Curing Children with Acute Lymphoblastic Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SGS-Safeguards 04910- Minimum Wages Increased in Jiangsu -EN-10
SAFEGUARDS SGS CONSUMER TESTING SERVICES CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 MINIMUM WAGES INCREASED IN JIANGSU Jiangsu becomes the first province to raise minimum wages in China in 2010, with an average increase of over 12% effective from 1 February 2010. Since 2008, many local governments have deferred the plan of adjusting minimum wages due to the financial crisis. As economic results are improving, the government of Jiangsu Province has decided to raise the minimum wages. On January 23, 2010, the Department of Human Resources and Social Security of Jiangsu Province declared that the minimum wages in Jiangsu Province would be increased from February 1, 2010 according to Interim Provisions on Minimum Wages of Enterprises in Jiangsu Province and Minimum Wages Standard issued by the central government. Adjustment of minimum wages in Jiangsu Province The minimum wages do not include: Adjusted minimum wages: • Overtime payment; • Monthly minimum wages: • Allowances given for the Areas under the first category (please refer to the table on next page): middle shift, night shift, and 960 yuan/month; work in particular environments Areas under the second category: 790 yuan/month; such as high or low Areas under the third category: 670 yuan/month temperature, underground • Hourly minimum wages: operations, toxicity and other Areas under the first category: 7.8 yuan/hour; potentially harmful Areas under the second category: 6.4 yuan/hour; environments; Areas under the third category: 5.4 yuan/hour. • The welfare prescribed in the laws and regulations. CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 P.2 Hourly minimum wages are calculated on the basis of the announced monthly minimum wages, taking into account: • The basic pension insurance premiums and the basic medical insurance premiums that shall be paid by the employers. -

Area/Temperature Limitation to Application of Vetiver System in China
Adequate Areas in China for the Application of Vetiver System Liyu XU (China Vetiver Network, Nanjing 210008) Abstract: Vetiver System was introduced into China by Mr. Grimshaw from the World Bank in 1988. Beginning from the Fuzhou Symposium in 1997, the system was applied for infrastructure protection in China. Since the Nanchang Symposium in 1999, it was extended quickly countrywide, and in particular, it was extensively applied and extended in South China. On the basis of reviewing successful research cases all over China, this paper deals with adequate areas where vetiver grasses can be planted, and lists related issues that should be further studied in the future. Key words: Vetiver system, Slope protection, Adequate planting area Environment protection is one of the most urgent missions faced by the contemporary world and also one of the basic tasks faced by the Chinese people in their economical construction and social development. Therefore, it should be considered as a basic state policy to be adhered in a long historic period. In its broad sense, environment protection consists of two fields, i.e., soil and water conservation as well as pollution control. To practice environment protection, various measures may be adopted. However, among those measures, bioengineering technology has been becoming favorite one frequently adopted by more and more people in recent years. Vetiver (Vetiveria zizanioides) is characterized by its strong stress tolerance, wide adoptability, quick growing vitality, huge biomass, highly developed root system with fantastic mechanical properties, and powerful soil bounding capacity as well as is to be easily planted and simply managed at very low cost. -

