Carrying Forward a Proud Family Tradition of Philanthropy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Brochure
it begins with a healthy MEDICAL BREAKTHROUGHS AT UCLA UCLA Medical Center opens The first open-heart surgery in the UCLA researchers develop the fi rst western United States is performed techniques for fetal monitoring. at UCLA Medical Center. 1955 1956 1958 UCLA HEALTH UCLA Health. It’s a partnership among you and our doctors, researchers, nurses and staff, who are dedicated to making a difference in your life on a daily basis — all working together to advance the field of medicine, while offering you the finest personal care and treatments available today. People seek us out at the most vulnerable times of their lives. That is why, with our foundation of outstanding academic medicine, cutting-edge technologies and first-rate facilities in Westwood and Santa Monica, we pledge to the 2.5-million patients who enter our medical offices and the more than 100,000 patients who are admitted to our hospitals each year that we will treat each and every one as we would members of our own families. UCLA Health. It begins with you. UCLA Health: Accolades and Achievements Ronald Reagan UCLA Medical Center ranks as the No. 1 UCLA Medical Center, Santa Monica is named a medical center in the western U.S. and No. 5 in the nation distinguished hospital for clinical excellence Mattel Children’s Hospital UCLA ranks among the top UCLA Medical Group awarded Gold Level Achievement U.S. pediatric hospitals for clinical quality by the California Department of Managed Health Care Stewart and Lynda Resnick Neuropsychiatric Hospital at UCLA ranks No. 1 in the West and among the UCLA is a national leader in organ transplantation top-10 in the country UCLA Jonsson Comprehensive Cancer Center is Ophthalmology services at UCLA Stein Eye and Doheny designated as one of only 40 U.S. -

Press Kit (Pdf)
IMAGES IMAGES PROJECT DESCRIPTION The new UCLA Health Training Center is currently in construction in El Segundo, CA. The new complex will house the business and basketball operations as well as a full NBA training center with an exhibition court and arena seating. The new 120,000 square-foot facility is both striking and noteworthy. The project was designed by noted Detroit-based sports and entertainment architect ROSSETTI in conjunction with the Los Angeles architectural office of Perkins + Will. Highlights of the building design include a Sponsor’s Gallery which will be accessible to the public, separate office and game-day entries, separate and secure player parking and entry, and an employee hub/internet café. The new building is specifically designed to facilitate high level training. The state-of-the-art facility is all encompassing for the athlete. The 80,000 square-foot first floor includes a double court gymnasium with on-court smart board and video displays for strategic planning and playbacks; plyometric training areas; weight and conditioning gym that opens to the court; a video theater/screening room directly adjacent to the player lounge; an indoor-outdoor lounge fully outfitted for video, sound and a myriad of digital connections; a barber shop; a player kitchen and training table (as well as an adjacent commercial kitchen directed by a nutritionist); a player quiet room outfitted with blue light spectrum lighting; a state-of-the- art training room with multiple whirlpools, two plunge pools, a resistance pool and cryogenics chamber; a separate training area for the D-Fenders Development League team and all the necessary accessory spaces to support a high level Training, Recovery and Rest program. -

