An Approach to Spider Bites Erroneous Attribution of Dermonecrotic Lesions to Brown Recluse Or Hobo Spider Bites in Canada Robert G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RESEARCH ARTICLE Anti-Glioma Effect of Pseudosynanceia
DOI:10.31557/APJCP.2021.22.7.2295 Effect of Pseudosynanceia Melanostigma Venom on Glioblastoma Cells RESEARCH ARTICLE Editorial Process: Submission:02/14/2021 Acceptance:07/15/2021 Anti-Glioma Effect of Pseudosynanceia Melanostigma Venom on Isolated Mitochondria from Glioblastoma Cells Maral Ramezani, Fatemeh Samiei, Jalal Pourahmad* Abstract Background: Glioblastoma is the most common primary malignant tumor of the central nervous system that occurs in the spinal cord or brain. Pseudosynanceia Melanostigma is a venomous stonefish in the Persian Gulf, which our knowledge about is little. This study’s goal is to investigate the toxicity of stonefish crude venom on mitochondria isolated from U87 cells. Methods: In the first stage, we extracted venom stonefish and then isolated mitochondria have exposed to different concentrations of venom. Finally, mitochondrial toxicity parameters (Succinate dehydrogenase (SDH) activity, Reactive oxygen species (ROS), cytochrome c release, Mitochondrial Membrane Potential (MMP), and mitochondrial swelling) have evaluated. Results: To determine mitochondrial parameters, we used 115, 230, and 460 µg/ml concentrations. The results of our study show that the venom of stonefish selectively increases upstream parameters of apoptosis such as mitochondrial swelling, cytochrome c release, MMP collapse and ROS. Conclusion: This study suggests that Pseudosynanceia Melanostigma crude venom has selectively caused toxicity by increasing active mitochondrial oxygen radicals. This venom could potentially be a candidate for the treatment of glioblastoma. Keywords: Mitochondria- glioblastoma- fish venoms- cell line- tumor- toxicity-Persian Gulf Asian Pac J Cancer Prev, 22 (7), 2295-2302 Introduction freshwater or saltwater. Marine animals most commonly used for animals live in saltwater, i.e. in oceans, seas, Glioblastoma multiform is the most common group of etc. -

Katsushika Hokusai and a Poetics of Nostalgia
ACCESS: CONTEMPORARY ISSUES IN EDUCATION 2015, VOL. 33, NO. 1, 33–46 https://doi.org/10.1080/00131857.2014.964158 Katsushika Hokusai and a Poetics of Nostalgia David Bell College of Education, University of Otago ABSTRACT KEYWORDS This article addresses the activation of aesthetics through the examination of cultural memory, Hokusai, an acute sensitivity to melancholy and time permeating the literary and ukiyo-e, poetic allusion, nostalgia, mono no aware pictorial arts of Japan. In medieval court circles, this sensitivity was activated through a pervasive sense of aware, a poignant reflection on the pathos of things. This sensibility became the motivating force for court verse, and ARTICLE HISTORY through this medium, for the mature projects of the ukiyo-e ‘floating world First published in picture’ artist Katsushika Hokusai. Hokusai reached back to aware sensibilities, Educational Philosophy and Theory, 2015, Vol. 47, No. 6, subjects and conventions in celebrations of the poetic that sustained cultural 579–595 memories resonating classical lyric and pastoral themes. This paper examines how this elegiac sensibility activated Hokusai’s preoccupations with poetic allusion in his late representations of scholar-poets and the unfinished series of Hyakunin isshu uba-ga etoki, ‘One hundred poems, by one hundred poets, explained by the nurse’. It examines four works to explain how their synthesis of the visual and poetic could sustain aware themes and tropes over time to maintain a distinctive sense of this aesthetic sensibility in Japan. Introduction: Mono no aware How can an aesthetic sensibility become an activating force in and through poetic and pictorial amalgams of specific cultural histories and memories? This article examines how the poignant aesthetic sensibility of mono no aware (a ‘sensitivity to the pathos of things’) established a guiding inflection for social engagements of the Heian period (794–1185CE) Fujiwara court in Japan. -

