3Rd Global Vaccine Congress
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gavi's Vaccine Investment Strategy
Gavi’s Vaccine Investment Strategy Deepali Patel THIRD WHO CONSULTATION ON GLOBAL ACTION PLAN FOR INFLUENZA VACCINES (GAP III) Geneva, Switzerland, 15-16 November 2016 www.gavi.org Vaccine Investment Strategy (VIS) Evidence-based approach to identifying new vaccine priorities for Gavi support Strategic investment Conducted every 5 years decision-making (rather than first-come- first-serve) Transparent methodology Consultations and Predictability of Gavi independent expert advice programmes for long- term planning by Analytical review of governments, industry evidence and modelling and donors 2 VIS is aligned with Gavi’s strategic cycle and replenishment 2011-2015 Strategic 2016-2020 Strategic 2021-2025 period period 2008 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 RTS,S pilot funding decision VIS #1 VIS #2 VIS #3 MenA, YF mass campaigns, JE, HPV Cholera stockpile, Mid 2017 : vaccine ‘long list’ Rubella, Rabies/cholera studies, Oct 2017 : methodology Typhoid Malaria – deferred Jun 2018 : vaccine shortlist conjugate Dec 2018 : investment decisions 3 VIS process Develop Collect data Develop in-depth methodology and Apply decision investment decision framework for cases for framework with comparative shortlisted evaluation analysis vaccines criteria Phase I Narrow long list Phase II Recommend for Identify long list to higher priority Gavi Board of vaccines vaccines approval of selected vaccines Stakeholder consultations and independent expert review 4 Evaluation criteria (VIS #2 – 2013) Additional Health Implementation -

Yellow Fever 2016
Resident / Humanitarian Coordinator Report on the use of CERF funds RESIDENT / HUMANITARIAN COORDINATOR REPORT ON THE USE OF CERF FUNDS ANGOLA RAPID RESPONSE YELLOW FEVER 2016 RESIDENT/HUMANITARIAN COORDINATOR Pier Paolo Balladelli REPORTING PROCESS AND CONSULTATION SUMMARY a. Please indicate when the After Action Review (AAR) was conducted and who participated. Review agreed on 02/09/2016 and 07/09/2016. b. Please confirm that the Resident Coordinator and/or Humanitarian Coordinator (RC/HC) Report was discussed in the Humanitarian and/or UN Country Team and by cluster/sector coordinators as outlined in the guidelines. YES NO c. Was the final version of the RC/HC Report shared for review with in-country stakeholders as recommended in the guidelines (i.e. the CERF recipient agencies and their implementing partners, cluster/sector coordinators and members and relevant government counterparts)? YES NO Final version shared with UNICEF and UNDP, although this initiative was mainly implemented by WHO 2 I. HUMANITARIAN CONTEXT TABLE 1: EMERGENCY ALLOCATION OVERVIEW (US$) Total amount required for the humanitarian response: Source Amount CERF 3,000,000 Breakdown of total response COUNTRY-BASED POOL FUND (if applicable) 4,508,559 funding received by source OTHER (bilateral/multilateral) TOTAL 10,473,618 *The total amount does not match because this was considered an underfunded emergency. TABLE 2: CERF EMERGENCY FUNDING BY ALLOCATION AND PROJECT (US$) Allocation 1 – date of official submission: 06/04/2016- 05/10/2016 Agency Project code Cluster/Sector -

Hanna Nohynek @Hnohynek
Biosketch Hanna Nohynek @hnohynek Hanna Nohynek is Chief Physician and Deputy Head of the Infectious Diseases Control and Vaccines Unit of the Department of Health Security at the Finnish Institute for Health and Welfare. She serves as secretary of the Finnish NITAG (KRAR), and leads the subgroup on Strategic development of the influenza vaccination programme and the subgroup on the SARS-CoV-2 vaccination strategy. She practices clinical medicine at a travel health clinic in Aava, Helsinki. She was instrumental in designing the first THL (KTL) health advisory for refugees and asylum seekers in Finland, studying the narcolepsy signal post pandemic vaccination, designing the introduction of the HPV vaccine to the national immunization programme, and the introduction of the live attenuated influenza vaccine for children. Her present research interests are register-based vaccine impact studies, evidence based policy/decision