Stein and Doheny Eye Institutes Broaden Patient Access to Eye Care
Spring 2014 Volume 32 Number 2 EYE Stein and Doheny Eye Institutes Broaden Patient Access to Eye Care he greater Los Angeles region is reaping immediate ben- efits from the historic alliance of the UCLA Stein Eye TInstitute and the Doheny Eye Institute: Two Doheny Eye Center UCLA locations—one in Arcadia and the other COUNTY Olive View-UCLA Medical Center in Orange County—are now open and seeing patients, and a SYLMAR third Doheny Eye Center UCLA is set to open this summer in Pasadena. LOS ANGELES The three Doheny Eye Center UCLA locations join the prestigious Stein Eye Institute in Westwood, the Stein Doheny Eye Center UCLA VENTURA COUNTY PASADENA Eye Center–Santa Monica, and the UCLA Department of Ophthalmology-affiliated teaching satellite hospitals: Veterans Affairs Greater Los Angeles Healthcare Center at West Los Stein Eye Institute UCLA Angeles and Sepulveda, Harbor-UCLA Medical Center, and WESTWOOD Doheny Eye Center UCLA Olive View-UCLA Medical Center. ARCADIA “From the westside to the eastside and south to Orange County, patients throughout Los Angeles and neighbor- ing regions now have access to the finest ophthalmologic Veteran's Affairs care available,” says Chairman of the UCLA Department of Stein Eye Center UCLA Healthcare Center SANTA MONICA WEST LOS ANGELES Ophthalmology and Director of the Stein Eye Institute, Bartly J. Mondino, MD. LOS ANGELES COUNTY A Shared Tradition of Excellence ORANGE COUNTY Both Doheny and Stein Eye have a long tradition of excellence and are consistently ranked in the top 10 of the U.S. News & Harbor-UCLA Medical Center World Report Best Hospital Rankings for ophthalmology. -

Annual Report 2019-2020
ENDOWMENT IN ACTION • 2020 DEAR FRIENDS, For more than 100 years, UCLA has met challenges with resolve and innovation and answered injustice with reflection and action. 2020 has called on us to do that more than any year in recent memory. Thanks to our stellar faculty, students, and staff — and in large part to your generosity — we are rising to the occasion. When you give to grow UCLA’s endowment, you are thinking ahead and allowing UCLA to look forward. These funds facilitate the university’s exceptional work and bolster us in exceptionally difficult times such as those we face now. Enclosed are a report on the performance of the endowed funds to which you have contributed, information about the university’s endowment, and messages from leaders of The UCLA Foundation and the UCLA Investment Company. Thank you for all you do for UCLA. Your leadership, advocacy, and philanthropy have helped solidify the university’s standing as the nation’s number one public university and a renowned leader in education, research, and service. Sincerely, Gene D. Block Chancellor 1 A NOTE FROM FOUNDATION LEADERSHIP Our vision at The UCLA Foundation is to be the partner of choice to UCLA leadership, students, and donors. An important aspect of being an effective partner is providing leadership and resources when challenges are most intense. The year 2020 has mandated that The UCLA Foundation be thoughtful, swift, and responsive, elevating its influence when circumstances required it the most. Additionally, thanks in large part to our donor base, our university is thriving and making the world a better place. -

Innovation Update
Newsletter Fall 2018 Innovation Update In this Issue, you will find: Message from Desert Horse-Grant INNOVATION AWARDS, COMPETITIONS, HONORS UCLA Mattel Children’s Hospital Named One of Nation’s Most Innovative FDA Grant Awarded to UCLA Health and collaborators for MedTech Innovation VentureWell Grant for Sustainable Design and Prototyping in Medical Technology Innovation awarded to UCLA Biodesign Program UCLA Computer Science Innovation Fund Winner INNOVATION IN PATIENT AND SYSTEMS SERVICES Smartphones for Good Health Records on iPhone® App Available to UCLA Health Patients Using Mobile to Monitor Depression Clinical Care Offering — Pediatrics CAR T-cell Therapy Clinical Trial Offering — Gene Therapy Cancer Treatment INNOVATION AS A LEARNING HEALTH SYSTEM Advances in Treatment Planning — 3D Printing and More Effective Cardiovascular Surgeries Performance Improvement Projects INNOVATION WITH BIOMEDICAL TECHNOLOGIES Metabolism-focused Startup Aims to Shorten Time Between Scientific Insight and Therapies UCLA Bioengineers Use Magnetic Force to Manage Pain — Early Findings with Mechanoceuticals UPCOMING PROPOSALS, MEETINGS AND DEADLINES Accelerators on Campus Magnify at UCLA CNSI Anderson Venture Accelerator University of California Pitch Day — Upcoming Event Nursing: New Knowledge, Innovations and Improvements Council Meeting UCLA Bioscience Innovation Day — Upcoming Event TDG Biopharmaceuticals — Staff Spotlight Message from Desert Horse-Grant Dear UCLA Health Community and Supporters, UCLA Health achieved important innovation milestones during the past quarter, in- cluding the support of Health Records on iPhone®. These records combine informa- tion from hospitals, clinics and the existing Apple® Health app to make it easy for patients to see their available medical data from multiple providers, whenever they choose. We are committed to empowering patients, and now offer anytime access to their medical records from all UCLA Health hospitals and clinics through the myUCLA- Health web or mobile applications. -

