1091-Ball-Basics-Web.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epididymo-Orchitis
Epididymo-orchitis In men over the age of 35 years the most Epididymo-orchitis Bladder common cause is a urine infection – with local Seminal spread of infection from the bladder. This may Epidiymo-orchitis – the basics vesicle Epididymo-orchitisIt is a condition- the basics affecting men characterised by also occur after surgical procedures such as pain and swelling inside the scrotum (ball bag) Prostate Rectum cystoscopy or catheterisation. Epididymo-orchitisand is duea tocondition an infection eitherthat in causesthe: pain and Urethra Occasionally it may also be due to a ‘gut’ swelling inside the scrotum (ball bag). epididymis – tube carrying the sperm from bacterial infection from insertive anal Te s t i s the testicle to the vas deferens and then the intercourse. It is due to an infectionurethra either or water in pipe the: (epididymitis) Rarely epididymo-orchitis may be caused by Penis • epididymistesticle – tube (orchitis) carrying the sperm from the other infections such as mumps or tuberculosis. testicle to theepididymis vas deferensand testicle (epididymo-orchitis)and then the Vas urethra or water pipe (epididymitis) deferens What would I notice if I had epididymo-orchitis? • In men under the age of 35 years it is usually A rapid onset of pain and swelling in one or testicle (orchitis) Epididymis caused by a sexually transmitted infection (STI) sometimes both of your testicles. • epididymisin theand water testicle pipe e.g. (epididymo chlamydia or gonorrhoea.-orchitis) Scrotal Te s t i s Some men may also notice a discharge from Skin Prompt medical assessment is needed to the tip of the water pipe and/or pain on passing In people undermake 35 sure theyou don’t infection have a twisted is testicleoften sexually urine. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Torsión Del Cordón Espermático
Torsión del cordón espermático A. SííMí MoYÁNO, J. J. GÓMEZ Ruíz, A. GÓMEZ VEGAS, J. Bi.k’ouriz IzouínRDo, J. CORRAL Rosíu.o y L. RESEL EsrÉvEz Cátedra y Servicio de Urología. Hospital Universitario San Carlos. Universidad Complutense de Madrid La primera descripción de una torsión o vólvulo del cordón espermático parece que fue realizada por Delasiauve’, en el año 1840, bajo el siguiente epígrafe: «Necrosis de un testiculo ectópico ocasionado por una hernia inguinal estrangulada en el adulto». La torsión del cordón espermático con la consecuente isquemia e infarto hemorrágico del parénquima testicular constituye uno de los accidentesvasculares dídimo epididimarios más importantes y que, a pesar del aumento progresivo de su incidencia anual, obliga a la orquiectomia tanto o más que ninguna otra patología testicular, incluido lostumores de dicho órgano’3. Según se desprende de la literatura médica revisada, al igual que de nuestra propia experiencia, será difícil que disminuya ostensiblemente el número de exéresis testiculares por esta causa patológica en un futuro próximo, aun contando en el mayorde loscasos con la colaboración del paciente, nuevas técnicas para un diagnóstico precoz y una actuación de urgencia quirúrgica4- <‘L É2AÑ¡9 El error o la tardanza en diagnosticar este proceso agudo puede suponer la pérdida de la glándula testicular y por ello el médico general o pediatra, que son losque suelen inicialmenteobservara estospacientes, debenconocer la existencia de esta patología, su diagnóstico y tratamiento precoz. De todas formas, aunque la situación anatómica del testículo y su contenido permiten realizar una exhaustiva exploración física, desgraciadamente todavía la remota posibilidad de una torsión del cordón espermático queda muchas veces descartada del diagnóstico diferencial al no pensar en ella. -

Information for Parents About Retractile Testicles
Patient and Family Education Information for Parents About Retractile Testicles Your son has a retractile testicle. This is not dangerous, but there are some things you should know about this condition. How do testicles develop? During pregnancy, the testicles in boy babies actually grow inside Tunnel the abdominal cavity, not in the scrotum. Four months before Testicles birth, a tunnel formed by the smooth lining of the intestinal To scrotum cavity pushes down through the groin into the scrotum. Between 1-2 months before birth, the testicles move down through his tunnel to be anchored in the scrotum. As the tunnel moves through the abdominal muscles, it is wrapped with some of the muscle tissue. This muscle is called the cremaster muscle. When a boy is cold or nervous the cremaster muscle contracts, pulling the testicle up out of the scrotum and into the groin area. Testicles move through Is it dangerous for my son to have a retractile testicle? tunnel to Tunnel scrotum Closes In some boys, even though the testicle makes the complete trip into the scrotum, that testicle may move up and down along the tunnel. Some doctors believe that this is an exaggerated reflex response. Such testicles are called ‘retractile testes’ because they retract into the groin when the cremaster muscle contracts. This retraction can make it hard to find the testicle on examination. Sometimes it may be difficult to tell the difference between a retractile testicle and an undescended testicle (one that never made the full trip into the scrotum during development). There are significant differences between the two conditions. -

