Q3D(R1) Elemental Impurities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang Et Al
US007074961B2 (12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang et al. (45) Date of Patent: Jul. 11, 2006 (54) ANTIDEPRESSANTS AND THEIR 6.211,171 B1 4/2001 Sawynok et al. ANALOGUES AS LONG-ACTING LOCAL 6,545,057 B1 4/2003 Wang et al. ANESTHETCS AND ANALGESCS 2001/0036943 A1 11/2001 Coe et al. (75) Inventors: Ging Kuo Wang, Westwood, MA (US); FOREIGN PATENT DOCUMENTS Peter Gerner, Weston, MA (US); Donald K. Verrecchia, Winchester, MA CH 534124 A 2, 1973 (US) WO WO95/17903 A1 7, 1995 WO WO95/1818.6 A1 7, 1995 (73) Assignee: The Brigham and Women's Hospital, WO WO 99.59.598 A1 11, 1999 Inc., Boston, MA (US) WO WO O2/060870 A2 8, 2002 (*) Notice: Subject to any disclaimer, the term of this OTHER PUBLICATIONS patent is extended or adjusted under 35 U.S.C. 154(b) by 451 days. Luo et al., Xenobiotica, vol. 25, No. 3, pp. 291-301, 1995.* (21) Appl. No.: 10/117,708 Ehlert et al., The Interaction of Amitriptyline, Doxepin, Imipramine and Their N-Methyl Quaternary Ammonium (22) Filed: Apr. 4, 2002 Derivatives with Subtypes of Muscarinic Receptors in Brain (65) Prior Publication Data and Heart, The Journal of Pharmacology and Experimental Therapeutics, Apr. 1990, vol. 253, No. 1, pp. 13–19. US 2003/00968.05 A1 May 22, 2003 Gerner, P., et al., Anesthesiology (2002) 96:1435–42. Related U.S. Application Dat e pplication Uata Khan, M.A., et al., Anesthesiology (2002) 96:109–16. (63) stripps'965,138, filed on Sep. -
Food Additives Safety and Maximum Use Level
5/10/2017 FOOD ADDITIVES SAFETY & MAXIMUM USE LEVEL Nuri Andarwulan SEAFAST Center, IPB (Southeast Asian Food & Agr. Sci & Tech Center) Departemen Ilmu dan Teknologi Pangan, IPB [email protected] Outline Food additives Chemicals HOW are food additives regulated? Maximum use level of food additive [email protected] 1 5/10/2017 Food Additive is a substance (intentionally) added to food to alter the properties and/or the appearance of the food [email protected] As described by Paracelsus nearly 500 years ago, “All substances are poisons; there is none which is not a poison. The right dose differentiates a poison and a remedy”. This means that any chemical substance is likely to produce some form(s) of harmful effect, if taken in sufficient quantity. More addition of a chemical in food does not itself make food unsafe, but the quantity used in food, quantity of that food consumed and bodyweight will decide the safety. [email protected] 2 5/10/2017 The Codex definition of hazard is “a biological, chemical or physical agent with the potential to cause an adverse health effect”. The likelihood or risk of that hazard actually occurring in humans is dependent upon the quantity of chemical encountered or taken into the body, i.e. the exposure. [email protected] WHY do we need to regulate food additives? These chemicals may be harmful to your health (if consumed above the safety margin level) Benford, D. 2000, ILSI Europe [email protected] 3 5/10/2017 Food Additive (Codex Stan 192-1995) • Any substance not normally consumed as a food by itself and not normally used as a typical ingredient of the food, whether or not it has nutritive value, the intentional addition of which to food for a technological (including organoleptic) purpose in the manufacture, processing, preparation, treatment, packing, packaging and transport. -

