiral switches that have yielded safer form of a chiral molecule is called an optically alternatives. These include levosalbutamol, S-ketamine, levobupivacaine, S-zopiclone, object exists only in one form and there is no pure, chirally pure or enantiomerically pure levocetirizine, S-amlodipine, S-atenolol, S-metoprolol, S-omeprazole, S-pantoprazole possibility of left- or right-handedness.