Stem Cell Treatment After Ischemic Stroke Alters the Expression of Dna Damage Signaling Molecules
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Functions of DNA Damage Factor RNF8 in the Pathogenesis And
Int. J. Biol. Sci. 2019, Vol. 15 909 Ivyspring International Publisher International Journal of Biological Sciences 2019; 15(5): 909-918. doi: 10.7150/ijbs.31972 Review The Functions of DNA Damage Factor RNF8 in the Pathogenesis and Progression of Cancer Tingting Zhou 1, Fei Yi 1, Zhuo Wang 1, Qiqiang Guo 1, Jingwei Liu 1, Ning Bai 1, Xiaoman Li 1, Xiang Dong 1, Ling Ren 2, Liu Cao 1, Xiaoyu Song 1 1. Institute of Translational Medicine, China Medical University; Key Laboratory of Medical Cell Biology, Ministry of Education; Liaoning Province Collaborative Innovation Center of Aging Related Disease Diagnosis and Treatment and Prevention, Shenyang, Liaoning Province, China 2. Department of Anus and Intestine Surgery, First Affiliated Hospital of China Medical University, Shenyang, Liaoning Province, China Corresponding authors: Xiaoyu Song, e-mail: [email protected] and Liu Cao, e-mail: [email protected]. Key Laboratory of Medical Cell Biology, Ministry of Education; Institute of Translational Medicine, China Medical University; Collaborative Innovation Center of Aging Related Disease Diagnosis and Treatment and Prevention, Shenyang, Liaoning Province, 110122, China. Tel: +86 24 31939636, Fax: +86 24 31939636. © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2018.12.03; Accepted: 2019.02.08; Published: 2019.03.09 Abstract The really interesting new gene (RING) finger protein 8 (RNF8) is a central factor in DNA double strand break (DSB) signal transduction. -
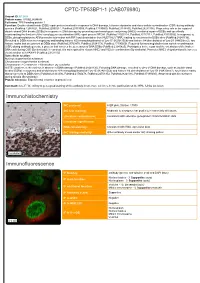
CPTC-TP53BP1-1 (CAB079980) Immunohistochemistry Immunofluorescence
CPTC-TP53BP1-1 (CAB079980) Uniprot ID: Q12888 Protein name: TP53B_HUMAN Full name: TP53-binding protein 1 Function: Double-strand break (DSB) repair protein involved in response to DNA damage, telomere dynamics and class-switch recombination (CSR) during antibody genesis (PubMed:12364621, PubMed:22553214, PubMed:23333306, PubMed:17190600, PubMed:21144835, PubMed:28241136). Plays a key role in the repair of double-strand DNA breaks (DSBs) in response to DNA damage by promoting non-homologous end joining (NHEJ)- mediated repair of DSBs and specifically counteracting the function of the homologous recombination (HR) repair protein BRCA1 (PubMed:22553214, PubMed:23727112, PubMed:23333306). In response to DSBs, phosphorylation by ATM promotes interaction with RIF1 and dissociation from NUDT16L1/TIRR, leading to recruitment to DSBs sites (PubMed:28241136). Recruited to DSBs sites by recognizing and binding histone H2A monoubiquitinated at 'Lys-15' (H2AK15Ub) and histone H4 dimethylated at 'Lys-20' (H4K20me2), two histone marks that are present at DSBs sites (PubMed:23760478, PubMed:28241136, PubMed:17190600). Required for immunoglobulin class-switch recombination (CSR) during antibody genesis, a process that involves the generation of DNA DSBs (PubMed:23345425). Participates in the repair and the orientation of the broken DNA ends during CSR (By similarity). In contrast, it is not required for classic NHEJ and V(D)J recombination (By similarity). Promotes NHEJ of dysfunctional telomeres via interaction with PAXIP1 (PubMed:23727112). Subcellular -