making, vaccine safety, hesitancy, SARS-CoV-2, RSV, influenza and pneumococcus. She coordinates the work packages on field studies and communication for IMI DRIVE on brand specific influenza vaccine effectiveness (www.drive-eu.org). She has authored more than 130 original articles (including the first scientific report on the association between pandemic influenza vaccination and narcolepsy), and she teaches, giving over 30 invited lectures annually and guiding elective, graduate and PhD students (presently Raija Auvinen and Idil Hussein). She belongs to the external faculty of the University of Tampere MSc course on Global Health. She has served on expert committees evaluating HBV, PCV and rota virus vaccines in Finland, and as an advisor to the EU, IMI, IVI, WHO, GAVI, SIDA/SRC, and the Finnish MOFA. -

UNEP Mercury Treaty Protects Access to Thiomersal-Containing Vaccines
UNEP mercury treaty protects access to thiomersal-containing vaccines United Nations Environment Program has developed a treaty on mercury in an effort to protect human health and the environment by limiting mercury releases. In the course of the negotiations, a proposal was made to restrict vaccines that contain the preservative thiomersal under a section of the treaty that prohibits trade of mercury-added products. The implications of restricting thiomersal, an ethyl mercury-containing preservative, would be significant. According to SAGE, “Thiomersal-containing vaccines [are] safe, essential, and irreplaceable components of immunization programs, especially in developing countries, and…removal of these products would disproportionately jeopardize the health and lives of the most disadvantaged children worldwide.” The treaty annex that describes prohibited products specifically excludes “vaccines containing thiomersal as preservatives” under a short list of products the authors intended to emphasize were to be protected. Protecting access to vaccines came as the result of a strong partnership between WHO, UNICEF, GAVI, and civil society advocates and experts around the world to educate country delegates, who predominantly came from ministries of environment. This was also a wonderful partnership with animal health experts, who similarly rely on thiomersal for veterinary vaccines. By facilitating communication between ministries of health and ministries of environment, strong statements are made by delegates about the essential role of thiomersal-containing vaccines in protecting human health. PATH will be collecting and disseminating additional information about how the community came together around this issue and lessons learned in the coming months. . -
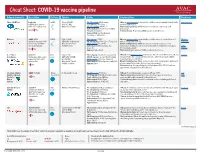
Cheat Sheet: COVID-19 Vaccine Pipeline
Cheat Sheet: COVID-19 vaccine pipeline Primary sponsor(s) Description Platform Funders Status Considerations Read more Pfizer / BioNTech Comirnaty mRNA Pfizer ($500M) Ph. I/II ongoing: 456/Germany Efficacy: Interim analysis shows that the candidate was safe and well-tolerated with New York Times mRNA that encodes for USG ($1.9M) Ph. II planned: 960/China an efficacy rate of 95%. SARS-CoV-2 spike protein. Warp Speed Finalist Ph. II/III ongoing: 44K US +5 Manufacturing/delivery: mRNA vaccines are relatively easy to scale and Authorization: EUA in EU, US, +9; WHO manufacture. Emergency Validation Platform history: No previous mRNA vaccines licensed for use. Approval: Bahrain, New Zealand, Saudi Arabia, Switzerland Moderna mRNA-1273 mRNA USG ($2.48B) Ph. I ongoing: 155/US Efficacy: Interim analysis shows that the candidate was safe and well-tolerated Moderna Synthetic messenger RNA CEPI/GAVI (Undisclosed) Ph. II/III ongoing: 3000 (12 to 17 years)/ US with an efficacy rate of 94.5%. Statement that encodes for SARS- Warp Speed Finalist Ph. III ongoing: 30,000/US Manufacturing/delivery: mRNA vaccines are relatively easy to scale and CoV-2 spike protein. COVAX Portfolio Authorization: EUA in Canada, EU, manufacture (potential for 1B doses by 2022); likely to require two doses, but a AVAC Israel, US third may be necessary. Webinar Approval: Switzerland Platform history: No previous mRNA vaccines licensed for use. U. of Oxford AZD1222 Viral USG ($1.2B) Ph. II ongoing: 300 vols (6-17 years)/ UK Efficacy: Ph. III interim analysis shows vaccine was safe and well-tolerated, efficacy Science AstraZeneca Chimpanzee Adeno vector vector CEPI/GAVI ($750M) Ph. -

