Drug and Alcohol Dependence 181 (2017) 162–169
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Controlled Drinking: More Than Just a Controversy 05/07/2007 08:37 AM
Controlled Drinking: More Than Just a Controversy 05/07/2007 08:37 AM www.medscape.com To Print: Click your browser's PRINT button. NOTE: To view the article with Web enhancements, go to: http://www.medscape.com/viewarticle/473554 Controlled Drinking: More Than Just a Controversy Michael E. Saladin; Elizabeth J. Santa Ana Curr Opin Psychiatry 17(3):175-187, 2004. © 2004 Lippincott Williams & Wilkins Posted 04/28/2004 Abstract and Introduction Abstract Purpose of Review: We intend to provide clinicians and clinical scientists with an overview of developments in the controlled-drinking literature, primarily since 2000. A brief description of the controversy surrounding controlled drinking provides a context for a discussion of various approaches to controlled drinking intervention as well as relevant clinical research. Recent Findings: Consistent with previous research, behavioral self-control training continues to be the most empirically validated controlled-drinking intervention. Recent research has focused on increasing both the accessibility/availability and efficacy of behavioral self-control training. Moderation-oriented cue exposure is a recent development in behaviorally oriented controlled drinking that yields treatment outcomes comparable to behavioral self-control training. The relative efficacy of moderation-oriented cue exposure versus behavioral self- control training may vary depending on the format of treatment delivery (group versus individual) and level of drinking severity. In general, the efficacy of both techniques does not appear to vary as a function of drinking severity but may vary as a function of drinking-related self-efficacy. Guided-self change is a relatively new and brief cognitive-behavioral intervention that has demonstrated efficacy with problem drinkers. -

Styles of Secular Recovery
White, W. & Nicolaus, M. (2005). Styles of secular recovery. Counselor, 6(4), 58-61. Styles of Secular Recovery William L. White and Martin Nicolaus The last essay in this column noted the growing diversity in religious, spiritual and secular frameworks of recovery and sketched the history of religious approaches to addiction recovery. This essay reviews the history and growing varieties of secular recovery and the implications of such diversity for the addictions professional. A History of Secular Recovery The history of non-religious, non-spiritual approaches to the resolution of alcohol and other drug problems begins with the Washingtonian Revival of the 1840s. The Washingtonians removed preachers and physicians from the temperance lectern in favor of men and women who, in the vernacular of the day, were “reformed” or were “reforming.” The Washingtonians replaced religious admonitions not to drink with 1) public confession of one’s addiction, 2) a signed pledge of abstinence, 3) visits to younger members, 4) economic assistance to new members, 5) experience sharing meetings, 6) outreach to the suffering drunkard, and 7) sober entertainment and fellowship. While many Washingtonians entered the life of their local churches, Washingtonian leaders were charged by their religious critics with committing the sin of humanism--placing their own will above the power of God. Recovery support societies that followed the Washingtonians took on a more religious orientation, but secular recovery groups continued in some of the mid- century moderation societies, ribbon reform clubs and support societies that grew out of early treatment institutions, e.g. the Ollapod Club and the Keeley Leagues. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

Staying Connected Is Important: Virtual Recovery Resources
STAYING CONNECTED IS IMPORTANT: VIRTUAL RECOVERY RESOURCES • Refuge Recovery: Provides online and virtual INTRODUCTION support In an infectious disease outbreak, when social https://www.refugerecovery.org/home distancing and self-quarantine are needed to • Self-Management and Recovery Training limit and control the spread of the disease, (SMART) Recovery: Offers global community continued social connectedness to maintain of mutual-support groups, forums including a recovery is critically important. Virtual chat room and message board resources can and should be used during this https://www.smartrecovery.org/community/ time. Even after a pandemic, virtual support may still exist and still be necessary. • SoberCity: Offers an online support and recovery community This tip sheet describes resources that can be https://www.soberocity.com/ used to virtually support recovery from mental/ substance use disorders as well as other • Sobergrid: Offers an online platform to help resources. anyone get sober and stay sober https://www.sobergrid.com/ • Soberistas: Provides a women-only VIRTUAL RECOVERY PROGRAMS international online recovery community https://soberistas.com/ • Alcoholics Anonymous: Offers online support • Sober Recovery: Provides an online forum for https://aa-intergroup.org/ those in recovery and their friends and family https://www.soberrecovery.com/forums/ • Cocaine Anonymous: Offers online support and services • We Connect Recovery: Provides daily online https://www.ca-online.org/ recovery groups for those with substance use and -