EMERITI Newsletter Fall 2020 UCLA Emeriti Association, Our 53Rd Year Vol
UCLA EMERITI Newsletter Fall 2020 UCLA Emeriti Association, Our 53rd Year Vol. 34, No. 1 PRESIDENT’S MESSAGE UCLA will continue to confer emeritus/a status on all retiring members of the Academic Senate, Dear Fellow Emeriti, Re- it is believed that this criterion should be com- tired Librarians, and mon to all the UC campuses. Letters in support Spouses: of a return to the original language identifying criteria for conferral of emeritus/a status were I know I speak for most sent to the Chair of the Academic Council, rep- of you, when I say that resenting all UC Academic Senates, who formal- UCLA has been an im- ly requested return to the previous wording. portant part of our lives, both professionally and A second issue was a proposal from the Office personally. The Emeriti of the President to consolidate a number of Association, which repre- emeriti/retiree health plans into a new plan. UC sents retired faculty, li- Emeriti and Retiree Associations did not feel brarians, and their spous- that they had been adequately consulted. This es, fosters continuing connections between issue was raised at a meeting of the Regent’s UCLA colleagues through its newsletter, and, Health Services Committee. The Council of UC normally, through after lunch programs, quar- Emeriti Associations (CUCEA) and Council of UC terly dinners, and an annual arts & crafts fair Retiree Associations (CUCRA) protested this (the current pandemic has required that events perceived lack of adequate consulation. As a now be virtual rather than in-person). The pro- result, the new plan replaced only one of the grams are interesting and informative, whether previous health-care plans and is considered a it be about a career in astrophysics, the current test for possible future changes in emeriti/ political situation in Turkey and the Middle retiree health-care plans. -
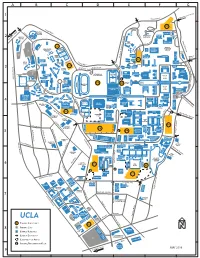
G F E D C B a 1 2 3 4 5 6 7
A B C D E F G 1 Sunset Blvd. Charing Cross Road S FERNALD R u o ns CENTER et y EAST ay EASTON Bl c MELNITZ Bellagio Drive v e w SOFTBALL d. MELNITZ ee STADIUM D r r BROAD F i UNIVERSITY MACGOWAN 5 h v ART EAST 2 0 KRIEGER t e RESIDENCE r 4 CENTER o CENTER o T N H e e UCLA t i v v r MACGOWAN l i i LAB r u g r SCHOOL Co a D CRA re D o m r yca d e S g v A n e MURPHY v u n e o SCULPTURE e SUNSET CANYON SPIEKER YOUNG n Pool Y D RECREATION AQUATICS RESEARCH GARDEN u . AMPHITHEATER e 11 CENTER GSEIS E LIBRARY GUEST Pool s HOUSE e l 10 SUNSET r ROSENFELD NC TENNIS a LIBRARY STUDENT h BUNCHE COURTS CENTER Wyton Pool C PUBLIC AFFAIRS Drive HEDRICK MULLIN CORNELL SUMMIT S ART C HITCH CANYON un LIBRARY h SUITES POINT COURTSIDE se ANDERSON a t Bl W KORN rl HEDRICK vd. e ROLFE e s ENTRE CAMPBELL LU s V t GOLD VALLE E 3 e w COLLINS PRENEURS . DELTA har Drive North PERLOFF t SUNSET C les E o Y e . g TERRACE VILLAGE Youn o o r d u a LAW n n P g l LIBRARY Pool A a COVEL FOWLER D z v 15 SYCAMORE INTRAMURAL a MUSEUM SOCCER KAUFMAN r e TENNIS RIEBER ROYCE DICKSON LAW i PLAYING FIELD v n FIELD COURTS HAINES e u COURT DODD e J M TERRACE NORTH E SPROUL a JANSS s ORNAMENTAL t RIEBER NW STEPS HORTICULTURE CAMPUS SHAPIRO VISTA WILSON FOUNDERS ROCK AUD PLAZA FOUNTAIN FLAG MARSHALL SAXON CARNESALE FIELD DRAKE SUITES COVE DICKSON 17 D RIEBER JOHN WOODEN STUDENT POWELL COURT e HALL SPROUL CENTER ACTIVITIES LIBRARY SOUTH MURPHY N ASHE ev LANDING CENTER e SPROUL Drive Pool A 13 HUMANITIES SOUTHERN CEDAR BRUIN BRUIN WALK PLAZA BUS REGIONAL HOLLY SCHOENBERG ATERMINAL LIBRARY GARDENIA PHYSICS MUSIC C LA TENNIS Strathmore Drive FACILITY DOGWOODDE NEVE h CENTER MORGAN & BUILDING 4 a ASTRONOMY r KERCKHOFF OSTIN BIRCH le EVERGREEN ACACIA s ACKERMAN KNUDSEN e DE NEVE PAULEY venu WESTWOOD E ACOSTA UNION y A COMMONS . -

