Advanced Hemodynamics CACCN.Key
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Accuracy of Alternatives to Mercury Sphygmomanometers OCTOBER 2009
HEALTH CARE RESEARCH COLLABORATIVE The Accuracy of Alternatives to Mercury Sphygmomanometers OCTOBER 2009 A U T H O R : Susan Buchanan, MD, MPH Health Care Without Harm has initiated a research collaborative coordinated by faculty of the University of Illinois at Chicago School of Public Health, with support from the Pioneer Portfolio of the Robert Wood Johnson Foundation, aimed at stimulating collaborative research around health and safety improvements in health care. This collaborative is designed to increase the evidence base concerning the human health and environmental impacts of materials, products and practices within health care. In partnership with the Global Health and Safety Initiative (GHSI), the Research Collaborative is engaged in research directed at the intersection of environmental, patient, and worker safety issues related to building and operating health care institutions. This paper is the third in a series of papers in which the Collaborative provides research and analysis of factors influencing patient, worker and environmental safety and sustainability in the healthcare sector. The editors of this series are Peter Orris, MD, MPH and Susan Kaplan, JD. TABLE OF CONTENTS Executive Summary .......................................................................................................................................3 I. Introduction .........................................................................................................................................4 II. Methods ...............................................................................................................................................7 -

Who Technical Specifications for Automated Non-Invasive Blood Pressure Measuring Devices with Cuff
WHO TECHNICAL SPECIFICATIONS FOR AUTOMATED NON-INVASIVE BLOOD PRESSURE MEASURING DEVICES WITH CUFF WHO MEDICAL DEVICE TECHNICAL SERIES fully automated cuff 01 WHO TECHNICAL SPECIFICATIONS FOR AUTOMATED NON-INVASIVE BLOOD PRESSURE MEASURING DEVICES WITH CUFF WHO MEDICAL DEVICE TECHNICAL SERIES WHO technical specifications for automated non-invasive blood pressure measuring devices with cuff ISBN 978-92-4-000265-4 (electronic version) ISBN 978-92-4-000266-1 (print version) © World Health Organization 2020 Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO technical specifications for automated non-invasive blood pressure measuring devices with cuff. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -
Module 10: Vital Signs
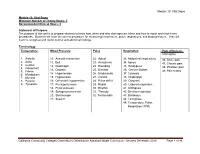
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Aneroid Sphygmomanometer for Five Minutes
Low Level Disinfection Prepare Enzol enzymatic detergent according to the manufacturer’s instructions. Spray detergent solution liberally onto cuff and use a sterile brush to agitate the detergent so- lution over entire cuff surface for five minutes. Rinse continuously with distilled water Aneroid Sphygmomanometer for five minutes. To disinfect, first follow the cleaning steps above, then spray cuff with 10% bleach solution until saturated, agitate with a sterile brush over entire cuff surface for five minutes. Rinse continuously with distilled water for five minutes. Wipe off excess water with sterile cloth and allow cuff to air dry. Use, Care, & Maintenance ! CAUTION: Do not iron cuff. ! CAUTION: Do not heat or steam sterilize cuff. Manometer Quality Control A Serial number and Lot number are (Figure 4) automatically assigned to every aneroid during manufacturing, ensuring every item is "controlled". The Serial Number can be located on the faceplate of each aneroid (Figure 4). Serial Number The Lot number is located on the the box end label (Figure 5). Lot Number Warranty The manufacturer warrants its products against defects in materials and workmanship REF 0000 LOT 0 00000 000 ADC under normal use and service as follows: DIAGNOSTIXTM Hauppauge, NY Aneroid • Warranty service extends to the original retail purchaser only and commences SIZE: Adult ! with the date of delivery. COLOR: Black 0000-00 CONTENTS: 1 ea ***LATEX-FREE*** (Figure 5) Warranty duration is as follows: Manometer Inflation System 5 YEARS 1 YEAR 10 YEARS 1 YEAR 20 YEARS 3 YEARS Standards LIFE 3 YEARS ANSI/AAMI/ISO 81060-1:2007 • ANSI/AAMI SP-10:2002 *Refer to box end panel for specific warranty duration. -