Anatomy and Physiology of a Bull's Reproductive Tract
Beef Cattle Handbook BCH-2010 Product of Extension Beef Cattle Resource Committee Reproductive Tract Anatomy and Physiology of the Bull E. J. Turman, Animal Science Department Oklahoma State University T. D. Rich, Animal Science Department Oklahoma State University The reproductive tract of the bull consists of the testicles normally and usually produces enough sperm so that and secondary sex organs, which transport the sperma- the male will be of near normal fertility. However, since tozoa from the testicle and eventually deposits them in this condition appears to have a hereditary basis, such the female reproductive tract. These organs are the epi- males should not be used for breeding. If both testicles didymis, vas deferens and penis, plus three accessory are retained, the male will be sterile. sex glands, the seminal vesicles, prostate and Cowper’s Usually, hormone production is near normal in the gland. This basic anatomy is illustrated in figure 1 as a cryptorchid testicle and the male develops and behaves greatly simplified diagrammatic sketch. like a normal male. If the retained testicle is not The testicle has two very vital functions: (1) produc- removed at time of castration, the male will develop the ing the spermatozoa; and (2) producing the specific secondary sex characters of an uncastrated male. This male hormone, testosterone. The testicles are located operation is not as simple, nor as safe, as removing tes- outside of the body cavity in the scrotum. This is essen- ticles that are in the scrotum. Thus, it is recommended tial for normal sperm formation since this occurs only at to select against this trait by culling cryptorchid males. -

Leydig Cell Tumor of the Testis
Odaba ş et al. Eastern Journal of Medicine 3 (2): 78-79, 1998. Leydig cell tumor of the testis ODABAŞ Ö.1, DİLEK F.H.2, AVANOĞLU H.1, ATILLA M.K.1, YILMAZ Y.1, AYDIN S.1 Departments of Urology1 and Pathology School of Medicine, Yüzüncü Yıl University, Van Key words Testicle, Leydig cell tumor, adult had bilateral testicular Leydig cell tumor with adrenocortical adenoma and suggested to examine Introduction the adrenal gland in patients with testicular Leydig cell tumors (4). Adult patients may present with Leydig cell tumor is a rare form of testicular gynaecomastia, loss of libido, feminine hair neoplasm. It represents only 1 to 3 percent of all distribution and genital under-development. testicular tumors although it is the most common Testicular swelling is usually present, but where a form of the sex cord-mesenchyme tumors. The discrete tumor mass is not palpable , ultrasound is majority have been recognized in males between the extremely useful in confirming the presence of a ages of 20 and 60 years. However approximately one tumor (5). In our case, the patient admitted with fourth have been reported before puberty (1). tescular swelling as reported usually, not with The etiology of Leydig cell tumors is unknown. In hormonal disturbance. contrast to germ cell tumors, there is no correlation with cryptorchidism. Causing experimental production of Leydig cell tumor in mice following chronic estrogen administration or intrasplenic testicular autografting shows its hormonal basis (1). In addition, estrogen and progesterone receptors were detected in about 70 per cent of the Leydig tumor cells in an immunohistologic study, though no receptor was observed in normal Leydig cells (2). -

THE UNIVERSITY of EDINBURGH
THE UNIVERSITY of EDINBURGH Title Urethroscopy: an aid to diagnosis, treatment and prognosis of urethral conditions in the male due to gonorrhoea Author McFarlane, Wilfrid Qualification MD Year 1919 Thesis scanned from best copy available: may contain faint or blurred text, and/or cropped or missing pages. Digitisation Notes: • Page 8 of Supplement at back is missing Scanned as part of the PhD Thesis Digitisation project http://librarvblogs.is.ed.ac.uk/phddigitisation URETHROSCOPY an aid to Diagnosis, Treatment and Prognosis of Urethral Conditions in the Male due to GONORRHOEA. "by Wilfrid McFarlane, M.C., M.B., Ch.E. (Edin) L.R.C.P. & S.E. M.O. 9. Stationary Hospital, Havre. 1916 M.O. i/c Gonorrhoeal Division, Military Hospital, Hemel Hempstead. 1918 M.O. Venereal Hospital, Cambridge. Thesis for"the Degree of M.D. - f 1• THE ANATOMY AMD HISTOLOGY OF THE URETHRA AND THE PATHOLOGY OF GONORRHOEA. In order to make a correct diagnosis and to carry out a sound treatment of any disease it is essential to have an accurate knowledge of the anatomy of the l • organ affected and of the pathology of the disease affecting it. THE -ANATOMY OF THE MALE URETHRA. It is merely necessary to bring out those points which will enable one to understand the effect of Gonorrhoea on the urethra, especially in longstanding cases. The urethra is the channel by which urine passes from the bladder to the outside. Into this channel open the ejaculatory ducts and thus it acts also as a passage for the spermatic fluid. In its course from the neck of the bladder to the root of the penis the urethra describes a curve, the concavity of which looks upwards and forwards. -