Sacrifice, Stigma, and Free-Riding in Alcoholics Anonymous (AA): a New Perspective on Behavior Change in Self-Help Organizations for Addiction
Sacrifice and stigma in AA Sacrifice, stigma, and free-riding in Alcoholics Anonymous (AA): A new perspective on behavior change in self-help organizations for addiction Anna Lembke, MD Stanford University February 2013 Abstract Iannaccone and others have claimed that behavior change in religious organizations is mediated in part by sacrifice and stigma, which enhances participation, augments club goods that make participation worthwhile, and reduces free-riding. As applied to Alcoholics Anonymous (AA), a non-religious self-help organization for addiction, Iannaccone’s ideas shed light on the ways in which sacrifice and stigma influence behavior in AA. AA members’ willingness to embrace a stigmatized identity, give up alcohol, and participate in the AA fellowship, creates the club goods that are integral to ‘recovery’ from addiction. Iannaccone’s model furthermore illuminates the problem of free-riding in AA, providing one explanation for the incredible rate of growth of AA over the years, particularly as compared with less ‘strict’ self-help organizations for alcohol use problems, such as Moderation Management. Keywords Sacrifice, stigma, free-riding, 12-steps, Alcoholics Anonymous, Moderation Management, mechanism of change 1 Sacrifice and stigma in AA Introduction Addictive disorders represent one of the greatest public health threats to the developed world, contributing to the suffering of millions, including over 500,000 substance-use-related U.S. deaths annually (Horgan et al., 2001). Self-help organizations are the most commonly utilized treatment for people with addiction in the United States today (Miller and McCrady, 1993). There exist many different types of self-help organizations for addiction, e.g. -

Addiction : an Information Guide / Marilyn Herie
A addiction can affect your health, relationships, finances, d d i c career—every aspect of your life. You may not see your t i o substance use as a problem, and even if you do, it can still n Addiction be hard to change. A n Addiction: An Information Guide is for people who are i n f having problems with alcohol or other drugs, their families o r m and friends, and anyone else who wants to better under - a An t i o stand addiction. The guide describes what addiction is, n g what is thought to cause it, and how it can be managed u i d and treated. The guide also includes ways family members e can support people with addiction while taking care of information themselves, and tips on explaining addiction to children. guide This publication may be available in other formats. For information about alternate formats or other CAMH publications, or to place an order, please contact Sales and Distribution: Toll-free: 1 800 661-1111 Toronto: 416 595-6059 E-mail: [email protected] Online store: http://store.camh.net To make a donation, please contact the CAMH Foundation: Tel.: 416 979-6909 E-mail: [email protected] Website: www.camh.net Disponible en français. Marilyn Herie, PhD, RSW 3 4 Tim Godden, MSW, RSW 0 M P Joanne Shenfeld, MSW, RSW / 0 1 0 Colleen Kelly, MSW, RSW 2 - 5 0 / d 3 A Pan American Health Organization / 7 9 World Health Organization Collaborating Centre 3 i Addiction An information guide A GUIDE FOR PEOPLE WITH ADDICTION AND THEIR FAMILIES Marilyn Herie, PhD, RSW Tim Godden, MSW, RSW Joanne Shenfeld, MSW, RSW Colleen Kelly, MSW, RSW A Pan American Health Organization / World Health Organization Collaborating Centre ii Addiction: An information guide Library and Archives Canada Cataloguing in Publication Addiction : an information guide / Marilyn Herie.. -