From Grasping to Emptiness – Excursions Into the Thought-World of the Pāli Discourses (2)
From Grasping to Emptiness – Excursions into the Thought-world of the Pāli Discourses (2) Anālayo © 2010 Anālayo Published by The Buddhist Association of the United States 2020 Route 301, Carmel, New York 10512 Printed in Taiwan Cover design by Laurent Dhaussy ISBN 978-0-615-25529-3 Introduction 3 1. Grasping / Upādāna 5 1.1 Grasping at Sensual Pleasures 5 1.2 Grasping at Views 7 1.3 Grasping at Rules and Observances 9 1.4 Grasping at a Doctrine of Self 10 1.5 The Five Aggregates [Affected by] Clinging 13 1.6 Grasping and Nibbāna 15 1.7 Freedom from Grasping 16 2. Personality View / Sakkāyadihi 19 2.1 Manifestations of Personality View 19 2.2 Removal of Personality View 24 3. Right View / Sammādihi 27 3.1 Wrong View 27 3.2 Right View and Investigation 29 3.3 Right View as the Forerunner of the Path 31 3.4 Arrival at Right View 33 3.5 Right View and the Four Noble Truths 34 4. Volitional Formations / Sakhārā 39 4.1 Sakhāras as an Aggregate 40 4.2 Sakhāras as a Link in Dependent Arising 44 4.3 Sakhāras in General 48 5. Thought / Vitakka 55 5.1 The Ethical Perspective on Thought 56 5.2 The Arising of Thought 57 5.3 The Vitakkasahāna-sutta 60 5.4 Vitakka in Meditation 64 5.5 Thought Imagery 66 6. Wise Attention / Yoniso Manasikāra 69 6.1 Wise ( Yoniso ) 69 6.2 Attention ( Manasikāra ) 72 6.3 The Implications of Wise Attention 72 6.4 The Importance of Wise Attention 78 7. -

Spider Bites
Infectious Disease Epidemiology Section Office of Public Health, Louisiana Dept of Health & Hospitals 800-256-2748 (24 hr number) www.infectiousdisease.dhh.louisiana.gov SPIDER BITES Revised 6/13/2007 Epidemiology There are over 3,000 species of spiders native to the United States. Due to fragility or inadequate length of fangs, only a limited number of species are capable of inflicting noticeable wounds on human beings, although several small species of spiders are able to bite humans, but with little or no demonstrable effect. The final determination of etiology of 80% of suspected spider bites in the U.S. is, in fact, an alternate diagnosis. Therefore the perceived risk of spider bites far exceeds actual risk. Tick bites, chemical burns, lesions from poison ivy or oak, cutaneous anthrax, diabetic ulcer, erythema migrans from Lyme disease, erythema from Rocky Mountain Spotted Fever, sporotrichosis, Staphylococcus infections, Stephens Johnson syndrome, syphilitic chancre, thromboembolic effects of Leishmaniasis, toxic epidermal necrolyis, shingles, early chicken pox lesions, bites from other arthropods and idiopathic dermal necrosis have all been misdiagnosed as spider bites. Almost all bites from spiders are inflicted by the spider in self defense, when a human inadvertently upsets or invades the spider’s space. Of spiders in the United States capable of biting, only a few are considered dangerous to human beings. Bites from the following species of spiders can result in serious sequelae: Louisiana Office of Public Health – Infectious Disease Epidemiology Section Page 1 of 14 The Brown Recluse: Loxosceles reclusa Photo Courtesy of the Texas Department of State Health Services The most common species associated with medically important spider bites: • Physical characteristics o Length: Approximately 1 inch o Appearance: A violin shaped mark can be visualized on the dorsum (top). -