Eight Days of Water-Only Fasting Promotes Favorable Changes in the Functioning of the Urogenital System of Middle-Aged Healthy Men
nutrients Article Eight Days of Water-Only Fasting Promotes Favorable Changes in the Functioning of the Urogenital System of Middle-Aged Healthy Men Sławomir Letkiewicz 1,2, Karol Pilis 1,* , Andrzej Sl˛ezak´ 1 , Anna Pilis 1, Wiesław Pilis 1, Małgorzata Zychowska˙ 3 and Józef Langfort 4 1 Department of Health Sciences, Jan Długosz University in Cz˛estochowa,42-200 Cz˛estochowa,Poland; [email protected] (S.L.); [email protected] (A.S.);´ [email protected] (A.P.); [email protected] (W.P.) 2 Urological and Andrological Clinic “Urogen”, 42-600 Tarnowskie Góry, Poland 3 Faculty of Physical Education, Department of Sport, Kazimierz Wielki University in Bydgoszcz, 85-091 Bydgoszcz, Poland; [email protected] 4 Institute of Sport Sciences, The Jerzy Kukuczka Academy of Physical Education, 40-065 Katowice, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-34-365-5983 or +48-508-204-403 Abstract: The aim of this study was to determine whether, after 8 days of water-only fasting, there are changes in the efficiency of the lower urinary tract, the concentration of sex hormones, and the symptoms of prostate diseases in a group of middle-aged men (n = 14). For this purpose, before and after 8 days of water-only fasting (subjects drank ad libitum moderately mineralized water), and the following somatic and blood concentration measurements were made: total prostate specific antigen (PSA-T), free prostate specific antigen (PSA-F), follicle stimulating hormone (FSH), luteotropic hormone (LH), prolactin (Pr), total testosterone (T-T), free testosterone (T-F), dehydroepiandrosterone (DHEA), sex hormone globulin binding (SHGB), total cholesterol (Ch-T), β-hydroxybutyrate (β-HB). -

Orchiopexy: Surgery for an Undescended Testicle
In partnership with Primary Children’s Hospital Orchiopexy: Surgery for an undescended testicle Orchiopexy (or-key-oh-PEX-ee) is a procedure that brings the testicle(s) into the scrotum. Why does my child need an orchiopexy? The testicles develop in the abdomen while a baby is in utero and usually move to the scrotum by 6 months old. Your child may need an orchiopexy if their testicle or testicles have not moved to the scrotum by this time. Surgically moving the testicles to the scrotum helps them develop normally and allows healthy growth for future sperm production. What happens during an orchiopexy? During an orchiopexy, your child will be put under general anesthesia. The surgeon will make two small openings in the groin and find the undecended testicle(s). They will make sure the testicle is healthy and then put it into the scrotum. What should I do about nausea When can my child go home after and vomiting? an orchiopexy? After surgery, many children feel nauseated and may Your child can usually go home the same day as the vomit in the first 24 hours. This can be caused by orchiopexy. Watch your child carefully during the medicines during surgery, car movement, or pain ride home to make sure their head and neck don’t medicine after surgery. Help control nausea by: slump forward and close their airway. • Encouraging your child to lie still When can my child eat after • Offering clear liquids, which are important after an orchiopexy? surgery to help prevent dehydration After your child wakes up from surgery, they may • Slowly offering regular foods over a few days until have clear liquids like Pedialyte™, water, apple juice, your child can eat a normal diet sports drinks, ice pops, and plain gelatin. -
Slang for Penis and Testicles
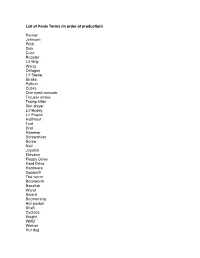
List of Penis Terms (in order of production) Pecker Johnson Prick Dick Cock Rooster Lil' Billy Wang Octagon Lil' Stevie Snake Python Cobra One eyed monster Trouser snake Tramp killer Slut slayer Lil' Buddy Lil' Friend Halfmast Tool Drill Hammer Screwdriver Screw Nail Joystick Elevator Floppy Drive Hard Drive Hardware Gearshift The worm Bookworm Basalisk Wand Sword Boomerang Hot pocket Shaft Cyclops Knight WMD Weiner Hot dog Popsicle Lollipop Kielbalsa Stick Ice Cream Cone Morning Wood The Colonel The Lieutenant The Tank The Battleship The land mine The assault rifle the grenade the machete The water gun Gun Banana Carrot Zuchini Cucumber Pickle The Major The seaman The key My asian buddy The shotgun Water hose Twix Snickers bar Bag of tricks Nuclear missile Hollow point The member Chairman Mao Mallet Pyramid Elephant Fuck Truck The mustang Cane Rod Staff Plug Cigar Nebraska State Capitol Turtle Head Undercover Brother The lightsaber Katana Sniper Rifle The sticky grenade Straw Remote Control The silver bullet Drumstick Bone Mast The machine The goods The hardware Junk Bulge The sequoia Bushwhacker The lawnmower Hoover tower The Washington monument The Lincoln memorial The pocket monster The pocket rocket The mongoose The ground squirrel The trombone Dong Torpedo Sausage Philly Cheesesteak The pendulum Babymaker Toy soldier Antenna The titanic Zeus Ares List of Testicle Terms (in order of production) Balls Stones Family Jewels Meatballs Reece's Pieces Nuts Coconuts Weights Walnuts Gonads Dumbbells Truffles The sperm factory Peanuts Chestnuts Package Grenades Huevos Water Balloons Wheels Itchy and scratchy Beavis and butthead Tweedledee and Tweedledum Easter eggs Fiery Coals Jellybeans Sack The two amigos Maracas. -