Curriculum Vitae: Daniel J
CURRICULUM VITAE: DANIEL J. WALLACE, M.D., F.A.C.P., M.A.C.R. Up to date as of January 1, 2019 Personal: Address: 8750 Wilshire Blvd, Suite 350 Beverly Hills, CA 90211 Phone: (310) 652-0010 FAX: (310) 360-6219 E mail: [email protected] Education: University of Southern California, 2/67-6/70, BA Medicine, 1971. University of Southern California, 9/70-6/74, M.D, 1974. Postgraduate Training: 7/74-6/75 Medical Intern, Rhode Island (Brown University) Hospital, Providence, RI. 7/75-6/77 Medical Resident, Cedars-Sinai Medical Center, Los Angeles, CA. 7/77-6/79 Rheumatology Fellow, UCLA School of Medicine, Los Angeles, CA. Medical Boards and Licensure: Diplomate, National Board of Medical Examiners, 1975. Board Certified, American Board of Internal Medicine, 1978. Board Certified, Rheumatology subspecialty, 1982. California License: #G-30533. Present Appointments: Medical Director, Wallace Rheumatic Study Center Attune Health Affiliate, Beverly Hills, CA 90211 Attending Physician, Cedars-Sinai Medical Center, Los Angeles, 1979- Clinical Professor of Medicine, David Geffen School of Medicine at UCLA, 1995- Professor of Medicine, Cedars-Sinai Medical Center, 2012- Expert Reviewer, Medical Board of California, 2007- Associate Director, Rheumatology Fellowship Program, Cedars-Sinai Medical Center, 2010- Board of Governors, Cedars-Sinai Medical Center, 2016- Member, Medical Policy Committee, United Rheumatology, 2017- Honorary Appointments: Fellow, American College of Physicians (FACP) Fellow, American College of Rheumatology (FACR) -

Testosterone, Myocardial Function, and Mortality
Heart Failure Reviews https://doi.org/10.1007/s10741-018-9721-0 Testosterone, myocardial function, and mortality Vittorio Emanuele Bianchi1 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract The cardiovascular system is particularly sensitive to androgens, but some controversies exist regarding the effect of testosterone on the heart. While among anabolic abusers, cases of sudden cardiac death have been described, recently it was reported that low serum level of testosterone was correlated with increased risk of cardiovascular diseases (CVD) and mortality rate. This review aims to evaluate the effect of testosterone on myocardial tissue function, coronary artery disease (CAD), and death. Low testosterone level is associated with increased incidence of CAD and mortality. Testosterone administration in hypogonadal elderly men and women has a positive effect on cardiovascular function and improved clinical outcomes and survival time. Although at supraphysiologic doses, androgen may have a toxic effect, and at physiological levels, testosterone is safe and exerts a beneficial effect on myocardial function including mechanisms at cellular and mitochondrial level. The interaction with free testosterone and estradiol should be considered. Further studies are necessary to better understand the interaction mechanisms for an optimal androgen therapy in CVD. Keywords Testosterone . Coronary artery disease . Heart failure . Cardiovascular disease . Cardiomyocytes . Cardiac mitochondria . Cardiovascular mortality Introduction essential role [20]. Asymptomatic hypogonadism is observed in men 30–79 years old with an incidence of about 5.6% [21] The effects of testosterone on myocardial function have gen- and is more relevant in aging subjects. In recent years, pre- erated a great deal of discussion in the literature but remain scriptions for testosterone replacement therapy have increased controversial. -

Ruthenium Tetroxide (Ruo4) Oxidation of N-Alkyllactams Proceeded Regioselectively Depend- Ing on the Size of Lactam Ring, Except for the Seven-Membered Ring
No. 1 357 Chem. Pharm. Bull. 35(1) 357-363 (1987) Ruthenium Tetroxide Oxidation of N-Alkyllactams SHIGEYUKIYOSHIFUJI,* YUKIMI ARAKAWA, and YOSHIHIRONITTA Schoolof Pharmacy,Hokuriku University,Kanagawa-machi, Kanazawa920-11, Japan (ReceivedJuly 31, 1986) Ruthenium tetroxide (RuO4) oxidation of N-alkyllactams proceeded regioselectively depend- ing on the size of lactam ring, except for the seven-membered ring. Four- and eight-membered N- methyl- and N-ethyllactams were oxidized at the exocyclic ƒ¿-carbon adjacent to nitrogen to produce the N-acyllactams and NH-lactams, while five- and six-membered lactams underwent endocyclic oxidation to yield the cyclic imides. Oxidation of seven-membered lactams yielded a mixture of products arising from both exocyclic and endocyclic oxidations. These regioselectivities were confirmed in the oxidation of substrates having a tertiary carbon at the oxidation position. Keywords•\oxidation; ruthenium tetroxide oxidation; regioselective oxidation; hydroxyl- ation; imide synthesis; N-alkyllactam; N-acyllactam; imide; ruthenium tetroxide; two-phase method Ruthenium tetroxide (RuO4) is a good reagent for the conversion of N-acylated cyclic amines to the corresponding lactams,1) by oxidation of one of two carbons adjacent to nitrogen. As a common feature of the RuO4 oxidation in this conversion (la to 2 in Chart 1) and in the transformation of cyclic ethers into the corresponding lactones,2) it has been considered that RuO4 predominantly oxidizes a secondary carbon rather than a tertiary one. However, as reported previously,3) we obtained an opposite result in the RuO4 oxidation of some 1-azabicycloalkan-2-ones, such as quinolizidin-4-one (1b), which gave the hydroxylated products, such as 3, resulting from the oxidation of the tertiary carbon. -

