6127.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
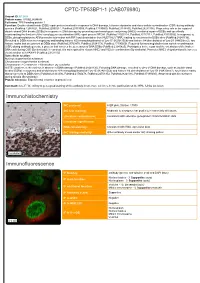
CPTC-TP53BP1-1 (CAB079980) Immunohistochemistry Immunofluorescence
CPTC-TP53BP1-1 (CAB079980) Uniprot ID: Q12888 Protein name: TP53B_HUMAN Full name: TP53-binding protein 1 Function: Double-strand break (DSB) repair protein involved in response to DNA damage, telomere dynamics and class-switch recombination (CSR) during antibody genesis (PubMed:12364621, PubMed:22553214, PubMed:23333306, PubMed:17190600, PubMed:21144835, PubMed:28241136). Plays a key role in the repair of double-strand DNA breaks (DSBs) in response to DNA damage by promoting non-homologous end joining (NHEJ)- mediated repair of DSBs and specifically counteracting the function of the homologous recombination (HR) repair protein BRCA1 (PubMed:22553214, PubMed:23727112, PubMed:23333306). In response to DSBs, phosphorylation by ATM promotes interaction with RIF1 and dissociation from NUDT16L1/TIRR, leading to recruitment to DSBs sites (PubMed:28241136). Recruited to DSBs sites by recognizing and binding histone H2A monoubiquitinated at 'Lys-15' (H2AK15Ub) and histone H4 dimethylated at 'Lys-20' (H4K20me2), two histone marks that are present at DSBs sites (PubMed:23760478, PubMed:28241136, PubMed:17190600). Required for immunoglobulin class-switch recombination (CSR) during antibody genesis, a process that involves the generation of DNA DSBs (PubMed:23345425). Participates in the repair and the orientation of the broken DNA ends during CSR (By similarity). In contrast, it is not required for classic NHEJ and V(D)J recombination (By similarity). Promotes NHEJ of dysfunctional telomeres via interaction with PAXIP1 (PubMed:23727112). Subcellular -

RIDDLE Immunodeficiency Syndrome Is Linked to Defects in 53BP1-Mediated DNA Damage Signaling
RIDDLE immunodeficiency syndrome is linked to defects in 53BP1-mediated DNA damage signaling Grant S. Stewart*†, Tatjana Stankovic*, Philip J. Byrd*, Thomas Wechsler‡, Edward S. Miller*, Aarn Huissoon§, Mark T. Drayson¶, Stephen C. West‡, Stephen J. Elledge†ʈ, and A. Malcolm R. Taylor* *Cancer Research UK, Institute for Cancer Studies, Birmingham University, Vincent Drive, Edgbaston, Birmingham B15 2TT, United Kingdom; ‡Cancer Research UK, Clare Hall Laboratories, London Research Institute, South Mimms, Hertfordshire EN6 3LD, United Kingdom; §Department of Immunology, Birmingham Heartlands Hospital, Birmingham, B9 5SS, United Kingdom; ¶Division of Immunity and Infection, Birmingham University Medical School, Vincent Drive, Edgbaston, Birmingham B15 2TT, United Kingdom; and ʈHoward Hughes Medical Institute, Department of Genetics, Harvard Partners Center for Genetics and Genomics, Harvard Medical School, 77 Avenue Louis Pasteur, Boston, MA 02115 Contributed by Stephen J. Elledge, September 6, 2007 (sent for review July 6, 2007) Cellular DNA double-strand break-repair pathways have evolved with an alternative constant region (e.g., ␣, ␥, ) to generate to protect the integrity of the genome from a continual barrage of different Ig isotypes e.g., IgA, IgG, and IgE (2). potentially detrimental insults. Inherited mutations in genes that During the process of CSR, it has been hypothesized that two control this process result in an inability to properly repair DNA closely positioned single-stranded DNA nicks result in the damage, ultimately -

WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT (51) International Patent Classification: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, C12Q 1/68 (2018.01) A61P 31/18 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, C12Q 1/70 (2006.01) HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/US2018/056167 OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (22) International Filing Date: SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 16 October 2018 (16. 10.2018) TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, (30) Priority Data: UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, 62/573,025 16 October 2017 (16. 10.2017) US TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, ΓΕ , IS, IT, LT, LU, LV, (71) Applicant: MASSACHUSETTS INSTITUTE OF MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, TECHNOLOGY [US/US]; 77 Massachusetts Avenue, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, Cambridge, Massachusetts 02139 (US). -

PRODUCT INFORMATION TP53BP1 BRCT Domains (Human Recombinant) Item No
PRODUCT INFORMATION TP53BP1 BRCT domains (human recombinant) Item No. 14171 • Batch No. XXXX Overview and Properties Synonyms: Tumor Protein p53 binding Protein 1, Tumor Suppressor p53-binding Protein 1 Source: Recombinant human N-terminal GST-tagged protein expressed in E. coli amino acids 1,717-1,972 (N- and C-terminal truncation) Uniprot No.: Q12888 Batch specific information can be found on the Batch Specific Insert or by contacting Technical Support Molecular Weight: 55.1 kDa Storage: -80°C (as supplied) Stability: ≥6 months Purity: batch specific Supplied in: 50 mM Tris-HCl, pH 8.0, containing 150 mM sodium chloride and 20% glycerol Protein Concentration: batch specific mg/ml Image(s) 1 2 3 4 250 kDa · · · · · · · 150 kDa · · · · · · · 100 kDa · · · · · · · 75 kDa · · · · · · · 50 kDa · · · · · · · 37 kDa · · · · · · · 25 kDa · · · · · · · 20 kDa · · · · · · · Lane 1: MW Markers Lane 2: TP53BP1 BRCT domains (1 µg) Lane 3: TP53BP1 BRCT domains (2 µg) Lane 4: TP53BP1 BRCT domains (5 µg) Representative gel image shown; actual purity may vary between each batch. WARNING CAYMAN CHEMICAL THIS PRODUCT IS FOR RESEARCH ONLY - NOT FOR HUMAN OR VETERINARY DIAGNOSTIC OR THERAPEUTIC USE. 1180 EAST ELLSWORTH RD SAFETY DATA ANN ARBOR, MI 48108 · USA This material should be considered hazardous until further information becomes available. Do not ingest, inhale, get in eyes, on skin, or on clothing. Wash thoroughly after handling. Before use, the user must review the complete Safety Data Sheet, which has been sent via email to your institution. PHONE: [800] 364-9897 WARRANTY AND LIMITATION OF REMEDY [734] 971-3335 Buyer agrees to purchase the material subject to Cayman’s Terms and Conditions. -

Ubch7 Regulates 53BP1 Stability and DSB Repair
UbcH7 regulates 53BP1 stability and DSB repair Xiangzi Hana,1, Lei Zhanga,1, Jinsil Chunga,1, Franklin Mayca Pozoa, Amanda Trana, Darcie D. Seachrista, James W. Jacobbergerb, Ruth A. Keria, Hannah Gilmorec, and Youwei Zhanga,2 aDepartment of Pharmacology, bDivision of General Medical Sciences, Case Comprehensive Cancer Center, School of Medicine, and cUniversity Hospitals Case Medical Center, Case Western Reserve University, Cleveland, OH 44106 Edited by Tony Hunter, The Salk Institute for Biological Studies, La Jolla, CA, and approved November 3, 2014 (received for review May 8, 2014) DNA double-strand break (DSB) repair is not only key to genome and generation of one-ended DSBs. Such one-ended DSBs re- stability but is also an important anticancer target. Through an quire HR, but not NHEJ, to repair (8). In contrast, repair of one- shRNA library-based screening, we identified ubiquitin-conjugat- ended DSBs by NHEJ leads to radial chromosomes and cell death ing enzyme H7 (UbcH7, also known as Ube2L3), a ubiquitin E2 (12–14). Therefore, stabilization of 53BP1 by UbcH7 depletion enzyme, as a critical player in DSB repair. UbcH7 regulates both increased the sensitivity of cancers cells to CPT and other DNA the steady-state and replicative stress-induced ubiquitination damaging agents. Our data suggest a novel strategy in enhancing and proteasome-dependent degradation of the tumor suppressor the anticancer effect of radiotherapy or chemotherapy through p53-binding protein 1 (53BP1). Phosphorylation of 53BP1 at the N terminus is involved in the replicative stress-induced 53BP1 degra- stabilizing or increasing 53BP1. dation. Depletion of UbcH7 stabilizes 53BP1, leading to inhibition Results of DSB end resection. -

Tumor Suppressor and DNA Damage Response Panel 2
Tumor suppressor and DNA damage response panel 2 (55 analytes) Gene Symbol Target protein name UniProt ID (& link) Modification* *blanks mean the assay detects the ACT Actin; ACTA2 ACTA1 ACTB ACTG1 ACTC1 ACTG2 Q562L2 non‐modified peptide sequence CASC5 cancer susceptibility candidate 5 Q8NG31 pS767 CASC5 cancer susceptibility candidate 5 Q8NG31 CASP3 caspase 3, apoptosis‐related cysteine peptidase P42574 pS26 CDC25B cell division cycle 25 homolog B (S. pombe) P30305 pS16 CDC25B cell division cycle 25 homolog B (S. pombe) P30305 pS323 CDC25B cell division cycle 25 homolog B (S. pombe) P30305 CDC25C cell division cycle 25 homolog B (S. pombe) P30307 pS216 CDC25C cell division cycle 25 homolog B (S. pombe) P30307 CDCA8 cell division cycle associated 8 Q53HL2 pT16 CDK1 cyclin‐dependent kinase 1 P06493 pT161 CDK1 cyclin‐dependent kinase 1 P06493 CDK7 cyclin‐dependent kinase 7 P50613 pT17 CHEK1 CHK1 checkpoint homolog (S. pombe) O14757 pS286 CHEK2 CHK2 checkpoint homolog (S. pombe) O96017 pS379 CHEK2 CHK2 checkpoint homolog (S. pombe) O96017 pT387 CHEK2 CHK2 checkpoint homolog (S. pombe) O96017 GAPDH Glyceraldehyde‐3‐phosphate dehydrogenase P04406 LAT linker for activation of T cells O43561 pS224 LMNB1 lamin B1 P20700 pT2; pS23 LMNB1 lamin B1 P20700 pT2 LMNB1 lamin B1 P20700 pS23 MCM6 minichromosome maintenance complex component 6 Q14566 pS762 MCM6 minichromosome maintenance complex component 6 Q14566 MDM2 Mdm2, transformed 3T3 cell double minute 2, p53 binding protein (mouse) Q00987 pS166 MDM2 Mdm2, transformed 3T3 cell double minute 2, p53 binding protein (mouse) Q00987 MKI67 antigen identified by monoclonal antibody Ki‐67 P46013 pT181 MKI67 antigen identified by monoclonal antibody Ki‐67 P46013 MKI67 antigen identified by monoclonal antibody Ki‐67 P46013 pT246 MRE11A MRE11 meiotic recombination 11 homolog A (S. -

Targeted Mass Spectrometry Enables Quantification of Novel
cancers Article Targeted Mass Spectrometry Enables Quantification of Novel Pharmacodynamic Biomarkers of ATM Kinase Inhibition Jeffrey R. Whiteaker 1 , Tao Wang 1, Lei Zhao 1, Regine M. Schoenherr 1, Jacob J. Kennedy 1, Ulianna Voytovich 1, Richard G. Ivey 1, Dongqing Huang 1, Chenwei Lin 1, Simona Colantonio 2, Tessa W. Caceres 2, Rhonda R. Roberts 2, Joseph G. Knotts 2, Jan A. Kaczmarczyk 2, Josip Blonder 2, Joshua J. Reading 2, Christopher W. Richardson 2, Stephen M. Hewitt 3, Sandra S. Garcia-Buntley 2, William Bocik 2, Tara Hiltke 4, Henry Rodriguez 4, Elizabeth A. Harrington 5, J. Carl Barrett 5, Benedetta Lombardi 5, Paola Marco-Casanova 5, Andrew J. Pierce 5 and Amanda G. Paulovich 1,* 1 Fred Hutchinson Cancer Research Center, Clinical Research Division, Seattle, WA 98109, USA; [email protected] (J.R.W.); [email protected] (T.W.); [email protected] (L.Z.); [email protected] (R.M.S.); [email protected] (J.J.K.); [email protected] (U.V.); [email protected] (R.G.I.); [email protected] (D.H.); [email protected] (C.L.) 2 Cancer Research Technology Program, Antibody Characterization Lab, Frederick National Laboratory for Cancer Research, Frederick, MD 21701, USA; [email protected] (S.C.); [email protected] (T.W.C.); [email protected] (R.R.R.); [email protected] (J.G.K.); [email protected] (J.A.K.); [email protected] (J.B.); [email protected] (J.J.R.); [email protected] (C.W.R.); [email protected] (S.S.G.