UNITED STATES DISTRICT COURT EASTERN DISTRICT of MISSOURI EASTERN DIVISION JEFFREY D. BRIDGES, ) ) Plaintiff, ) ) V. )
Case: 4:06-cv-01200-ERW Doc. #: 16 Filed: 07/26/07 Page: 1 of 40 PageID #: <pageID> UNITED STATES DISTRICT COURT EASTERN DISTRICT OF MISSOURI EASTERN DIVISION JEFFREY D. BRIDGES, ) ) Plaintiff, ) ) v. ) Case number 4:06cv1200 ERW ) TCM MICHAEL J. ASTRUE, ) Commissioner of Social Security,1 ) ) Defendant. ) REPORT AND RECOMMENDATION OF UNITED STATES MAGISTRATE JUDGE This is an action under 42 U.S.C. § 405(g) for judicial review of the final decision of Michael Astrue, the Commissioner of Social Security ("Commissioner"), denying Jeffrey D. Bridges disability insurance benefits ("DIB") under Title II of the Social Security Act ("the Act"), 42 U.S.C. §§ 401-433. Plaintiff has filed a brief in support of his complaint; the Commissioner has filed a brief in support of his answer. The case was referred to the undersigned United States Magistrate Judge for a review and recommended disposition pursuant to 28 U.S.C. § 636(b). Procedural History Jeffrey D. Bridges ("Plaintiff") applied for DIB in December 2003, alleging he was disabled as of January 2000 by Wegener's disease, stress, aches and pains, memory loss, 1Mr. Astrue was sworn in as the Commissioner of Social Security on February 12, 2007, and is hereby substituted as defendant pursuant to Rule 25(d)(1) of the Federal Rules of Civil Procedure. Case: 4:06-cv-01200-ERW Doc. #: 16 Filed: 07/26/07 Page: 2 of 40 PageID #: <pageID> depression, high blood pressure, and anxiety. (R. at 48-50.)2 This application was denied initially and after a hearing held in November 2004 before Administrative Law Judge ("ALJ") James B. -

Violent Incidents Between Humans and Orcas in Captivity
Violent incidents between humans and orcas in captivity Several accounts of violent incidents with humans have appeared in books and news clips, with little information on the dates or details of those incidents. Other descriptions have made headlines, and some were captured on video tape. There are also anecdotal reports of incidents that were never officially documented. NO. DATE AQUARIUM WHALEs INCIDENT SOURCE early years New York When water level was lowered for pool cleaning, young female Lupa sent Edward R. Riciuti, , New #1 1968 Lupa York, Walker & Co., 1973, Aquarium, USA trainers scrambling from the pool, snapping her jaws threatening. pp. 227-228. Edward R. Riciuti, Killers of the Sea, New York, Young male Cuddles became so increasingly aggressive, having a hold of at Walker & Co., 1973, pp. Flamingo Park, least two trainers, that keepers had to clean the pool from the protection of a 227-228; Reading #2 1969-1970 Cuddles England shark cage. Cuddles also dragged keeper Don Robinson into the pool when he Eagle, August 15, was at Dudley Zoo but that was possibly a PR stunt. 1971; Doug Cartlidge, personal communication, March 2010. Karen Pryor writes, "I have since heard... of at least one killer whale which Karen Pryor, Lads Before the Wind, New York, #3 1970s unknown unknown launched an unprovoked attack on a favorite trainer, in normal circumstances, Harper & Row, 1976, p. savaged him very badly, and nearly killed him." 220. Vancouver Trainer Doug Pemberton described young female Skana as the dominant Cranky killer whales put trainers through their #4 1970's Aquarium, Skana animal in the pool. -

Awareness, Prevention and Treatment of World-Wide Marine Stings and Bites
Awareness, Prevention and Treatment of world-wide marine stings and bites Dr Peter Fenner Honorary Medical Officer, Surf Life Saving Australia International Life Saving Federation Medical/Rescue Conference Proceedings September 1997 Abstract The most common world-wide first aid treatment used by the average lifesaver/lifeguard is the treatment of marine envenomation, especially the treatment of jellyfish stings. It is important to use the correct first aid treatment for each type of envenomation. This study provides a simplified protocol for: - 1. Awareness of the geographical distribution and possibilities of envenomation enabling: - 2. Preventative strategies to reduce morbidity and mortality from marine envenomation 3. First aid treatment of marine envenomation by jellyfish or other marine animals This discussion is based on protocols developed for Surf Life Saving Australia and other first aid providers in Australia over the past ten years. Their success has been proven by a 30% reduction in the number of stings over the past 10 years (statistics from the author’s records). Information for this article has been taken from: - 1. Venomous and poisonous marine animals: a medical and biological handbook produced by Surf Life Saving Queensland 2. The global problem of cnidarian stinging. MD Thesis by the author for the University of London. Introduction The global problem of marine envenomation is not fully appreciated. Each year hundreds of deaths occur from poisoning (by ingestion or eating) or by envenomation (stinging by jellyfish, or biting by venomous marine animals). The morbidity is even greater with jellyfish stings world-wide being numbered in their millions. Each summer it is estimated that up to half a million stings occur on the east coast of the United States from the Portuguese man-o’-war (Physalia physalis). -