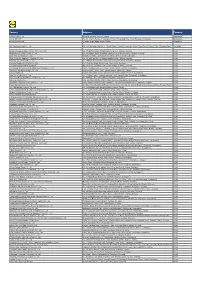
Shop Direct Factory List Dec 18
Factory Factory Address Country Sector FTE No. workers % Male % Female ESSENTIAL CLOTHING LTD Akulichala, Sakashhor, Maddha Para, Kaliakor, Gazipur, Bangladesh BANGLADESH Garments 669 55% 45% NANTONG AIKE GARMENTS COMPANY LTD Group 14, Huanchi Village, Jiangan Town, Rugao City, Jaingsu Province, China CHINA Garments 159 22% 78% DEEKAY KNITWEARS LTD SF No. 229, Karaipudhur, Arulpuram, Palladam Road, Tirupur, 641605, Tamil Nadu, India INDIA Garments 129 57% 43% HD4U No. 8, Yijiang Road, Lianhang Economic Development Zone, Haining CHINA Home Textiles 98 45% 55% AIRSPRUNG BEDS LTD Canal Road, Canal Road Industrial Estate, Trowbridge, Wiltshire, BA14 8RQ, United Kingdom UK Furniture 398 83% 17% ASIAN LEATHERS LIMITED Asian House, E. M. Bypass, Kasba, Kolkata, 700017, India INDIA Accessories 978 77% 23% AMAN KNITTINGS LIMITED Nazimnagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 1708 60% 30% V K FASHION LTD formerly STYLEWISE LTD Unit 5, 99 Bridge Road, Leicester, LE5 3LD, United Kingdom UK Garments 51 43% 57% AMAN GRAPHIC & DESIGN LTD. Najim Nagar, Hemayetpur, Savar, Dhaka, Bangladesh BANGLADESH Garments 3260 40% 60% WENZHOU SUNRISE INDUSTRIAL CO., LTD. Floor 2, 1 Building Qiangqiang Group, Shanghui Industrial Zone, Louqiao Street, Ouhai, Wenzhou, Zhejiang Province, China CHINA Accessories 716 58% 42% AMAZING EXPORTS CORPORATION - UNIT I Sf No. 105, Valayankadu, P. Vadugapal Ayam Post, Dharapuram Road, Palladam, 541664, India INDIA Garments 490 53% 47% ANDRA JEWELS LTD 7 Clive Avenue, Hastings, East Sussex, TN35 5LD, United Kingdom UK Accessories 68 CAVENDISH UPHOLSTERY LIMITED Mayfield Mill, Briercliffe Road, Chorley Lancashire PR6 0DA, United Kingdom UK Furniture 33 66% 34% FUZHOU BEST ART & CRAFTS CO., LTD No. 3 Building, Lifu Plastic, Nanshanyang Industrial Zone, Baisha Town, Minhou, Fuzhou, China CHINA Homewares 44 41% 59% HUAHONG HOLDING GROUP No. -

Results Announcement for the Year Ended December 31, 2020
(GDR under the symbol "HTSC") RESULTS ANNOUNCEMENT FOR THE YEAR ENDED DECEMBER 31, 2020 The Board of Huatai Securities Co., Ltd. (the "Company") hereby announces the audited results of the Company and its subsidiaries for the year ended December 31, 2020. This announcement contains the full text of the annual results announcement of the Company for 2020. PUBLICATION OF THE ANNUAL RESULTS ANNOUNCEMENT AND THE ANNUAL REPORT This results announcement of the Company will be available on the website of London Stock Exchange (www.londonstockexchange.com), the website of National Storage Mechanism (data.fca.org.uk/#/nsm/nationalstoragemechanism), and the website of the Company (www.htsc.com.cn), respectively. The annual report of the Company for 2020 will be available on the website of London Stock Exchange (www.londonstockexchange.com), the website of the National Storage Mechanism (data.fca.org.uk/#/nsm/nationalstoragemechanism) and the website of the Company in due course on or before April 30, 2021. DEFINITIONS Unless the context otherwise requires, capitalized terms used in this announcement shall have the same meanings as those defined in the section headed “Definitions” in the annual report of the Company for 2020 as set out in this announcement. By order of the Board Zhang Hui Joint Company Secretary Jiangsu, the PRC, March 23, 2021 CONTENTS Important Notice ........................................................... 3 Definitions ............................................................... 6 CEO’s Letter .............................................................. 11 Company Profile ........................................................... 15 Summary of the Company’s Business ........................................... 27 Management Discussion and Analysis and Report of the Board ....................... 40 Major Events.............................................................. 112 Changes in Ordinary Shares and Shareholders .................................... 149 Directors, Supervisors, Senior Management and Staff.............................. -
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -

Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020
Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020 Wei Zhang Xiamen University Jia Rui Xiamen University Xiaoqing Cheng Jiangsu Provincial Center for Disease Control and Prevention Bin Deng Xiamen University Hesong Zhang Xiamen University Lijing Huang Xiamen University Lexin Zhang Xiamen University Simiao Zuo Xiamen University Junru Li Xiamen University XingCheng Huang Xiamen University Yanhua Su Xiamen University Benhua Zhao Xiamen University Yan Niu Chinese Center for Disease Control and Prevention, Beijing City, People’s Republic of China Hongwei Li Xiamen University Jian-li Hu Jiangsu Provincial Center for Disease Control and Prevention Tianmu Chen ( [email protected] ) Page 1/30 Xiamen University Research Article Keywords: Hand foot mouth disease, Jiangsu Province, model, transmissibility, effective reproduction number Posted Date: July 30th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-752604/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/30 Abstract Background: Hand, foot, and mouth disease (HFMD) has been a serious disease burden in the Asia Pacic region represented by China, and the transmission characteristics of HFMD in regions haven’t been clear. This study calculated the transmissibility of HFMD at county levels in Jiangsu Province, China, analyzed the differences of transmissibility and explored the reasons. Methods: We built susceptible-exposed-infectious-asymptomatic-removed (SEIAR) model for seasonal characteristics of HFMD, estimated effective reproduction number (Reff) by tting the incidence of HFMD in 97 counties of Jiangsu Province from 2015 to 2020, compared incidence rate and transmissibility in different counties by non -parametric test, rapid cluster analysis and rank-sum ratio. -

GH 8 2 V Announcement
Geospatial Health 8(2), 2014, pp. 429-435 Spatial distribution and risk factors of influenza in Jiangsu province, China, based on geographical information system Jia-Cheng Zhang1, Wen-Dong Liu2, Qi Liang2, Jian-Li Hu2, Jessie Norris3, Ying Wu2, Chang-Jun Bao2, Fen-Yang Tang2, Peng Huang1, Yang Zhao1, Rong-Bin Yu1, Ming-Hao Zhou2, Hong-Bing Shen1, Feng Chen1, Zhi-Hang Peng1 1Department of Epidemiology and Biostatistics, School of Public Health, Nanjing Medical University, Nanjing, People’s Republic of China; 2Jiangsu Province Center for Disease Control and Prevention, Nanjing, People’s Republic of China; 3National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, People’s Republic of China Abstract. Influenza poses a constant, heavy burden on society. Recent research has focused on ecological factors associated with influenza incidence and has also studied influenza with respect to its geographic spread at different scales. This rese- arch explores the temporal and spatial parameters of influenza and identifies factors influencing its transmission. A spatial autocorrelation analysis, a spatial-temporal cluster analysis and a spatial regression analysis of influenza rates, carried out in Jiangsu province from 2004 to 2011, found that influenza rates to be spatially dependent in 2004, 2005, 2006 and 2008. South-western districts consistently revealed hotspots of high-incidence influenza. The regression analysis indicates that rail- ways, rivers and lakes are important predictive environmental variables for influenza risk. A better understanding of the epi- demic pattern and ecological factors associated with pandemic influenza should benefit public health officials with respect to prevention and controlling measures during future epidemics. -

Property Sales Company Information
Quarterly Newsletter 4th Quarter 2017 Property Sales Contracted sales for the year of 2017 recorded at approximately RMB10.37 billion, up 123% year-on- year; contracted GFA aggregated approximately 1,180,000 sq.m., exceeding sales target and gaining a foothold in the billion-dollar sales club. RMB(bn) Contracted sales Sq.m(‘000) Contracted GFA 10 100 10.37 1177 5 50 4.65 460 0 0 FY2016 FY2017 FY2016 FY2017 Company Information Land acquisition . In December, Jiayuan International further acquired 51% equity Location of Jiayuan Huafu interest of Shenzhen Songling Industrial Co., Ltd., owner of a parcel of land planned for residential and commercial use located at Fanshen Avenue, Bao’an District in Shenzhen. In November, Jiayuan International acquired 2 property development projects in Yangzhou Guangling District— Yangzhou Guifu, located within the high-end living circle along the canal bund as planned by the Yangzhou Government; Yangzhou Huafu, surrounded by abundant educational resources and an 8-minute drive away from the city’s central commercial zone—allowing the Group to further reinforce its leadership position in Jiangsu Province. Bao’an Project Jiayuan Guifu Jiayuan Huafu Total Gross City Land Area Acquisition Cost Province Project Floor Area Quarter (District) (sq.m) (RMB mn) (sq.m) Bao’an (TBC) Guangdong District, 4,281 32,966 930* 4th Shenzhen Guangling Jiayuan Guifu Jiangsu District, 211,695 578,491 2450 4th Yangzhou Jiayuan Huafu Total: 611,457 3380 *RMB610 mn paid in 2016 1 Quarterly Newsletter 4th Quarter 2017 Company News December’s contracted sales saw an increase of 450% year-on-year . -