61Ni Synchrotron-Radiation-Based Mössbauer Absorption
Hyperfine Interact (2018) 239:11 https://doi.org/10.1007/s10751-018-1488-0 61Ni synchrotron-radiation-based Mossbauer¨ absorption spectroscopy of Ni nanoparticle composites Ryo Masuda1 · Hirokazu Kobayashi2,3 · Yoshimasa Aoyama2 · Makina Saito1 · Shinji Kitao1 · Hiroki Ishibashi1 · Shuichi Hosokawa1 · Takaya Mitsui4 · Yoshitaka Yoda5 · Hiroshi Kitagawa2 · Makoto Seto1,4 © Springer International Publishing AG, part of Springer Nature 2018 Abstract We obtained energy-domain 61Ni synchrotron-radiation-based Mossbauer¨ absorption spectra of three materials that relate to nanoparticles: Ni2(C8O6H2) metal- organic frameworks (MOFs), Ni nanoparticles synthesized by complete heat decomposition of the MOFs, and the composites of Ni nanoparticles and the MOFs synthesized by par- tial decomposition of the MOFs. The 61Ni abundance of all the samples was not enriched but we were successfully able to obtain their spectra in 1 day or less, by using a highly efficient measurement system where the internal conversion electrons from energy standard 61 Ni86V14 foil were detected. Although both nanoparticle constituent and MOF constituent in the composites included Ni atoms, the Mossbauer¨ parameters of the Ni nanoparticle con- stituent could be evaluated; the magnetic hyperfine field of the Ni nanoparticle constituent in the composites was different from that of the Ni nanoparticles obtained by the complete heat decomposition. This difference implied that the 3d and/or 4s electron configuration of the nanoparticle constituent were affected by the MOF constituent -

And Tipt-Based High-Temperature Shape Memory Alloys: a Review on Recent Advances
metals Review TiPd- and TiPt-Based High-Temperature Shape Memory Alloys: A Review on Recent Advances Yoko Yamabe-Mitarai 1,2 1 Department of Advanced Materials Science, Graduate School of Frontier Sciences, The University of Tokyo, 5-1-5 Kashiwanoha, Kashiwa-shi, Chiba 277-8561, Japan; [email protected] 2 National Institute for Materials Science, 1-2-1 Sengen, Tsukuba, Ibaraki 305-0047, Japan Received: 30 September 2020; Accepted: 12 November 2020; Published: 18 November 2020 Abstract: In this paper high-temperature shape memory alloys based on TiPd and TiPt are reviewed. The effect of the alloying elements in ternary TiPd and TiPt alloys on phase transformation and strain recovery is also discussed. Generally, the addition of alloying elements decreases the martensitic transformation temperature and improves the strength of the martensite and austenite phases. Additionally, it also decreases irrecoverable strain, but without perfect recovery due to plastic deformation. With the aim to improve the strength of high-temperature shape memory alloys, multi-component alloys, including medium- and high-entropy alloys, have been investigated and proposed as new structural materials. Notably, it was discovered that the martensitic transformation temperature could be controlled through a combination of the constituent elements and alloys with high austenite finish temperatures above 500 ◦C. The irrecoverable strain decreased in the multi-component alloys compared with the ternary alloys. The repeated thermal cyclic test was effective toward obtaining perfect strain recoveries in multi-component alloys, which could be good candidates for high-temperature shape memory alloys. Keywords: high-temperature shape memory alloys; titanium palladium; titanium platinum; multi-component alloys; medium-entropy alloys; high-entropy alloys 1. -