Recommended Technique for Measuring Blood Pressure Using a Sphygmomanometer and Stethoscope1.Pdf
Nursing Management of Hypertension Table 2: Recommended technique for measuring blood pressure using a sphygmomanometer and stethoscope Reproduced with permission. Canadian Medical Association, 1999. I. Measurement should be taken with a sphygmomanometer known to be accurate. Although a mercury manometer may be preferable, a recently calibrated aneroid or a validated and recently calibrated electronic device can be used. Aneroid devices and mercury columns need to be clearly visible at eye level. II. Choose a cuff with an appropriate bladder width matched to the size of the arm. III. Place the cuff so that the lower edge is 3 cm above the elbow crease and the bladder centered over the brachial artery. The client should be resting comfortably for 5 minutes in the seated position with back support. The arm should be bare and supported with the antecubital fossa at heart level, as a lower position will result in erroneously higher systolic blood pressure and diastolic blood pressure. There should be no talking and client’s legs should not be crossed. At least two measurements should be taken in the same arm with the client in the same position. Blood pressure should also be assessed after 2 minutes of standing, and at times when clients report symptoms suggestive of postural hypotension. Supine blood pressure measurements may also be helpful in the assessment of elderly in those with diabetes. IV. Increase the pressure rapidly to 30 mmHg above the level at which the radial pulse is extinguished (to exclude the possibility of a systolic auscultatory gap). Continue to auscultate at least 10 mmHg below phase V* to exclude a diastolic auscultatory gap. -

Aneroid Sphygmomanometers Instructions & Warranty Thank You for Your Purchase Thank You for Choosing a Prestige Medical® Aneroid Sphygmomanometer
Aneroid Sphygmomanometers Instructions & Warranty Thank you for your purchase Thank you for choosing a Prestige Medical® aneroid sphygmomanometer. Prestige Medical® is very proud of its fine reputation for supplying preci- sion medical products while delivering the highest level of service to the health care professional. Your Prestige Medical® aneroid sphygmomanometer has been subjected to the strictest of standards in manufacturing and quality assurance test- ing. With proper care and maintenance your instrument will provide you with years of dependable service. Please review this manual to become familiar with the ! recommended practices for using and caring for your aneroid sphygmomanometer. Please see page 13 for Warranty details 1 Gauge Calibration The indicator needle should always rest within the rectangular calibration area. If this is not the case, your gauge needs to be recalibrated to within 3mmHg when compared to a certified reference standard. If recalibration is ! required, please refer to your warranty and return instructions on page 13. Note: The gauge is still ! fully calibrated even if the needle is on the line of the calibration recatagle. 2 Aneroid Sphygmomanometer Anatomy Range Marking Index Hook & Loop (reverse side) Marking Closure Gauge Holder Cuff Cuff Size Gauge Clip (reverse side) Artery Aneroid Indicator Manometer Label Gauge End Inflation Valve Bulb Air Release Bladder Valve Tube (Hose) 3 Manometer Gauge Anatomy Hook & Loop Closure Lens Lens Retaining Ring (Rim) Faceplate Needle Cuff Size Gauge Clip (reverse side) Graduation Aneroid Marks Manometer Serial Gauge Number Calibration Rectangle (or Oval) Bellow Chamber Air Stem (Connects to Bladder Tube) Bladder Tube (Hose) 4 Cuff Positioning The cuff should be placed over the bare upper arm with the bladder side over the brachial artery. -