Yellow Fever Vaccine
Yellow Fever Vaccine: Current Supply Outlook UNICEF Supply Division May 2016 0 Yellow Fever Vaccine - Current Supply Outlook May 2016 This update provides revised information on yellow fever vaccine supply availability and increased demand. Despite slight improvements in availability and the return of two manufacturers from temporary suspension, a constrained yellow fever vaccine market will persist through 2017, exacerbated by current emergency outbreak response requirements. 1. Summary Yellow fever vaccine (YFV) supply through UNICEF remains constrained due to limited production capacity. Despite the return of two manufacturers from temporary suspension, the high demand currently generated from the yellow fever (YF) outbreak in Angola, in addition to potential increased outbreak response requirements in other geographic regions, outweigh supply. The demand in response to the current YF outbreak in Angola could negatively impact the supply availability for some routine immunization programme activities. UNICEF anticipates a constrained global production capacity to persist through 2017. UNICEF has long-term arrangements (LTAs) with four YFV suppliers to cover emergency stockpile, routine immunization, and preventative campaign requirements. During 2015, UNICEF increased total aggregate awards to suppliers to reach approximately 98 million doses for 2016- 2017. However, whereas supply can meet emergency stockpile and routine requirements, it is insufficient to meet all preventive campaign demands, which increased the total demand through UNICEF to 109 million doses. The weighted average price (WAP) per dose for YFV increased 7% a year on average since 2001, from US$ 0.39 to reach US$ 1.04 in 2015. Given the continued supply constraints, UNICEF anticipates a YFV WAP per dose of US$1.10 in the near-term. -
An Overview of COVID Vaccine Clinical Trial Results & Some Challenges
An overview of COVID vaccine clinical trial results & some challenges DCVMN Webinar December 8th, 2020 Access to COVID-19 tools ACCESSACCESS TO TOCOVID-19 COVID-19 TOOLS TOOLS (ACT) (ACT) ACCELERATOR ACCELERATOR (ACT) accelerator A GlobalA GlobalCollaboration Collaboration to Accelerate tothe AccelerateDevelopment, the Production Development, and Equitable Production Access to New and Equitable AccessCOVID-19 to New diagnostics, COVID-19 therapeutics diagnostics, and vaccines therapeutics and vaccines VACCINES DIAGNOSTICS THERAPEUTICS (COVAX) Development & Manufacturing Led by CEPI, with industry Procurement and delivery at scale Led by Gavi Policy and allocation Led by WHO Key players SOURCE: (ACT) ACCELERATOR Commitment and Call to Action 24th April 2020 ACT-A / COVAX governance COVAX COORDINATION MEETING CEPI Board Co-Chair: Jane Halton Co-Chair: Dr. Ngozi Gavi Board Workstream leads + DCVMN and IFPMA-selected Reps As needed – R&D&M Chair; COVAX IPG Chair Development & Manufacturing Procurement and delivery Policy and allocation (COVAX) at scale Led by (with industry) Led by Led by R&D&M Investment Committee COVAX Independent Product Group Technical Review Group Portfolio Group Vaccine Teams SWAT teams RAG 3 COVAX SWAT teams are being set up as a joint platform to accelerate COVID- 19 Vaccine development and manufacturing by addressing common challenges together Timely and targeted Multilateral Knowledge-based Resource-efficient Addresses specific cross- Establishes a dialogue Identifies and collates Coordinates between developer technical and global joint effort most relevant materials different organizations/ challenges as they are across different COVID-19 and insights across the initiatives to limit raised and/or identified vaccines organizations broader COVID-19 duplications and ensure on an ongoing basis (incl. -

Human Papillomavirus Vaccine