Epididymo-Orchitis-Leaflet Epididymo-Orchitis
Page 1 of 4 View this article online at: patient.info/health/epididymo-orchitis-leaflet Epididymo-orchitis Epididymo-orchitis is an inflammation of the epididymis and/or testicle (testis). It is usually due to infection, most commonly from a urine infection or a sexually transmitted infection. A course of antibiotic medicine will usually clear the infection. Full recovery is usual. Complications are uncommon. What is epididymo-orchitis? Epididymitis means inflammation of the epididymis (the structure next to the testicle (testis) that is involved in making sperm). Orchitis means inflammation of a testicle. As the epididymis and testis lie next to each other, it is often difficult to tell if the epididymis, the testis, or both are inflamed. Therefore, the term epididymo-orchitis is often used. What causes epididymo-orchitis? Most cases are due to an infection. Causes of infection include the following: A complication from a urine infection Germs (bacteria) such as E. coli that cause urine infections can sometimes track down the vas deferens to cause an epididymo-orchitis. This can happen at any age and is the most common cause of epididymo-orchitis in men aged over 35 years. This is because partial blockage of urine flow becomes more common with increasing age, due an enlarged prostate or narrowing of the urethra (urethral stricture). The urethra is the tube that urine flows out of from the bladder. Partial blockage of urine makes you more prone to develop urine infections. A complication of a urine infection is also the usual cause of epididymo-orchitis in young boys. Page 2 of 4 Sexually transmitted infection A sexually transmitted infection is the most common cause of epididymo-orchitis in young men (but can occur in any sexually active man). -

Undescended Testicles Patient Guide Table of Contents Pediatric Health Committee
PEDIATRIC HEALTH Undescended Testicles Patient Guide Table of Contents Pediatric Health Committee CHAIR Pediatric Health Committee . 2 T. Ernesto Figueroa, MD Kenny's Story . 3 Nemours/Alfred I . DuPont Hospital for Children Introduction: When Your Baby Boy Is Born . 4 Wilmington, DE GET THE FACTS . 5 How Does the Male Reproductive System Form? . 5 What Are Undescended Testicles (Cryptorchidism)? . 5 COMMITTEE MEMBERS What Causes this Problem? . 6 Paul Austin, MD GET DIAGNOSED . 6 Washington University School of Medicine in St . Louis GET TREATED . 7 St. Louis, MO AFTER TREATMENT . 7 GLOSSARY . 8 Ahmad Bani-Hani, MD QUESTIONS TO ASK YOUR DOCTOR . 9 Nemours/Alfred I . DuPont Hospital for Children About the Urology Care Foundation . [back cover] Wilmington, DE Michael Hsieh, MD Children’s National Health System Washington, DC 2 Kenny's Story When our son Kenny K* was born, we were so happy! He was absolutely beautiful . We were in love at first sight . He had all of his fingers and toes and looked like an angel . However, at three months old, we noticed that his genitals didn’t look right . We took him to his doctor and the pediatrician said he had an undescended testicle . Kenny’s pediatrician referred us to a specialist called “a pediatric urologist .” His urologist said an undescended testicle is a common problem and could easily be fixed . Everything else with Kenny was normal . After talking about all of our options, Kenny’s urologist recommended that he have surgery . After the surgery, Kenny didn’t have any other issues . He is growing up fine and doesn’t even know he had an issue .