Blood Pressure Measurement
Blood Pressure Measurement PhDr. Mária Sováriová Soósová, PhD. Training for Students 1. – 15. September 2019 UPJŠ, Košice, Slovakia Blood Pressure Blood pressure may be defined as the force of blood inside the blood vessels against the vessel walls. (Marieb and Hoehn, 2010 according to Dougherty, L., Lister, S., 2015) Blood pressure Systolic BP – is the peek pressure of the left ventricule contracting and blood entering the aorta, causing it to strech and there for in parts reflects the function of the left ventricule. Diastolic BP – is when the aortic valve closes, blod flows from the aorta into the smaller vessels and the aorta recoils back. This is when the aortic pressure is at its lowest and tends to reflect the resistance of the blood vessels. (Marieb and Hoehn, 2010 according to Dougherty, L., Lister, S., 2015) Factors influencing BP Age Gender Race Anxiety, fear, pain, emotional stress Medications Hemorrhage Increased intracranial pressure Hormones Diural rhythm Obesity Eating habits Exercise Smoking .......... Aerage and upper limits of blood pressure according to age in mmHg Age Average normal BP Upper limits of normal BP mm Hg mm Hg 1 year 95/65 undetermined 6 – 9 yrs. 100(105)/65 119/79 10 – 13 yrs. 110/65 124/84 14 – 17 yrs. 120/ (75)80 134/83 18 + yrs. 120/80 139/89 Classification of Hypertension ESC/ESH classification of office blood pressurea and definitions of hypertension gradeb (Williams, Mancia, Spiering, et al. 2018, p. 3030) Category Systolic (mmHg) Diastolic (mmHg) Optimal <120 and <80 Normal 120–129 and/or 80–84 High normal - prehypertension 130–139 and/or 85–89 Grade 1 hypertension 140–159 and/or 90–99 Grade 2 hypertension 160–179 and/or 100–109 Grade 3 hypertension ≥180 and/or ≥110 Isolated systolic hypertensionb ≥140 and <90 Methods of BP measuring Invasive - direct: direct in an artery continuous monitoring Noninvasive – indirect: Auscultation – Korotkoff sounds. -

Accurate Blood Pressure Measurement: What It Is, Why It's Important, and How to Ensure Reliable Results
® Modular Diagnostic 2 Station WHITE PAPER Accurate Blood Pressure Measurement: What It Is, Why It’s Important, and How to Ensure Reliable Results Similar to the pressure created by water flowing through a garden hose, blood pressure refers to the force exerted by circulating blood on the walls of our arteries and blood vessels. Blood pressure is commonly measured by inflating a cuff on the upper arm and watching the pressure indicated by a blood pressure gauge while listening to the Korotkoff sounds at the brachial artery with a stethoscope. The cuff must first be inflated enough to stop all the blood from flowing through the artery. Then, as the pressure in the cuff is gradually released with a valve, the occlusion of the artery is reduced. The point at which blood begins to flow again is signaled by the first Korotkoff sound. This is an indication of the peak blood pressure in the arteries and is referred to as systolic blood pressure. Continued reduction of the pressure in the cuff eventually allows the blood to flow completely unobstructed again. This point is signaled by the disappearance of the Korotkoff sounds and is considered a reliable indication of diastolic blood pressure. Typical values for a resting, healthy adult human are approximately 120 mmHg systolic and 80 mmHg diastolic (written as 120/80 mmHg, and spoken as "one twenty over eighty"). Blood pressure varies throughout the day as part of our natural circadian rhythm. Factors such as smoking, stress, drugs, disease, and nutrition also affect blood pressure. Hypertension refers to sustained blood pressure being abnormally high. -

The Mercury Sphygmomanometer Should Be Abandoned Before It Is Proscribed
Journal of Human Hypertension (2000) 14, 31–36 2000 Macmillan Publishers Ltd. All rights reserved 0950-9240/00 $15.00 www.nature.com/jhh ORIGINAL ARTICLE The mercury sphygmomanometer should be abandoned before it is proscribed ND Markandu, F Whitcher, A Arnold and C Carney Blood Pressure Unit, Department of Medicine, St George’s Hospital Medical School, London SW17 ORE, UK Both in clinical practice and medical research, blood cury is a non-degradable pollutant, eventually accumu- pressure is still largely measured by auscultation using lating on the sea bed. The use of mercury in sphygmo- a mercury sphygmomanometer. Blood pressure is the manometers is already in the process of being most important predictor of life expectancy. Treatment eliminated in Scandinavia and Holland and other coun- of high blood pressure reduces strokes, heart attack tries are likely to follow. Our results suggest that mer- and heart failure. Accurate measurement is therefore cury sphygmomanometers are not adequately main- essential. At a large London teaching hospital, just tained and require expertise that is not available for under 500 mercury sphygmomanometers and their accurate measurement of blood pressure. Their use associated cuffs were examined. More than half had should be dispensed with on these grounds before a serious problems that would have rendered them inac- ban for other and, perhaps less justifiable reasons. Vali- curate in measuring blood pressure. At the same time, dated automatic devices, which are less liable to assessment of the technical knowledge needed to mea- measurement and observer error should be used sure blood pressure by the ausculatory technique was instead. -