Human Papillomavirus Vaccine: Supply and Demand Update UNICEF Supply Division October 2020 0 Human Papillomavirus Vaccine Supply and Demand Update - October 2020 This update provides information on human papillomavirus vaccine, including supply, demand, and pricing trends. It highlights continued supply constraints foreseen over 2020 and 2021, which also affects countries procuring through UNICEF. UNICEF requests self-financing middle-income countries to consolidate credible multi-year demand and to submit multi-year commitments through UNICEF. 1. Summary • UNICEF’s strategic plan for 2018-2021 seeks to ensure that at least 24 countries nationally introduce human papillomavirus (HPV) vaccine into their immunization programmes.1 As of to date, 20 countries supplied through UNICEF, of which 15 supported by Gavi, the Vaccine Alliance (Gavi) and five countries having transitioned from Gavi support and self-finance their procurement, have introduced HPV vaccines since 2013. Fourteen middle-income countries (MICs) are also procuring HPV vaccines through UNICEF. From 2013 to 2019, UNICEF’s total HPV vaccine procurement reached 30.9 million doses in support of girls. There is currently no gender-neutral programmes in countries supplied through UNICEF. Of the 30.9 million doses, UNICEF procured 28.3 million doses (91 per cent) for countries supported by Gavi, including those that transitioned from Gavi support and still access Gavi prices, and 2.6 million doses (9 per cent) on behalf of self-financing MICs. • In December 2016, Gavi revised its programme strategy to support full-scale national HPV vaccine introductions with multi-age cohort (MAC) vaccinations. This substantially increased HPV vaccine demand through UNICEF from 2017. -

'Astrazeneca' Covid-19 Vaccine
Medicines Law & Policy How the ‘Oxford’ Covid-19 vaccine became the ‘AstraZeneca’ Covid-19 vaccine By Christopher Garrison 1. Introduction. The ‘Oxford / AstraZeneca’ vaccine is one of the world’s leading hopes in the race to end the Covid-19 pandemic. Its history is not as clear, though, as it may first seem. The media reporting about the vaccine tends to focus either on the very small (non-profit, academic) Jenner Institute at Oxford University, where the vaccine was first invented, or the very large (‘Big Pharma’ firm) AstraZeneca, which is now responsible for organising its (non-profit) world-wide development, manufacture and distribution. However, examining the intellectual property (IP) path of the vaccine from invention to manufacture and distribution reveals a more complex picture that involves other important actors (with for-profit perspectives). Mindful of the very large sums of public money being used to support Covid-19 vaccine development, section 2 of this note will therefore contextualise the respective roles of the Jenner Institute, AstraZeneca and these other actors, so that their share of risk and (potential) reward in the project can be better understood. Section 3 provides comments as well as raising some important questions about what might yet be done better and what lessons can be learned for the future. 2. History of the ‘Oxford / AstraZeneca’ vaccine. 2.1 Oxford University and Oxford University Innovation Ltd. The Bayh-Dole Act (1980) was hugely influential in the United States and elsewhere in encouraging universities to commercially exploit the IP they were generating by setting up ‘technology transfer’ offices. -

GAVI HPV Vaccine Infographic Pdf, 765Kb
SAVING LIVES AND PROTECTING HEALTH THROUGH IMMUNISATION GAVI ALLIANCE TACKLES CERVICAL CANCER IN DEVELOPING COUNTRIES EVERY YEAR, 275,000 WOMEN DIE OF CERVICAL CANCER. OVER 85% OF THOSE DEATHS ARE IN DEVELOPING COUNTRIES COUNTRIES ELIGIBLE FOR GAVI’S HPV VACCINE FUNDING 1 10 30 SCALE: CERVICAL CANCER DEATHS PER 100,000 COUNTRIES WITH NATIONAL HPV VACCINE PROGRAMMES FRANCE 1.8 DEATHS PER 100,000 KOREA, DPR UNITED STATES OF AMERICA 3.3 DEATHS PER 100,000 1.7 DEATHS PER 100,000 LAO PDR HAITI 13.3 DEATHS PER 100,000 10.1 DEATHS PER 100,000 NICARAGUA 20.6 DEATHS PER 100,000 SIERRA LEONE 33.0 DEATHS PER 100,000 PAPUA NEW GUINEA 17.6 DEATHS PER 100,000 TANZANIA 17.6 DEATHS PER 100,000 37.5 DEATHS PER 100,000 MALAWI COUNTRIES WITH NATIONAL 38.3 DEATHS PER 100,000 MOZAMBIQUE HPV VACCINE PROGRAMMES 34.5 DEATHS PER 100,000 AUSTRALIA 1.4 DEATHS PER 100,000 COUNTRIES WITHOUT NATIONAL 1.4 DEATHS PER 100,000 HPV VACCINE PROGRAMMES ARGENTINA 7.4 