Ec:Rbfc/2010/3
EC:RBFC/2010/3 Food and Agriculture Organization of the United Nations JOINT FAO/WHO EXPERT CONSULTATION ON THE RISKS AND BENEFITS OF FISH CONSUMPTION Rome, Italy, 25 - 29 January 2010 HEALTH RISKS ASSOCIATED WITH FISH CONSUMPTION FOCUS ON METHYLMERCURY, DIOXINS AND DIOXIN-LIKE PCBS Lucio G. Costa Professor, Department of Occupational and Health Sciences University of Washington, Seattle, USA & Vittorio Fattori Nutrition and Consumer Protection Division, FAO, Rome, Italy 2 EC:RBFC/2010/3 TABLE OF CONTENTS 1 INTRODUCTION ......................................................................................... 4 1.1 Objective and Scope of the paper ................................................................ 4 2 CONTAMINANTS IN FISH ........................................................................... 4 3 INTERNATIONAL ADVISORIES ................................................................... 6 3.1 Mercury ....................................................................................................... 6 4 MERCURY ................................................................................................... 8 4.1 Mercury in the environment ....................................................................... 8 4.1.1 The environmental cycle of mercury ............................................................................ 8 4.1.2 Main sources of mercury release into environment ..................................................... 9 4.1.3 Main food sources ....................................................................................................... -

The Acceptable Daily Intake (ADI)
Appendix 1- Definitions and glossary of terms Acceptable Daily Intake (ADI) The Acceptable Daily Intake (ADI) for humans is defined as an estimate of the amount of a chemical that can be ingested daily over a lifetime without appreciable risk to health (WHO 2001). ADIs are set using information obtained from toxicological studies, including data from studies on various laboratory animals. From these studies, a No Observable Effect Level (NOEL) is established. The NOEL is the highest dose level that produces no observable toxic effect in the most sensitive test species and is expressed in milligrams per kilogram of body weight per day (mg/kg bw/day). The ADI is derived by applying a safety factor to the NOEL. The safety factor takes into consideration the nature of the effect, differences between laboratory test animals and humans, and genetic variation in the human population. If any information on exposure in humans is available, usually from short to mid-term studies, this will be used to set the ADI. The unit for the ADI is milligrams per kilogram of body weight per day. Limit of Detection (LOD) The LOD is the lowest concentration of a chemical that can be qualitatively detected using a specified laboratory method and/or item of laboratory equipment (i.e. its presence can be detected but not quantified). For the purposes of this study, analytical results reported as being less than the LOD were assumed to be zero. Limit of Quantification (LOQ) The LOQ is the lowest concentration of a chemical that can be detected and quantified, with an acceptable degree of certainty, using a specified laboratory method and/or item of laboratory equipment. -