-B.); [email protected] (W.B.) 3 Experimental Pathology Laboratory, Laboratory of Pathology, Center for Cancer Research, National Cancer Citation: Whiteaker, J.R.; Wang, T.; Institute, National Institute of Health, Bethesda, MD 20892, USA; [email protected] Zhao, L.; Schoenherr, R.M.; Kennedy, 4 Office of Cancer Clinical Proteomics Research, National Cancer Institute, Bethesda, MD 20892, USA; J.J.; Voytovich, U.; Ivey, R.G.; Huang, [email protected] (T.H.); [email protected] (H.R.) D.; Lin, C.; Colantonio, S.; et al. -

Differential Expression Profile Analysis of DNA Damage Repair Genes in CD133+/CD133‑ Colorectal Cancer Cells
ONCOLOGY LETTERS 14: 2359-2368, 2017 Differential expression profile analysis of DNA damage repair genes in CD133+/CD133‑ colorectal cancer cells YUHONG LU1*, XIN ZHOU2*, QINGLIANG ZENG2, DAISHUN LIU3 and CHANGWU YUE3 1College of Basic Medicine, Zunyi Medical University, Zunyi; 2Deparment of Gastroenterological Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi;3 Zunyi Key Laboratory of Genetic Diagnosis and Targeted Drug Therapy, The First People's Hospital of Zunyi, Zunyi, Guizhou 563003, P.R. China Received July 20, 2015; Accepted January 6, 2017 DOI: 10.3892/ol.2017.6415 Abstract. The present study examined differential expression cells. By contrast, 6 genes were downregulated and none levels of DNA damage repair genes in COLO 205 colorectal were upregulated in the CD133+ cells compared with the cancer cells, with the aim of identifying novel biomarkers for COLO 205 cells. These findings suggest that CD133+ cells the molecular diagnosis and treatment of colorectal cancer. may possess the same DNA repair capacity as COLO 205 COLO 205-derived cell spheres were cultured in serum-free cells. Heterogeneity in the expression profile of DNA damage medium supplemented with cell factors, and CD133+/CD133- repair genes was observed in COLO 205 cells, and COLO cells were subsequently sorted using an indirect CD133 205-derived CD133- cells and CD133+ cells may therefore microbead kit. In vitro differentiation and tumorigenicity assays provide a reference for molecular diagnosis, therapeutic target in BABA/c nude mice were performed to determine whether selection and determination of the treatment and prognosis for the CD133+ cells also possessed stem cell characteristics, in colorectal cancer. -

The Thyroid Hormone Receptor Induces DNA Damage and Premature
Published January 6, 2014 JCB: Article The thyroid hormone receptor induces DNA damage and premature senescence Alberto Zambrano,1 Verónica García-Carpizo,1 María Esther Gallardo,1,3 Raquel Villamuera,1 Maria Ana Gómez-Ferrería,1 Angel Pascual,1 Nicolas Buisine,2 Laurent M. Sachs,2 Rafael Garesse,1,3,4 and Ana Aranda1 1Instituto de Investigaciones Biomédicas “Alberto Sols”, Consejo Superior de Investigaciones Científicas and Universidad Autónoma de Madrid, 28029 Madrid, Spain 2Département Régulation, Développement et Diversité Moléculaire, Unité Mixte de Recherche 7221, Centre National de la Recherche Scientifique, Muséum National d’Histoire