Factors Influencing Depression in Men: a Qualitative Investigation
University of Kentucky UKnowledge Theses and Dissertations--Nursing College of Nursing 2015 Factors Influencing Depression in Men: A Qualitative Investigation Lori A. Mutiso University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Mutiso, Lori A., "Factors Influencing Depression in Men: A Qualitative Investigation" (2015). Theses and Dissertations--Nursing. 15. https://uknowledge.uky.edu/nursing_etds/15 This Doctoral Dissertation is brought to you for free and open access by the College of Nursing at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Nursing by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. I agree that the document mentioned above may be made available immediately for worldwide access unless an embargo applies. -

From Grasping to Emptiness – Excursions Into the Thought-World of the Pāli Discourses (2)
From Grasping to Emptiness – Excursions into the Thought-world of the Pāli Discourses (2) Anālayo © 2010 Anālayo Published by The Buddhist Association of the United States 2020 Route 301, Carmel, New York 10512 Printed in Taiwan Cover design by Laurent Dhaussy ISBN 978-0-615-25529-3 Introduction 3 1. Grasping / Upādāna 5 1.1 Grasping at Sensual Pleasures 5 1.2 Grasping at Views 7 1.3 Grasping at Rules and Observances 9 1.4 Grasping at a Doctrine of Self 10 1.5 The Five Aggregates [Affected by] Clinging 13 1.6 Grasping and Nibbāna 15 1.7 Freedom from Grasping 16 2. Personality View / Sakkāyadihi 19 2.1 Manifestations of Personality View 19 2.2 Removal of Personality View 24 3. Right View / Sammādihi 27 3.1 Wrong View 27 3.2 Right View and Investigation 29 3.3 Right View as the Forerunner of the Path 31 3.4 Arrival at Right View 33 3.5 Right View and the Four Noble Truths 34 4. Volitional Formations / Sakhārā 39 4.1 Sakhāras as an Aggregate 40 4.2 Sakhāras as a Link in Dependent Arising 44 4.3 Sakhāras in General 48 5. Thought / Vitakka 55 5.1 The Ethical Perspective on Thought 56 5.2 The Arising of Thought 57 5.3 The Vitakkasahāna-sutta 60 5.4 Vitakka in Meditation 64 5.5 Thought Imagery 66 6. Wise Attention / Yoniso Manasikāra 69 6.1 Wise ( Yoniso ) 69 6.2 Attention ( Manasikāra ) 72 6.3 The Implications of Wise Attention 72 6.4 The Importance of Wise Attention 78 7. -
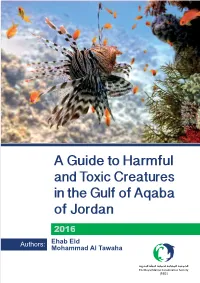
A Guide to Harmful and Toxic Creatures in the Goa of Jordan
Published by the Royal Marine Conservation Society of Jordan. P. O. Box 831051, Abdel Aziz El Thaalbi St., Shmesani 11183. Amman Copyright: © The Royal Marine Conservation Society of Jordan Reproduction of this publication for educational and other non- commercial purposes is authorized without prior written approval from the copyright holder provided the source is fully acknowledged. ISBN: 978-9957-8740-1-8 Deposit Number at the National Library: 2619/6/2016 Citation: Eid, E and Al Tawaha, M. (2016). A Guide to Harmful and Toxic Creature in the Gulf of Aqaba of Jordan. The Royal Marine Conservation Society of Jordan. ISBN: 978-9957-8740-1-8. Pp 84. Material was reviewed by Dr Nidal Al Oran, International Research Center for Water, Environment and Energy\ Al Balqa’ Applied University,and Dr. Omar Attum from Indiana University Southeast at the United State of America. Cover page: Vlad61; Shutterstock Library All photographs used in this publication remain the property of the original copyright holder, and it should not be reproduced or used in other contexts without permission. 1 Content Index of Creatures Described in this Guide ......................................................... 5 Preface ................................................................................................................ 6 Part One: Introduction ......................................................................................... 8 1.1 The Gulf of Aqaba; Jordan ......................................................................... 8 1.2 Aqaba; -