Experimental and Clinical Psychopharmacology Context and Craving Among Individuals with Alcohol Use Disorder Attempting to Moderate Their Drinking Alexis N
Experimental and Clinical Psychopharmacology Context and Craving Among Individuals With Alcohol Use Disorder Attempting to Moderate Their Drinking Alexis N. Kuerbis, Sijing Shao, Hayley Treloar Padovano, Anna Jadanova, Danusha Selva Kumar, Rachel Vitale, George Nitzburg, Nehal P. Vadhan, and Jon Morgenstern Online First Publication, January 23, 2020. http://dx.doi.org/10.1037/pha0000349 CITATION Kuerbis, A. N., Shao, S., Treloar Padovano, H., Jadanova, A., Selva Kumar, D., Vitale, R., Nitzburg, G., Vadhan, N. P., & Morgenstern, J. (2020, January 23). Context and Craving Among Individuals With Alcohol Use Disorder Attempting to Moderate Their Drinking. Experimental and Clinical Psychopharmacology. Advance online publication. http://dx.doi.org/10.1037/pha0000349 Experimental and Clinical Psychopharmacology © 2020 American Psychological Association 2020, Vol. 1, No. 999, 000 ISSN: 1064-1297 http://dx.doi.org/10.1037/pha0000349 Context and Craving Among Individuals With Alcohol Use Disorder Attempting to Moderate Their Drinking Alexis N. Kuerbis Sijing Shao City University of New York Center for Addiction Services and Psychotherapy Research, Northwell Health, Great Neck, New York Hayley Treloar Padovano Anna Jadanova, Danusha Selva Kumar, Center for Alcohol and Addiction Studies, Providence, Rachel Vitale, George Nitzburg, Nehal P. Vadhan, Rhode Island and Jon Morgenstern Center for Addiction Services and Psychotherapy Research, Northwell Health, Great Neck, New York Many individuals with alcohol use disorder (AUD) prefer a goal of moderation, because they do not see their drinking as causing severe enough consequences to merit abstinence. Given that individuals attempting to moderate will continue to put themselves in contexts where drinking occurs, understanding how distinct external alcohol cues prompt craving is important for implementing the optimal treatments for individuals with AUD. -
Maintaining Sobriety How Support Groups Can Help
MAINTAINING SOBRIETY HOW SUPPORT GROUPS CAN HELP Barbara H. Bradford, LICSW March 19, 2014 Overview • What do we know • High cost of substance-related addictive disorders • Role of support groups • Resources What do we know? •More than one-half of American adults have a close family member who has or has had Alcohol Use Disorder (AUD) •The federal government estimates that 8.9 percent of full-time workers have drinking problems •Alcohol costs American business an estimated $134 billion in productivity losses, mostly due to missed work •According to SAMHSA, in 2011, 133.4 million people used alcohol & 22.5 million used illicit drugs. What do we know • 22% of men and 14% of women have some type of substance-related addictive disorder (National Survey on Drug Use and Health 2011) • According to the National Center for Health Statistics – there were 38,329 overdose deaths in the US in 2010. 57.7% of those involved pharmaceuticals, 74.3% were unintentional Support group history • Native Americans • Washingtonians • Oxford Groups • Alcoholics Anonymous • Post AA alternatives Alcoholics Anonymous • 1935 “Dr. Bob & Bill W” • Primary features – Admit to having problem with alcohol – Acknowledge role of “Higher Power” – Sharing experience in meeting settings – Peer mentoring (sponsorship) 2.1 million members in 150 countries Strong on line presence with e-groups available Narcotics Anonymous • 1953 NA began in California • AA endorsed NA to make use of AA 12 Steps/traditions • 1970’s time of rapid growth from 20 meetings nationally to 1100 meetings -
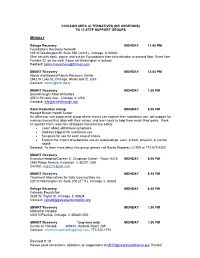
Chicago Area Additions/Alternatives to 12 Step
CHICAGO AREA ALTERNATIVES (OR ADDITIONS) TO 12 STEP SUPPORT GROUPS MONDAY Refuge Recovery MONDAY 12:00 PM Foundations Recovery Network 225 W Washington St. Suite 550 (2nd fl.), Chicago, IL 60603 (See security desk, sign in and ask for Foundations then take elevator to second floor. Enter from Franklin St. on the west if door on Washington is locked). Contact: [email protected] SMART Recovery MONDAY 12:00 PM Above and Beyond Family Recovery Center 2942 W Lake St.,Chicago, Illinois 60612, USA Contact: [email protected] SMART Recovery MONDAY 1:00 PM Breakthrough Urban Ministries 402 N St Louis Ave., Chicago, IL USA Contact: [email protected] Harm Reduction Group MONDAY 6:00 PM Howard Brown Health Center An affirming, non-judgmental group where clients can explore their substance use, get support for making choices that align with their values, and learn tools to help them reach their goals. Work on specific harm reduction strategies that prioritize safety Learn about withdrawal symptoms Address triggers for substance use Set goals for use for each drug of choice Explore the impact of substance use on relationships, work, school, physical, & mental health Contact: To learn more about this group, please call Sonila Sejdaras, LCSW at 773.572.8353 SMART Recovery Evanston Hospital/Doreen E. Chapman Center - Room 5415 MONDAY 6:00 PM 2650 Ridge Avenue, Evanston, IL 60201 USA Contact: [email protected] SMART Recovery MONDAY 6:15 PM Treatment Alternatives for Safe Communities Inc. 225 W Washington St. Suite 200 (2nd fl.), Chicago, IL 60603 Refuge Recovery MONDAY 6:30 PM Gateway Foundation 3828 W. -