NEGARA BAGIAN Cina Pabrik Pengolahan
Tanggal Validitas dari NEGARA Cina 05/09/2020 00133 BAGIAN Pabrik pengolahan Tanggal publikasi 05/09/2020 Daftar yang berlaku Nomor persetujuan Nama Kota Daerah Aktivitas Ucapan Tanggal permintaan 00631765 Qixian Zengwei Mealworm Insect Breeding Cooperatives Qixian Shanxi CAT3 06/11/2014 Professional 0400PF012 BAODING XINJIE BIOTECHNOLOGY CO,LTD Baoding Hebei CAT3 16/12/2019 0400ZC0001 Cangzhou Bee Industry Co.,Ltd Cangzhou Hebei CAT3 30/04/2020 0400ZC0013 HEBEI YUANDA APICULTURE CO.,LTD Hengshui Hebei CAT3 08/06/2020 0400ZC0017 HEBEI CERA RICA INDUSTRY AND TRADE CO.,LTD. Hengshui Hebei CAT3 08/06/2020 0400ZC0023 QINGYUAN COUNTY HENGYE BRUSH MANUFACTURING Baoding Hebei CAT3 08/06/2020 CO.,LTD 0400ZC0025 YIXIAN HUANGSHAN HONEYBEE PRODUCT CO.,LTD. Baoding Hebei CAT3 08/06/2020 0400ZC0044 QINGHE COUNTY LEESON FLUFF PLANT Xingtai Hebei CAT3 15/10/2020 0400ZC0047 HEBEI YIGANYA CASHMERE PRODUCT CO.,LTD Xingtai Hebei CAT3 15/10/2020 0400ZC0061 Hebei Xushi Beeswax Co.,Ltd Cangzhou Hebei CAT3 27/08/2021 0501PF006 SHANXI DINGSHUO AGRICULTURAL PRODUCT CO.,LTD Xinzhou Shanxi CAT3 21/07/2020 0503PF014 Datong HaiFa Biological Technology Co., Ltd Datong Shanxi CAT3 14/02/2020 1100AF001 BEIJING BEISHUI FOODINDUSTRYCO.,LTD. Tongzhou Beijing CAT1 21/12/2016 1200AF001 TIANJIN OCEAN PAL CAROL BIOTECH CO., LTD. Tianjin Tianjin CAT3 1 / 13 Daftar yang berlaku Nomor persetujuan Nama Kota Daerah Aktivitas Ucapan Tanggal permintaan 1200AF005 TIAN JIN DONG JIANG FOOD CO. LTD Tianjin Tianjin CAT3 03/05/2011 1200AF006 Marukyu (Tianjin) Fishing Tackle CO.\,Ltd Tianjin Tianjin CAT3 1200AF007 Tianjin Intra Technologies Co. Ltd. Tianjin Tianjin CAT3 03/05/2011 1200AF010 KYORIN AQUATIC INDUSTRIES(TIANJIN)CO.,LTD. -