Spider Biology Unit
Spider Biology Unit RET I 2000 and RET II 2002 Sally Horak Cortland Junior Senior High School Grade 7 Science Support for Cornell Center for Materials Research is provided through NSF Grant DMR-0079992 Copyright 2004 CCMR Educational Programs. All rights reserved. Spider Biology Unit Overview Grade level- 7th grade life science- heterogeneous classes Theme- The theme of this unit is to understand the connection between form and function in living things and to investigate what humans can learn from other living things. Schedule- projected time for this unit is 3 weeks Outline- *Activity- Unique spider facts *PowerPoint presentation giving a general overview of the biology of spiders with specific examples of interest *Lab- Spider observations *Cross-discipline activity #1- Spider short story *Activity- Web Spiders and Wandering spiders *Project- create a 3-D model of a spider that is anatomically correct *Project- research a specific spider and create a mini-book of information. *Activity- Spider defense pantomime *PowerPoint presentation on Spider Silk *Lab- Fiber Strength and Elasticity *Lab- Polymer Lab *Project- Spider silk challenge Support for Cornell Center for Materials Research is provided through NSF Grant DMR-0079992 Copyright 2004 CCMR Educational Programs. All rights reserved. Correlation to the NYS Intermediate Level Science Standards (Core Curriculum, Grades 5-8): General Skills- #1. Follow safety procedures in the classroom and laboratory. #2. Safely and accurately use the following measurement tools- Metric ruler, triple beam balance #3. Use appropriate units for measured or calculated values #4. Recognize and analyze patterns and trends #5. Classify objects according to an established scheme and a student-generated scheme. -
Hobo Spider, Eratigena Agrestis, Is a Fig
Published by Utah State University Extension and Utah Plant Pest Diagnostic Laboratory ENT-86-08 Revised: February 2016 Hobo Spider Eratigena agrestis Ryan S. Davis Arthropod Diagnostician What You Should Know • Hobo spiders and related spiders build funnel-webs to catch prey. • In Utah, hobo spiders are frequently found indoors from August through October. • Recent scientific evidence suggests that hobo spiders do not have a necrotic bite. • The primary spider of health concern in Utah is the western black widow spider. • For more detailed information about the hobo spider, visit this page. he hobo spider, Eratigena agrestis, is a Fig. 1. Adult female hobo spider with egg sac (Ryan S. member of the funnel-web spider family Davis, Utah State University Extension). TAgelenidae (Fig. 1). Funnel-web spiders are long-legged, swift-running spiders that build funnels or tube-shaped retreats in turf, log piles, arachnologist who can examine the microscopic rock piles, and other areas around the home and characters necessary to determine the species. yard. The hobo spider is native to Europe, but was For the homeowner or non-expert, spiders with detected in the Pacific Northwest in 1936. Over banding around the legs can be eliminated as a time, the hobo spider migrated to other parts of potential hobo spider. the western United States. This species is distributed throughout northern Utah. Hobo spiders are non- Life Cycle aggressive and unlikely to bite. Their old common name, “aggressive house spider,” originated from The exact length of the hobo spider life cycle in a mis-interpretation of the species name “agrestis” Utah is not known, but it is suspected that hobos which actually means “of the field,” describing take 2 years to develop into adults.