Naturelle, 75231 Paris, France 3Centro de Investigación Biomédica en Red, 28029 Madrid, Spain 4Instituto de Investigación Sanitaria Hospital 12 de Octubre, 28041 Madrid, Spain here is increasing evidence that the thyroid hormone factor 1) and THRB to the promoters of genes with a key (TH) receptors (THRs) can play a role in aging, can- role on mitochondrial respiration. Increased respiration T cer and degenerative diseases. In this paper, we leads to production of mitochondrial reactive oxygen spe- Downloaded from demonstrate that binding of TH T3 (triiodothyronine) to cies, which in turn causes oxidative stress and DNA dou- THRB induces senescence and deoxyribonucleic acid ble-strand breaks and triggers a DNA damage response (DNA) damage in cultured cells and in tissues of young that ultimately leads to premature senescence of suscepti- hyperthyroid mice. T3 induces a rapid activation of ATM ble cells. Our findings provide a mechanism for integrat- (ataxia telangiectasia mutated)/PRKAA (adenosine mo- ing metabolic effects of THs with the tumor suppressor jcb.rupress.org nophosphate–activated protein kinase) signal transduc- activity of THRB, the effect of thyroidal status on longevity, tion and recruitment of the NRF1 (nuclear respiratory and the occurrence of tissue damage in hyperthyroidism. -
Defective DNA Repair and Chromatin Organization in Patients with Quiescent Systemic Lupus Erythematosus Vassilis L
Souliotis et al. Arthritis Research & Therapy (2016) 18:182 DOI 10.1186/s13075-016-1081-3 RESEARCH ARTICLE Open Access Defective DNA repair and chromatin organization in patients with quiescent systemic lupus erythematosus Vassilis L. Souliotis1,2*, Konstantinos Vougas3, Vassilis G. Gorgoulis3,4 and Petros P. Sfikakis2 Abstract Background: Excessive autoantibody production characterizing systemic lupus erythematosus (SLE) occurs irrespective of the disease’s clinical status and is linked to increased lymphocyte apoptosis. Herein, we tested the hypothesis that defective DNA damage repair contributes to increased apoptosis in SLE. Methods: We evaluated nucleotide excision repair at the N-ras locus, DNA double-strand breaks repair and apoptosis rates in peripheral blood mononuclear cells from anti-dsDNA autoantibody-positive patients (six with quiescent disease and six with proliferative nephritis) and matched healthy controls following ex vivo treatment with melphalan. Chromatin organization and expression levels of DNA repair- and apoptosis-associated genes were also studied in quiescent SLE. Results: Defective nucleotide excision repair and DNA double-strand breaks repair were found in SLE, with lupus nephritis patients showing higher DNA damage levels than those with quiescent disease. Melphalan-induced apoptosis rates were higher in SLE than control cells and correlated inversely with DNA repair efficiency. Chromatin at the N-ras locus was more condensed in SLE than controls, while treatment with the histone deacetylase inhibitor vorinostat resulted in hyperacetylation of histone H4, chromatin decondensation, amelioration of DNA repair efficiency and decreased apoptosis. Accordingly, genes involved in DNA damage repair and signaling pathways, such as DDB1, ERCC2, XPA, XPC, MRE11A, RAD50, PARP1, MLH1, MLH3, and ATM were significantly underexpressed in SLE versus controls, whereas PPP1R15A, BARD1 and BBC3 genes implicated in apoptosis were significantly overexpressed. -
Genomic Profiling of the Transcription Factor Zfp148 and Its Impact on The