Proteomic Identification of the Transcription Factors Ikaros And
European School of Molecular Medicine (SEMM) University of Milan and University of Naples “Federico II” PhD degree in Systems Medicine (curriculum in Molecular Oncology) Settore disciplinare: BIO/11 Proteomic identification of the transcription factors Ikaros and Aiolos as new Myc interactors on chromatin Chiara Veronica Locarno Matricola: R10755 Center for Genomic Science IIT@SEMM, Milan Supervisor: Bruno Amati, PhD IEO, Milan Added Supervisor: Arianna Sabò, PhD IEO, Milan Academic year 2017-2018 Table of contents List of abbreviations ........................................................................................................... 4 List of figures ....................................................................................................................... 8 List of tables ....................................................................................................................... 11 Abstract .............................................................................................................................. 12 1. INTRODUCTION ......................................................................................................... 13 1.1 Myc ........................................................................................................................................ 13 1.1.1 Myc discovery and structure ........................................................................................... 13 1.1.2. Role of Myc in physiological and pathological conditions ........................................... -

DNA Damage and Its Links to Neurodegeneration
Neuron Review DNA Damage and Its Links to Neurodegeneration Ram Madabhushi,1,2 Ling Pan,1,2 and Li-Huei Tsai1,2,* 1Picower Institute for Learning and Memory 2Department of Brain and Cognitive Sciences Massachusetts Institute of Technology, Cambridge, MA 02139, USA *Correspondence: [email protected] http://dx.doi.org/10.1016/j.neuron.2014.06.034 The integrity of our genetic material is under constant attack from numerous endogenous and exogenous agents. The consequences of a defective DNA damage response are well studied in proliferating cells, espe- cially with regards to the development of cancer, yet its precise roles in the nervous system are relatively poorly understood. Here we attempt to provide a comprehensive overview of the consequences of genomic instability in the nervous system. We highlight the neuropathology of congenital syndromes that result from mutations in DNA repair factors and underscore the importance of the DNA damage response in neural devel- opment. In addition, we describe the findings of recent studies, which reveal that a robust DNA damage response is also intimately connected to aging and the manifestation of age-related neurodegenerative dis- orders such as Alzheimer’s disease and amyotrophic lateral sclerosis. Introduction The Cellular DNA Damage Response Upon analyzing the data collected in the 2000 census, health On any given day, a listing of endogenous DNA damage experi- officials arrived at the remarkable prediction that by the year enced by a typical mammalian cell would read something as fol- 2050, approximately 800,000 Americans would live to see their lows: 200 cytosine deaminations, 3,000 guanine methylations, hundredth birthday (Park, 2010). -

NBN Gene Analysis and It's Impact on Breast Cancer
Journal of Medical Systems (2019) 43: 270 https://doi.org/10.1007/s10916-019-1328-z IMAGE & SIGNAL PROCESSING NBN Gene Analysis and it’s Impact on Breast Cancer P. Nithya1 & A. ChandraSekar1 Received: 8 March 2019 /Accepted: 7 May 2019 /Published online: 5 July 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Single Nucleotide Polymorphism (SNP) researches have become essential in finding out the congenital relationship of structural deviations with quantitative traits, heritable diseases and physical responsiveness to different medicines. NBN is a protein coding gene (Breast Cancer); Nibrin is used to fix and rebuild the body from damages caused because of strand breaks (both singular and double) associated with protein nibrin. NBN gene was retrieved from dbSNP/NCBI database and investigated using computational SNP analysis tools. The encrypted region in SNPs (exonal SNPs) were analyzed using software tools, SIFT, Provean, Polyphen, INPS, SNAP and Phd-SNP. The 3’ends of SNPs in un-translated region were also investigated to determine the impact of binding. The association of NBN gene polymorphism leads to several diseases was studied. Four SNPs were predicted to be highly damaged in coding regions which are responsible for the diseases such as, Aplastic Anemia, Nijmegan breakage syndrome, Microsephaly normal intelligence, immune deficiency and hereditary cancer predisposing syndrome (clivar). The present study will be helpful in finding the suitable drugs in future for various diseases especially for breast cancer. Keywords NBN . Single nucleotide polymorphism . Double strand breaks . nsSNP . Associated diseases Introduction NBN has a more complex structure due to its interaction with large proteins formed from the ATM gene which is NBN (Nibrin) is a protein coding gene, it is also known as highly essential in identifying damaged strands of DNA NBS1, Cell cycle regulatory Protein P95, is situated on and facilitating their repair [1]. -