Annual Financial Report
ANNUAL FINANCIAL REPORT 2011 2012 REED HUTCHINSON Photography CONTENTS Letter from Chancellor Gene D. Block 01 Highlights 04 ANNUAL FINANCIAL REPORT ANNUAL Management’s Discussion and Analysis 06 UCLA Transmittal Letter 23 Financial Statements 24 2011 - 2012 | - 2012 2011 Notes to Financial Statements 29 Letter from Chancellor Gene D. Block The 2011–12 academic year was filled with outstanding accomplishments by UCLA’s students, fac ulty and staff. It also marked my fifth year as UCLA’s chancellor. During that half decade, which has coincided with one of the most challenging periods for public funding of higher education in our nation’s history, our campus has thrived. Today, UCLA is stronger than ever and enjoys unprecedented respect and acclaim around the world. Todd Ceney/UCLA Photography Todd Thanks to our planning of the past several years and an extraordinary collective effort that is not only campus-wide but also extends to parents, alumni and donors, UCLA is well positioned to continue our upward trajectory toward our centennial in 2019 and beyond — despite the State of California’s continued disinvestment in our great institution. Academic and Research Excellence. UCLA’s reputation, nationally and interna- tionally, continued to soar in 2011–12. Third-party rankings illustrate the regard in which an institution is held, even though they are imperfect measures of a uni- versity’s excellence, and we were especially proud of our standing in three surveys. Washington Monthly, which publishes rankings based on cutting-edge scholarship, commitment to service and access for low-income students, placed UCLA No. 2 in the U.S. -

LASEC 2018 Master Calendar
2018 LASEC MAJOR SPORTS & ENTERTAINMENT EVENTS CALENDAR NCAA Men’s Basketball NBA All-Star Banc of California West Regional STAPLES Center Stadium Opening STAPLES Center February 16–18, 2018 2018 March 22 and 24, 2018 www.LASEC.net WE MEAN BUSINESS MESSAGE FROM THE PRESIDENT We are pleased to present our 2018 Los Angeles Sports & Entertainment Commission (LASEC) Major Sports & Entertainment Events Calendar. With a growing number of major events held throughout the calendar year, it’s easy to lose track of the dates and locations. The 2018 LASEC Major Sports & Entertainment Events Calendar is designed to help you with planning for the future. It includes events happening in Los Angeles and also major out-of-town events (like the Super Bowl and the U.S. Open). For easy use, this calendar includes a list by name of the events we are tracking and is also sorted by month, so you can easily check to make sure you aren’t planning an event on a date that is already taken. We plan to update the calendar each year, so please do not hesitate to share feedback or make recommendations to help make this a more useful tool in the future. Founded in 1995, the Los Angeles Sports & Entertainment Commission (LASEC) partners with the City of Los Angeles to bring major sporting and entertainment events to Los Angeles, like the NBA All-Star, the GRAMMY Awards, the College Football Playoff National Championship, the Super Bowl and many others. These events have a significant economic impact on the local economy and continue to spotlight Los Angeles as the Entertainment Capital of the World. -