Sphygmomanometer Calibration Why, How and How Often?
CLINICAL PRACTICE Practice tip Sphygmomanometer calibration Why, how and how often? Martin J Turner BACKGROUND BSc(Eng), MSc(Eng), PhD, is Hypertension is the most commonly managed problem in general practice. Systematic errors in blood pressure Senior Research Asssociate, Departments of Anaesthetics measurements caused by inadequate sphygmomanometer calibration are a common cause of over- and under- and School of Public Health identification of hypertension. Screening and Test Evaluation Programme, University of OBJECTIVE Sydney, New South Wales. This article reviews sphygmomanometer error and makes recommendations regarding in service maintenance and [email protected] calibration of sphygmomanometers. Catherine Speechly DISCUSSION BMedSc, MBBS, FRACGP, is Most sphygmomanometer surveys report high rates of inadequate calibration and other faults, particularly in aneroid Research Officer, Projects, sphygmomanometers. Automatic electronic sphygmomanometers produce systematic errors in some patients. All Research and Development Unit, The Royal Australian sphygmomanometers should be checked and calibrated by an accredited laboratory at least annually. Aneroid College of General sphygmomanometers should be calibrated every 6 months. Only properly validated automatic sphygmomanometers Practitioners, New South should be used. Practices should perform regular in house checks of sphygmomanometers. Good sphygmomanometer Wales. maintenance and traceable sphygmomanometer calibration will contribute to reducing the burden of cardiovascular Noel -

Anatomy and Physiology of the Cardiovascular System
Chapter © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC 5 NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Anatomy© Jonesand & Physiology Bartlett Learning, LLC of © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION the Cardiovascular System © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION OUTLINE Aortic arch: The second section of the aorta; it branches into Introduction the brachiocephalic trunk, left common carotid artery, and The Heart left subclavian artery. Structures of the Heart Aortic valve: Located at the base of the aorta, the aortic Conduction System© Jones & Bartlett Learning, LLCvalve has three cusps and opens© Jonesto allow blood & Bartlett to leave the Learning, LLC Functions of the HeartNOT FOR SALE OR DISTRIBUTIONleft ventricle during contraction.NOT FOR SALE OR DISTRIBUTION The Blood Vessels and Circulation Arteries: Elastic vessels able to carry blood away from the Blood Vessels heart under high pressure. Blood Pressure Arterioles: Subdivisions of arteries; they are thinner and have Blood Circulation muscles that are innervated by the sympathetic nervous Summary© Jones & Bartlett Learning, LLC system. © Jones & Bartlett Learning, LLC Atria: The upper chambers of the heart; they receive blood CriticalNOT Thinking FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Websites returning to the heart. Review Questions Atrioventricular node (AV node): A mass of specialized tissue located in the inferior interatrial septum beneath OBJECTIVES the endocardium; it provides the only normal conduction pathway between the atrial and ventricular syncytia. -

MODELING of ARTERIAL HEMODYNAMICS by Jonathan
MODELING OF ARTERIAL HEMODYNAMICS by Jonathan Edwards A thesis submitted to the Faculty of the University of Delaware in partial fulfillment of the requirements for the degree of Master of Science in Biomechanics and Movement Science Fall 2009 Copyright 2009 Jonathan Edwards All Rights Reserved MODELING OF ARTERIAL HEMODYNAMICS by Jonathan Edwards Approved: __________________________________________________________ William C. Rose, Ph.D. Professor in charge of thesis on behalf of the Advisory Committee Approved: ____________________________________________________ Lynn Snyder-Mackler, Ph.D. Chair of the Biomechanics and Movement Sciences Program Approved: ____________________________________________________ James G. Richards, Ph.D. Deputy Dean of the College of Health Sciences Approved: ____________________________________________________ Debra Hess Norris, M.S. Vice Provost for Graduate and Professional Education ACKNOWLEDGEMENTS I thank Justin Spaeth and Prof. Antony Beris for sharing an early version of the modeling software, which came from Justin’s undergraduate thesis work, with Dr. Rose. I thank Dr. Edwards and Dr. Farquhar for the use of their lab space, their equipment, their supplies, and their advice and expertise. I thank my committee: Dr. Edwards, Dr. Knight, and Dr. Rose for their help and dedication. I thank my fellow graduate student colleagues for being great friends. I thank my advisor, Dr. Rose, for his patience and care; I could not have wished for a better mentor, and more importantly, companion. Finally, I thank