Spirituality and Alcohol Consumption in a General Population
Rowan University Rowan Digital Works Theses and Dissertations 9-17-2013 Spirituality and alcohol consumption in a general population Nicole Keenan Follow this and additional works at: https://rdw.rowan.edu/etd Part of the Psychiatric and Mental Health Commons Recommended Citation Keenan, Nicole, "Spirituality and alcohol consumption in a general population" (2013). Theses and Dissertations. 209. https://rdw.rowan.edu/etd/209 This Thesis is brought to you for free and open access by Rowan Digital Works. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Rowan Digital Works. For more information, please contact [email protected]. SPIRITUALITY AND ALCOHOL CONSUMPTION IN A GENERAL POPULATION by Nicole Marie Keenan A Thesis Submitted to the Department of Psychology College of Science and Math In partial fulfillment of the requirement For the degree of Master of Arts in Clinical Mental Health Counseling at Rowan University May 2013 Thesis Chair: Matthew Miller, Psy.D. Dedication I would like to dedicate this manuscript to my fellow Rowan University Clinical Mental Health Counseling 2013 graduates Acknowledgements I would like to express my appreciation to Dr. Matthew Miller for his guidance and support throughout this entire thesis process. Secondly, I'd like to thank my roommate Jenny Delorme for her emotional support and empathic understanding. iv Abstract Nicole Marie Keenan SPIRITUALITY, GENDER AND ALCOHOL CONSUMPTION IN A GENERAL POPULATION 2012/2013 Matthew Miller, Psy.D. Master of Arts in Clinical Mental Health Counseling This study examined the relationship between spirituality and alcohol consumption in a general population because spirituality is important when it comes to the treatment and continued recovery from addiction. -

Selected Papers of William L. White
Selected Papers of William L. White www.williamwhitepapers.com Collected papers, interviews, video presentations, photos, and archival documents on the history of addiction treatment and recovery in America. Citation: Kelly, J. & White, W. (2012) Broadening the base of addiction recovery mutual aid. Journal of Groups in Addiction & Recovery, 7(2-4), 82-101. Posted at www.williamwhitepapers.com Broadening the Base of Addiction Recovery Mutual Aid John F. Kelly, PhD and William L. White, MA Abstract mutual help options. This article presents a concise overview of the Peer-led mutual help organizations origins, size, and state of the science addressing substance use disorder on several of the largest of these (SUD) and related problems have had alternative additional mutual help a long history in the United States. organizations in an attempt to raise The modern epoch of addiction further awareness and help broaden mutual help began in the post- the base of addiction mutual help. prohibition era of the 1930s with the birth of Alcoholics Anonymous (AA). Keywords: Mutual help; mutual aid; self Growing from two members to two help; Alcoholics Anonymous; narcotics million members, AA’s reach and anonymous; SMART recovery; Secular influence has drawn much public organization for Sobriety; Women for health attention as well as Sobriety; Moderation Management. increasingly rigorous scientific investigation into its benefits and 1. Introduction mechanisms. In turn, AA’s growth and success has spurred the At first glance, the notion of development of myriad additional individuals with serious, objectively mutual help organizations. These verifiable, cognitive and social impairments alternatives may confer similar being able to facilitate life-saving changes in benefits to those found in studies of similarly impaired individuals may seem a AA, but have received only peripheral little incongruous; from a derisory attention. -

Introduction to SMART Recovery®
Introduction to SMART Recovery® http://www.smartrecovery.org/intro/ Search HOME GET STARTED LOCAL MEETINGS ONLINE COMMUNITY RESOURCES STORE Introduction to SMART Recovery "Discover the Power of Choice!"™ SMART Recovery's 4-Point Program® helps people recover from all types of addictive behaviors, including: alcoholism, drug abuse, substance abuse, drug addiction, alcohol abuse, gambling addiction, Follow Us cocaine addiction, and addiction to other substances and activities. SMART Recovery (Self-Management And Recovery Training) is not a 12-step group, like Alcoholics Anonymous (AA) or Narcotics Quick Links Anonymous (NA). Introduction to SMART Recovery Family & Friends SMART Recovery sponsors face-to-face meetings around the world, Teen & Youth Program and daily online meetings. In addition, our online message board and 24/7 chat room are excellent forums to learn about SMART Recovery and obtain addiction recovery support. Facilitator Training For Addiction Professionals Please note that registration at our messageboard is required for our online meetings. Courts and Legal For Correctional Facilities Need Urgent Help? Welcome to SMART Recovery Special Event SMART Recovery Blog An Interview with Dr. Michael R. Edelstein: Cognitive Tools for Fighting Addiction and Beyond SMART Recovery® is delighted to announce a new SMA... Watch our video and learn more about SMART Recovery and our 4-Point Program. Think SMART! SMART for Life: An Entertaining and Informative Vi... What’s the first step of habit change? Going off autopilot! Our Purpose – Carrie Wilkens, Clinical Director of the Center ... To support individuals who have chosen to abstain, or are considering abstinence from any type of addictive The Greatest Salesperson I will behaviors (substances or activities), by teaching how to change self-defeating thinking, emotions, and actions; and ever meet! 1 of 4 6/20/15 11:36 AM Introduction to SMART Recovery® http://www.smartrecovery.org/intro/ to work towards long-term satisfactions and quality of life.