DEATHS PER 100,000 Licensed under Creative Commons Attribution-NonCommercial-NoDerivs National HPV Programs source: CourtesyCourtesy ofof PATH,PATH, AprilApril 20132013 CervicalCervical cancercancer mortailitymortaility raterate source:source: GLOBOCAN 2008, globocan.iarc.fr CHANGING THE BALANCE HIGH-INCOME ABOUT HPV VACCINE LOWERING THE PRICE DRAMATIC ACCELERATION COUNTRIES Current lowest InIn wealthywealthy countriescountries public price, circa: thethe samesame vaccinesvaccines DEVELOPING By 2020, over million cancan costcost moremore than:than: COUNTRIES US$ 13 30 girls US$ 100 Price achieved in more countries by GAVI: by GAVI: than 40 US$ 4.50 will be vaccinated against HPV GAVI’s support for HPV vaccines will help Safe and effective, human papillomavirus The new low price of US $4.50 per dose redress the inequity, delivering vaccines to (HPV)(HPV) vaccinesvaccines protectprotect againstagainst 70%70% ofof marks a two-thirds reduction on the The first GAVI-supported HPV vaccines countries with the highest burden. -

Gavi's Vaccine Investment Strategy
Gavi’s Vaccine Investment Strategy Judith Kallenberg, Head of Policy WHO Product Development for Vaccines Advisory Committee Meeting Geneva, Switzerland, 7-9 September 2015 www.gavi.org Vaccine Investment Strategy (VIS) Evidence-based approach to identifying potential new vaccine priorities for Gavi support • Evidence review, analyses, stakeholder consultations, independent expert advice 2008 VIS: • HPV, rubella, JE, typhoid 2013 VIS: • Expanded support for yellow fever campaigns • Time-limited contribution to global cholera stockpile • Learning agenda: rabies and cholera studies to fill evidence gaps • Malaria vaccines to be re-assessed in 2015/16 2 VIS process (phase 1) 1. WHO ‘landscape analysis’ of vaccines in scope: anticipated licensure within next 5 years 2. Development of prioritisation criteria through Gavi stakeholder consultations 3. Assessment of vaccines against criteria 4. Development vaccine shortlist for in-depth analysis 2013 vaccines considered: Existing vaccines not ‘Pipeline’ Potential expansion of supported by GAVI vaccines GAVI vaccine support Cholera Malaria DTP (booster) Hepatitis A Dengue Hepatitis B (birth dose) Hepatitis E Enterovirus 71 Measles (additional campaigns) Influenza Meningococcal (additional serotypes) Mumps Yellow Fever (additional campaigns) Poliomyelitis Rabies 3 Evaluation criteria and indicators Category VIS Criteria Phase I Indicator U5 future deaths averted, 2015 – 2030 Impact on child mortality U5 future deaths averted per 100,000 vaccinated population Total future deaths averted, 2015 – 2030 -
The GAVI Alliance
GLOBAL PROGRAM REVIEW The GAVI Alliance Global Program Review The World Bank’s Partnership with the GAVI Alliance Main Report and Annexes Contents ABBREVIATIONS .................................................................................................................................. V ACKNOWLEDGMENTS ........................................................................................................................ XI PROGRAM AT A GLANCE: THE GAVI ALLIANCE ............................................................................ XII KEY BANK STAFF RESPONSIBLE DURING PERIOD UNDER REVIEW ........................................ XIV GLOSSARY ......................................................................................................................................... XV OVERVIEW ........................................................................................................................................ XVII GAVI ALLIANCE MANAGEMENT RESPONSE .............................................................................. XXV WORLD BANK GROUP MANAGEMENT RESPONSE ................................................................... XXIX CHAIRPERSON’S SUMMARY ......................................................................................................... XXXI 1. THE WORLD BANK-GAVI PARTNERSHIP AND THE PURPOSE OF THE REVIEW ...................... 1 Evolution of GAVI .....................................................................................................................................................