An Insider's Guide to Benefits & Retirement Programs
UCLA Health An Insider's Guide to Benefits & Retirement Programs Welcome to UCLA! This Insider’s Guide to UC’s Benefits and Retirement Programs will provide helpful hints, enrollment guidelines and resources that will assist you in selecting your Health & Welfare Benefits. Selecting health benefits is a personal choice and there are numerous resources available to help you make the best choices. To learn about each option in greater detail and gain valuable information to help you make your selection: Review your welcome kit: http://ucnet.universityofcalifornia.edu/forms/pdf/welcome-kit.pdf Visit UCnet: http://ucnet.universityofcalifornia.edu/compensation-and-benefits/ The information provided to you in this presentation is intended as a general overview. For more detailed information, visit ucnet.universityofcalifornia.edu for UC benefits publications, UC-sponsored plans provider directories, drug formularies and more. Call the plan (or see their website) for specific benefits, provider information, and plan booklets. Your Benefits Team can also provide assistance. Important Points of Contact Health Systems vs. Campus UCLA has two HR groups that support the employees within the organization, the Medical Center and Campus. Please review the options below to find your appropriate point of contact in case you need assistance. If you work for any of the following groups, If you work for either of the following groups, Centralized Human Resources for the Campus HR is your processing center and Medical Center is your processing center your -

Partners in Health
Partners in Health Engaging in the Community Our Commitment to the Community To truly improve lives, UCLA faculty, researchers and students must leave the confines of the campus and connect directly with people in their communities. That is the goal of our community engagement initiative: to engage with a diverse group of partners to improve the health of the broader community. Today, community engagement is, with teaching, patient care and research, among the core missions of UCLA Health System and the David Geffen School of Medicine at UCLA. By partnering with organizations outside of UCLA, we: • Gain access to venues to train the next generation of healthcare professionals • Learn about our regional communities and how best to improve the health of the people living in those communities Our community engagement does not have geographic boundaries. It is all of those people to whom we provide patient care. It involves people working within our service-learning and research partnerships; and it involves our donor community, whose creativity and generosity are essential to helping UCLA maintain excellence and stay nationally competitive. For more on our community engagement projects visit: uclahealth.org/community Table of Contents Breathmobile......................................................................................................... 4 CARE Center ........................................................................................................... 5 Care Harbor ..................................................................................................................6 -

Annualreport 1819 FULL.Pdf
ANNUAL REPORT – INTRODUCTION Dear Bruins, Our athletic department began the 2018-19 school year with the grand opening of Wallis Annenberg Stadium on Aug. 17, 2018, as the women’s soccer team earned win No. 1 of the season for the Bruins. Since then, we collected 353 more wins in all competitions for a final head-to-head record of 354-125-2, compiling a 74% win percentage across all our sports. To put that number in context, the Dodgers set an L.A. franchise record for wins in 2017, when their 104 victories equated to a 64% win percentage. Along the way, we had more special moments than I can list on this page, but it’s only appropriate to start with national championships for the beach volleyball and softball programs. These two teams reached the peak of competitive greatness in 2019, and we could not be more proud of Stein, Jenny, Kelly, Kirk, Lisa, the student-athletes, and the supporting staffs for these accomplishments. While not every team could end their season with a victory, congratulations are also in order for the gymnastics, men’s water polo and women’s water polo night of the year better captures our purpose. Earlier Frankie Amaya was the top selection in the MLS Draft, teams for their Top 3 finishes. In addition, our women’s in the school year, we announced a department-wide marking the sixth time in which a Bruin went first soccer and women’s tennis teams had runs to the Elite Graduation Success Rate of 90% for the first time in overall.