RIDDLE Immunodeficiency Syndrome Is Linked to Defects in 53BP1-Mediated DNA Damage Signaling
RIDDLE immunodeficiency syndrome is linked to defects in 53BP1-mediated DNA damage signaling Grant S. Stewart*†, Tatjana Stankovic*, Philip J. Byrd*, Thomas Wechsler‡, Edward S. Miller*, Aarn Huissoon§, Mark T. Drayson¶, Stephen C. West‡, Stephen J. Elledge†ʈ, and A. Malcolm R. Taylor* *Cancer Research UK, Institute for Cancer Studies, Birmingham University, Vincent Drive, Edgbaston, Birmingham B15 2TT, United Kingdom; ‡Cancer Research UK, Clare Hall Laboratories, London Research Institute, South Mimms, Hertfordshire EN6 3LD, United Kingdom; §Department of Immunology, Birmingham Heartlands Hospital, Birmingham, B9 5SS, United Kingdom; ¶Division of Immunity and Infection, Birmingham University Medical School, Vincent Drive, Edgbaston, Birmingham B15 2TT, United Kingdom; and ʈHoward Hughes Medical Institute, Department of Genetics, Harvard Partners Center for Genetics and Genomics, Harvard Medical School, 77 Avenue Louis Pasteur, Boston, MA 02115 Contributed by Stephen J. Elledge, September 6, 2007 (sent for review July 6, 2007) Cellular DNA double-strand break-repair pathways have evolved with an alternative constant region (e.g., ␣, ␥, ) to generate to protect the integrity of the genome from a continual barrage of different Ig isotypes e.g., IgA, IgG, and IgE (2). potentially detrimental insults. Inherited mutations in genes that During the process of CSR, it has been hypothesized that two control this process result in an inability to properly repair DNA closely positioned single-stranded DNA nicks result in the damage, ultimately -

WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT (51) International Patent Classification: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, C12Q 1/68 (2018.01) A61P 31/18 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, C12Q 1/70 (2006.01) HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/US2018/056167 OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (22) International Filing Date: SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 16 October 2018 (16. 10.2018) TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, (30) Priority Data: UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, 62/573,025 16 October 2017 (16. 10.2017) US TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, ΓΕ , IS, IT, LT, LU, LV, (71) Applicant: MASSACHUSETTS INSTITUTE OF MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, TECHNOLOGY [US/US]; 77 Massachusetts Avenue, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, Cambridge, Massachusetts 02139 (US). -

RNF168 Ubiquitylates 53BP1 and Controls Its Response to DNA Double-Strand Breaks
RNF168 ubiquitylates 53BP1 and controls its response to DNA double-strand breaks Miyuki Bohgakia,b,1, Toshiyuki Bohgakia,b,1, Samah El Ghamrasnia,b, Tharan Srikumara,b, Georges Mairec, Stephanie Panierd, Amélie Fradet-Turcotted, Grant S. Stewarte, Brian Raughta,b, Anne Hakema,b, and Razqallah Hakema,b,2 aOntario Cancer Institute, University Health Network and bDepartment of Medical Biophysics, University of Toronto, Toronto, M5G 2M9 ON, Canada; cThe Hospital for Sick Children, Toronto, M5G 2L3 ON, Canada; dDepartment of Molecular Genetics, University of Toronto, Toronto, ON, Canada M5S 1A8; and eCancer Research UK, Institute for Cancer Studies, Birmingham University, Birmingham B15 2TT, United Kingdom Edited* by Stephen J. Elledge, Harvard Medical School, Boston, MA, and approved November 14, 2013 (received for review October 30, 2013) Defective signaling or repair of DNA double-strand breaks has X–MDC1–RNF8 axis, RNF168 also functions in DSB signaling been associated with developmental defects and human diseases. independently of this pathway. Therefore, we postulated that The E3 ligase RING finger 168 (RNF168), mutated in the human RNF168 also might regulate DSB signaling through direct radiosensitivity, immunodeficiency, dysmorphic features, and modulation of 53BP1 functions. learning difficulties syndrome, was shown to ubiquitylate H2A- In the present study, we demonstrate that RNF168 associates γ – – type histones, and this ubiquitylation was proposed to facilitate with 53BP1 independently of the -H2A.X MDC1 RNF8 sig- the recruitment of p53-binding protein 1 (53BP1) to the sites of naling axis. RNF168 ubiquitylates 53BP1 before its localization DNA double-strand breaks. In contrast to more upstream proteins to DSB sites, and this ubiquitylation is important for the initial signaling DNA double-strand breaks (e.g., RNF8), deficiency of recruitment of 53BP1 to DSB sites and its function in non- homologous end joining (NHEJ) and activation of checkpoints. -