www.nature.com/scientificreports OPEN Genomic profling of the transcription factor Zfp148 and its impact on the p53 pathway Zhiyuan V. Zou1, Nadia Gul1,2,3, Markus Lindberg4, Abdulmalik A. Bokhari4, Ella M. Eklund2,3, Viktor Garellick1, Angana A. H. Patel2,3, Jozefna J. Dzanan2,3, Ben O. Titmuss2,3, Kristell Le Gal2,3, Inger Johansson1, Åsa Tivesten1, Eva Forssell‑Aronsson5,6, Martin O. Bergö7,8, Anna Stafas9, Erik Larsson4, Volkan I. Sayin2,3* & Per Lindahl1,4* Recent data suggest that the transcription factor Zfp148 represses activation of the tumor suppressor p53 in mice and that therapeutic targeting of the human orthologue ZNF148 could activate the p53 pathway without causing detrimental side efects. We have previously shown that Zfp148 defciency promotes p53‑dependent proliferation arrest of mouse embryonic fbroblasts (MEFs), but the underlying mechanism is not clear. Here, we showed that Zfp148 defciency downregulated cell cycle genes in MEFs in a p53‑dependent manner. Proliferation arrest of Zfp148‑defcient cells required increased expression of ARF, a potent activator of the p53 pathway. Chromatin immunoprecipitation showed that Zfp148 bound to the ARF promoter, suggesting that Zfp148 represses ARF transcription. However, Zfp148 preferentially bound to promoters of other transcription factors, indicating that deletion of Zfp148 may have pleiotropic efects that activate ARF and p53 indirectly. In line with this, we found no evidence of genetic interaction between TP53 and ZNF148 in CRISPR and siRNA screen data from hundreds of human cancer cell lines. We conclude that Zfp148 defciency, by increasing ARF transcription, downregulates cell cycle genes and cell proliferation in a p53‑dependent manner. -

A Pathway of Targeted Autophagy Is Induced by DNA Damage in Budding Yeast
A pathway of targeted autophagy is induced by DNA damage in budding yeast Vinay V. Eapena,1, David P. Watermana, Amélie Bernardb, Nathan Schiffmannc, Enrich Sayasd,e, Roarke Kamberf, Brenda Lemosa, Gonen Memisoglua, Jessie Anga, Allison Mazellaa, Silvia G. Chuartzmanc, Robbie J. Loewithd,e, Maya Schuldinerc, Vladimir Denicf, Daniel J. Klionskyb, and James E. Habera,2 aDepartment of Biology, Brandeis University, Waltham, MA 02454; bLife Sciences Institute, University of Michigan, Ann Arbor, MI 48109; cDepartment of Molecular Genetics, Weizmann Institute of Sciences, Rehovot, Israel 7610001; dDepartment of Molecular Biology, University of Geneva, CH-1211 Geneva 4, Switzerland; eInstitute of Genetics and Genomics in Geneva, University of Geneva, CH-1211 Geneva 4, Switzerland; and fMolecular and Cell Biology, Harvard University, Cambridge, MA 02138 Contributed by James E. Haber, December 5, 2016 (sent for review August 31, 2016; reviewed by Eric H. Baehrecke and Stephen J. Elledge) Autophagy plays a central role in the DNA damage response (DDR) by conditions. For example, in response to nutrient starvation, cells controlling the levels of various DNA repair and checkpoint proteins; recycle internal reserves of basic metabolites by the degradation however, how the DDR communicates with the autophagy pathway of proteins, or even whole organelles, by their digestion in the remains unknown. Using budding yeast, we demonstrate that global vacuole/lysosome. This process is initiated by the formation of genotoxic damage or even a single unrepaired double-strand break double-membraned cytosolic sequestering vesicles, termed phag- (DSB) initiates a previously undescribed and selective pathway of ophores, which can engulf either random portions of the cyto- autophagy that we term genotoxin-induced targeted autophagy plasm, organelles, or specific proteins (10).