An Aspect of Nutrition and Main Food Sweeteners in the Diet
Advances in Obesity, Weight Management & Control Review Article Open Access An aspect of nutrition and main food sweeteners in the diet Abstract Volume 11 Issue 2 - 2021 Food additives are factors in both health reason and food production. Sweeteners are utilized Necla Çağlarırmak in large scale because of biochemistry, production, obesity, food structure, economy, Food Proses Department, Manisa Celal Bayar University, Turkey functional property, and research and development efforts of food industry. Intake of high calorie nutrients such as sugar in the nutrition are important factors against increasing Correspondence: Necla Çağlarırmak, Food Proses trends of obesity, cardiovascular disease and diabetes and some of chronic diseases. In Department, Manisa Celal Bayar University, Saruhanlı College, healthy nutrition, the sufficient calorie intake must be recommended for basal metabolism Saruhanlı-Manisa, Turkey, Email [email protected] and usual daily activities due to individual and environment conditions. Sweeteners are also food additives and using commonly for low calorie nutrition or from other reasons such as Received: April 01, 2021 | Published: April 12, 2021 bulk of foods. natural sweeteners can be suggested such as stevia, together with balanced and low calorie diet including vegetables, and other food types due to diet originality that change in different societies, economies, regions and education levels of people. Traditional nutrition such as Mediterranean diet can be recommended for balanced diet. This topic was reviewed under light of literature. Keywords: biochemistry, foods, JEFCA, sweeteners, obesity, nutrition, food formulas, side effects, health Abbreviations: SSBs, sugar-sweetened beverages; Ace-K, World. Nobody does not forget almost one billion people in border acesulfame potassium; ADI, adequate dietary intake of starvation or suffering the famine against obesity.2 There are lots of factors affected nutrition including economies and development Introduction strategies in the World. -
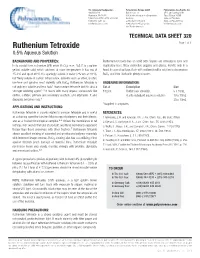
Ruthenium Tetroxide Page 1 of 1 0.5% Aqueous Solution
U.S. Corporate Headquarters Polysciences Europe GmbH Polysciences Asia-Pacific, Inc. 400 Valley Rd. Badener Str. 13 2F-1, 207 Dunhua N. Rd. Warrington, PA 18976 69496 Hirschberg an der Bergstrasse Taipei, Taiwan 10595 1(800) 523-2575 / (215) 343-6484 Germany (886) 2 8712 0600 1(800)343-3291 fax +(49) 06201 845 20 0 (886) 2 8712 2677 fax [email protected] +(49) 06201 845 20 20 fax [email protected] [email protected] TECHNICAL DATA SHEET 320 Ruthenium Tetroxide Page 1 of 1 0.5% Aqueous Solution BACKGROUND AND PROPERTIES: Ruthenium tetroxide has an acrid odor. Vapors are irritating to eyes and In its crystal form, ruthenium (VIII) oxide (RuO4), m.w. 165.7, is a golden respiratory tract. Wear protective goggles and gloves. Handle only in a yellow, volatile solid which sublimes at room temperature. It has mp of hood. In case of spillage, flush with sodium bisulfite solution to decompose 25.4°C and bp of 40°C. It is sparingly soluble in water (2% w/v at 20°C), RuO4 and then flush with plenty of water. but freely soluble in carbon tetrachloride. Solvents such as ether, alcohol, benzene and pyridine react violently with RuO4. Ruthenium tetroxide is ORDERING INFORMATION: not only less volatile and less toxic1 than osmium tetroxide but it is also a Cat. # Description Size stronger oxidizing agent.1-3 It reacts with many organic compounds like 18253 Ruthenium tetroxide, 5 x 10mL olefins, sulfides, primary and secondary alcohols, and aldehydes. It also 0.5% stabalized aqueous solution 10 x 10mL degrades benzene rings.3 25 x 10mL *Supplied in ampoules APPLICATIONS AND INSTRUCTIONS: Ruthenium tetroxide is closely related to osmium tetroxide and is useful REFERENCES: as a staining agent for Electron Microscopy of polymers and their blends, 1. -

Glyphosate: Unsafe on Any Plate
GLYPHOSATE: UNSAFE ON ANY PLATE ALARMING LEVELS OF MONSANTO’S GLYPHOSATE FOUND IN POPULAR AMERICAN FOODS “For the first time in the history of the world, every human being is now subjected to contact with dangerous chemicals from the moment of conception until death…These chemicals are now stored in the bodies of the vast majority of human beings, regardless of age. They occur in the mother’s milk, and probably in the tissues of the unborn child.”1 —RACHEL CARSON, SILENT SPRING “Glyphosate was significantly higher in humans [fed] conventional [food] compared with predominantly organic [fed] humans. Also the glyphosate residues in urine were grouped according to the human health status. Chronically ill humans had significantly higher glyphosate residues in urine than healthy humans”2 —MONIKA KRUGER, ENVIRONMENTAL & ANALYTICAL TOXICOLOGY “Analysis of individual tissues demonstrated that bone contained the highest concentration of [14C] glyphosate equivalents (0.3–31ppm). The remaining tissues contained glyphosate equivalents at a concentration of between 0.0003 and 11 ppm. In the bone and some highly perfused tissues, levels were statistically higher in males than in females.”3 —PESTICIDE RESIDUES IN FOOD, JOINT FAO/WHO MEETING 2004 1 Rachel Carson, Silent Spring, (Houghton Mifflin, 1961), Elixirs of Death, 15-16. 2 Krüger M, Schledorn P, Schrödl W, Hoppe HW, Lutz W, et al. (2014) Detection of Glyphosate Residues in Animals and Humans. J Environ Anal Toxicol 4: 210 3 Residues in Food, 2004, Evaluations Part II, Toxicological, Joint FAO/WHO Meeting on Pesticide Residues. http://apps.who.int/iris/ bitstream/10665/43624/1/9241665203_eng.pdf Contents What Is in This Report? Findings: The first ever independent, FDA-registered laboratory food testing results for glyphosate residues in iconic American food brands finds alarming levels of glyphosate contamination and reveal the inadequacy of current food safety regulations relating to allowable pesticide residues.