Mutations in the Nijmegen Breakage Syndrome Gene (NBS1) in Childhood Acute Lymphoblastic Leukemia (ALL)1
[CANCER RESEARCH 61, 3570–3572, May 1, 2001] Advances in Brief Mutations in the Nijmegen Breakage Syndrome Gene (NBS1) in Childhood Acute Lymphoblastic Leukemia (ALL)1 Raymonda Varon, Andre´Reis,2 Gu¨nter Henze, Hagen Graf v. Einsiedel, Karl Sperling, and Karlheinz Seeger Institute of Human Genetics [R. V., A. R., K. Sp.] and Department of Pediatric Oncology/Hematology [G. H., H. G. v. E., K. Se.], Charite´, Humboldt-University, 13353 Berlin, Germany, and Molecular Genetics and Gene Mapping Centre, Max-Delbrueck-Centre, 13092 Berlin, Germany [A. R.] Abstract protein—a FHA and a BRCT, both spanning the first 200 amino acids of nibrin (9)—that are also present in a number of other proteins The Nijmegen Breakage Syndrome (NBS) is a rare autosomal recessive involved in the cell cycle control (10, 11). On the basis of epidemi- disorder associated with immune deficiency, chromosome fragility, and ological data, it has been suggested that NBS heterozygotes also have increased susceptibility to lymphoid malignancies. The aim of the present an elevated cancer risk (12) similar to AT or other syndromes asso- study was to elucidate the potential role of the gene mutated in NBS (NBS1) in the pathogenesis and disease progression of childhood acute ciated with immune deficiencies (4). The findings that the ATM gene lymphoblastic leukemia (ALL). Samples from 47 children with first re- is involved in the pathogenesis of B-CLL (13, 14) and T-cell prolym- lapse of ALL were analyzed for mutations in all 16 exons of the NBS1 phocytic leukemia (15) as well as in breast cancer (16) implicate its gene, and in 7 of them (14.9%), four novel amino acid substitutions were role as a tumor suppressor gene. -

MDC1 and RNF8 Function in a Pathway That Directs BRCA1
Research Article 6049 MDC1 and RNF8 function in a pathway that directs BRCA1-dependent localization of PALB2 required for homologous recombination Fan Zhang1, Gregory Bick1, Jung-Young Park1 and Paul R. Andreassen1,2,* 1Division of Experimental Hematology and Cancer Biology, Cincinnati Children’s Research Foundation, Cincinnati, OH 45229, USA 2Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH 45229, USA *Author for correspondence ([email protected]) Accepted 6 September 2012 Journal of Cell Science 125, 6049–6057 ß 2012. Published by The Company of Biologists Ltd doi: 10.1242/jcs.111872 Summary The PALB2 protein is associated with breast cancer susceptibility and Fanconi anemia. Notably, PALB2 is also required for DNA repair by homologous recombination (HR). However, the mechanisms that regulate PALB2, and the functional significance of its interaction with the BRCA1 breast cancer susceptibility protein, are poorly understood. Here, to better understand these processes, we fused PALB2, or the PALB2(L21P) mutant which cannot bind to BRCA1, with the BRCT repeats that are present in, and which localize, BRCA1. Our results yield important insights into the regulation of PALB2 function. Both fusion proteins can bypass BRCA1 to localize to sites of DNA damage. Further, the localized fusion proteins are functional, as determined by their ability to support the assembly of RAD51 foci, even in the absence of the capacity of PALB2 to bind BRCA1. Strikingly, the localized fusion proteins mediate DNA double-strand break (DSB)-initiated HR and resistance to mitomycin C in PALB2-deficient cells. Additionally, we show that the BRCA1–PALB2 heterodimer, rather than the PALB2–PALB2 homodimer, mediates these responses. -