Translating Science Into Survival
Scientific Report 2018 Scientific Report 2018 www.stjude.org/scientificreport 262 Danny Thomas Place Memphis, TN 38105 Physician Referral Service 866.278.5833 Translating Science General Information 901.595.3300 into Survival Behind the Cover The scientific image on the cover is a fluorescence image of pyramidal neurons in the auditory cortex. The brain can modify the structure and function of neuronal connections in response to sensory experiences. This ability is known as neuroplasticity. Stanislav S. Zakharenko, MD, PhD (Developmental Neurobiology), and his Faculty Editorial Board colleagues are investigating the role of neuroplasticity in the Terrence L. Geiger, MD, PhD Nickhill Bhakta, MD, MPH auditory cortex during learning and how dysfunction in that part of Michael A. Dyer, PhD the brain can cause catastrophic neurologic or psychiatric diseases. Alberto S. Pappo, MD Leslie L. Robison, PhD Carlos Rodriguez-Galindo, MD Stephen W. White, DPhil Stanislav S. Zakharenko, MD, PhD Editoral Direction Angela J. McArthur, PhD, ELS Creative Direction Jerry L. Harris Photography Peter Barta Seth Dixon Ann-Margaret Hedges Jere Parobek Prepared by Departments of Scientific Editing and Biomedical Communications St. Jude Children’s Research Hospital and ALSAC are registered trademarks. ST. JUDE INVESTIGATORS, BACKED BY EXTRAORDINARY RESOURCES AND SUPPORT TEAMS, HAVE THE FREEDOM TO FOCUS ON MAKING BIG DISCOVERIES. OUR CULTURE AND CAMPUS FOSTER THE FREE EXCHANGE OF IDEAS AMONG SCIENTISTS AND CLINICIANS TO PROMOTE CREATIVE, COLLABORATIVE SCIENCE. Privileged communication. Copyright © 2018 St. Jude Children’s Research Hospital. No part of this communication may be cited, reproduced, stored in a retrieval system, or transmitted by electronic or other means without prior written permission of the President and CEO and the appropriate investigator. -

A History of St. Judes Children's Research Hospital (.Pdf)
British Journal of Haematology, 2003, 120, 1–7 Historical Review F A HISTORY OF ST JUDE CHILDRENAPOS;S RESEARCH HOSPITAL The entertainer Danny Thomas founded St Jude Children’s Cardinal Samuel Stritch, then Catholic archbishopO of Research Hospital in Memphis, Tennessee, in 1960 and Chicago, whom Thomas had met when the former was a opened its doors in 1962 to serve children in need through bishop in Toledo. Stritch dissuaded him from building a research and medical care. Dr Donald Pinkel, the first shrine, saying there were plenty already.O They subsequently director, initiated the ÔTotal TherapyÕ series of studies of agreed that a children’s hospital for the needy was a better acute lymphoblastic leukaemia (ALL), which subsequently tribute, something like the Shriner’s hospitals in the USA, demonstrated that the disease was curable in a significant where disabled children received free care. Thomas favoured percentage of children. Pioneering studies in childhood locating the hospital in ChicagoR where he got his show cancer and high-quality basic biological research served as business start. Stritch persuaded him that Chicago already key ingredients in creating an environment of scientific had good children’s facilities and that he should find a place excellence and interdisciplinary activity. During its in greater need. StritchP suggested Memphis, Tennessee, 40 years, the institution has grown in scientific stature where he had been a parish priest and, being a practical and programmatic depth, both made possible by the skill of sort, because he was a good friend of a civic leader in its investigators, and by its physical and financial growth. -

A Legacy of Hope for Young Leukemia Patients
For more on the Giants of Cancer Care®, visit Giants.OncLive.com Joseph V. Simone, MD An Innovator in Pediatric Cancer Care Joseph V. Simone, MD, is best known for leading the research efforts that resulted in the first curative com- bination treatment for certain pediatric patients with acute lymphoid leukemia. Under his leadership, the St. Jude Children’s Research Hospital in Memphis, Tennessee, was designated the first and only National Cancer Institute cancer center dedicated to children. He was honored in the Pediatric Oncology category with a 2017 Giants of Cancer Care® award. A Legacy of Hope for Young Leukemia Patients BY ANGELICA WELCH IN THE 1960S, PROGRAMS for treating the kids will understand. It’s tricky, though, to find cures for more children. “When you get leukemia were few and far between—especially because you can scare them, the parents are one like that, you get very, very anxious to get for children. The disease was just beginning scared—and sometimes I am scared. But I think more. That pushed us on,” he says. to be understood, and rules and regulations [having] that group—parents, doctor, our superb for taking care of both adult and pediatric nurses, and the patients involved—is something A MENTOR patients were underdeveloped and inefficient, [for which] we do not provide enough training When asked about the great strides made in as the first treatment for systemic cancers had for people,” Simone admits. the 1960s and 1970s for childhood leukemia, been developed only a decade earlier. St. Jude’s prominence grew with Simone’s Simone credits his mentor, Donald Pinkel, MD.