PRODUCT INFORMATION TP53BP1 BRCT Domains (Human Recombinant) Item No
PRODUCT INFORMATION TP53BP1 BRCT domains (human recombinant) Item No. 14171 • Batch No. XXXX Overview and Properties Synonyms: Tumor Protein p53 binding Protein 1, Tumor Suppressor p53-binding Protein 1 Source: Recombinant human N-terminal GST-tagged protein expressed in E. coli amino acids 1,717-1,972 (N- and C-terminal truncation) Uniprot No.: Q12888 Batch specific information can be found on the Batch Specific Insert or by contacting Technical Support Molecular Weight: 55.1 kDa Storage: -80°C (as supplied) Stability: ≥6 months Purity: batch specific Supplied in: 50 mM Tris-HCl, pH 8.0, containing 150 mM sodium chloride and 20% glycerol Protein Concentration: batch specific mg/ml Image(s) 1 2 3 4 250 kDa · · · · · · · 150 kDa · · · · · · · 100 kDa · · · · · · · 75 kDa · · · · · · · 50 kDa · · · · · · · 37 kDa · · · · · · · 25 kDa · · · · · · · 20 kDa · · · · · · · Lane 1: MW Markers Lane 2: TP53BP1 BRCT domains (1 µg) Lane 3: TP53BP1 BRCT domains (2 µg) Lane 4: TP53BP1 BRCT domains (5 µg) Representative gel image shown; actual purity may vary between each batch. WARNING CAYMAN CHEMICAL THIS PRODUCT IS FOR RESEARCH ONLY - NOT FOR HUMAN OR VETERINARY DIAGNOSTIC OR THERAPEUTIC USE. 1180 EAST ELLSWORTH RD SAFETY DATA ANN ARBOR, MI 48108 · USA This material should be considered hazardous until further information becomes available. Do not ingest, inhale, get in eyes, on skin, or on clothing. Wash thoroughly after handling. Before use, the user must review the complete Safety Data Sheet, which has been sent via email to your institution. PHONE: [800] 364-9897 WARRANTY AND LIMITATION OF REMEDY [734] 971-3335 Buyer agrees to purchase the material subject to Cayman’s Terms and Conditions. -

Identification of the Interactors of Human Nibrin (NBN) and of Its 26 Kda and 70 Kda Fragments Arising from the NBN 657Del5 Founder Mutation
RESEARCH ARTICLE Identification of the Interactors of Human Nibrin (NBN) and of Its 26 kDa and 70 kDa Fragments Arising from the NBN 657del5 Founder Mutation Domenica Cilli1., Cristiana Mirasole2., Rosa Pennisi1, Valeria Pallotta2, Angelo D’Alessandro2, Antonio Antoccia1,3, Lello Zolla2, Paolo Ascenzi3,4, Alessandra di Masi1,3* 1. Department of Science, Roma Tre University, Rome, Italy, 2. Department of Ecological and Biological Sciences, University of Tuscia, Viterbo, Italy, 3. Istituto Nazionale Biostrutture e Biosistemi – Consorzio Interuniversitario, Rome, Italy, 4. Interdepartmental Laboratory for Electron Microscopy, Roma Tre University, Rome, Italy *[email protected] . These authors contributed equally to this work. OPEN ACCESS Citation: Cilli D, Mirasole C, Pennisi R, Pallotta V, Abstract D’Alessandro A, et al. (2014) Identification of the Interactors of Human Nibrin (NBN) and of Its 26 Nibrin (also named NBN or NBS1) is a component of the MRE11/RAD50/NBN kDa and 70 kDa Fragments Arising from the NBN complex, which is involved in early steps of DNA double strand breaks sensing and 657del5 Founder Mutation. PLoS ONE 9(12): e114651. doi:10.1371/journal.pone.0114651 repair. Mutations within the NBN gene are responsible for the Nijmegen breakage Editor: Sue Cotterill, St. Georges University of syndrome (NBS). The 90% of NBS patients are homozygous for the 657del5 London, United Kingdom mutation, which determines the synthesis of two truncated proteins of 26 kDa (p26) Received: October 28, 2013 and 70 kDa (p70). Here, HEK293 cells have been exploited to transiently express Accepted: November 12, 2014 either the full-length NBN protein or the p26 or p70 fragments, followed by affinity Published: December 8, 2014 chromatography enrichment of the eluates.