Monitoring Visit Report –Andhra Pradesh Quarter 4, 2012- 2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LHA Recuritment Visakhapatnam Centre Screening Test Adhrapradesh Candidates at Mudasarlova Park Main Gate,Visakhapatnam.Contact No
LHA Recuritment Visakhapatnam centre Screening test Adhrapradesh Candidates at Mudasarlova Park main gate,Visakhapatnam.Contact No. 0891-2733140 Date No. Of Candidates S. Nos. 12/22/2014 1300 0001-1300 12/23/2014 1300 1301-2600 12/24/2014 1299 2601-3899 12/26/2014 1300 3900-5199 12/27/2014 1200 5200-6399 12/28/2014 1200 6400-7599 12/29/2014 1200 7600-8799 12/30/2014 1177 8800-9977 Total 9977 FROM CANDIDATES / EMPLOYMENT OFFICES GUNTUR REGISTRATION NO. CASTE GENDER CANDIDATE NAME FATHER/ S. No. Roll Nos ADDRESS D.O.B HUSBAND NAME PRIORITY & P.H V.VENKATA MUNEESWARA SUREPALLI P.O MALE RAO 1 1 S/O ERESWARA RAO BHATTIPROLU BC-B MANDALAM, GUNTUR 14.01.1985 SHAIK BAHSA D.NO.1-8-48 MALE 2 2 S/O HUSSIAN SANTHA BAZAR BC-B CHILAKURI PETA ,GUNTUR 8/18/1985 K.NAGARAJU D.NO.7-2-12/1 MALE 3 3 S/O VENKATESWARULU GANGANAMMAPETA BC-A TENALI. 4/21/1985 SHAIK AKBAR BASHA D.NO.15-5-1/5 MALE 4 4 S/O MAHABOOB SUBHANI PANASATHOTA BC-E NARASARAO PETA 8/30/1984 S.VENUGOPAL H.NO.2-34 MALE 5 5 S/O S.UMAMAHESWARA RAO PETERU P.O BC-B REPALLI MANDALAM 7/20/1984 B.N.SAIDULU PULIPADU MALE 6 6 S/O PUNNAIAH GURAJALA MANDLAM ,GUNTUR BC-A 6/11/1985 G.RAMESH BABU BHOGASWARA PET MALE 7 7 S/O SIVANJANEYULU BATTIPROLU MANDLAM, GUNTUR BC-A 8/15/1984 K.NAGARAJENDRA KUMAR PAMIDIMARRU POST MALE 8 8 S/O. -
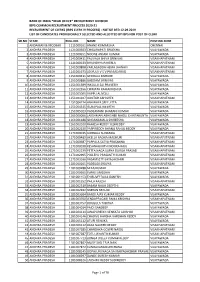
Clerks (Ibps Clerk Ix Process) - Notice Dtd 12.09.2019 List of Candidates Provisionally Selected and Allotted by Ibps for Post of Clerk
BANK OF INDIA *HEAD OFFICE* RECRUITMENT DIVISION IBPS COMMON RECRUITMENT PROCESS 2020-21 RECRUITMENT OF CLERKS (IBPS CLERK IX PROCESS) - NOTICE DTD 12.09.2019 LIST OF CANDIDATES PROVISIONALLY SELECTED AND ALLOTTED BY IBPS FOR POST OF CLERK SR.NO STATE ROLL.NO. NAME POSTING ZONE 1 ANDAMAN & NICOBAR 1111000161 ANAND KUMAR JHA CHENNAI 2 ANDHRA PRADESH 1121000303 CHIGURUPATI SRILEKHA VIJAYAWADA 3 ANDHRA PRADESH 1121000651 NOONE ANJANI KUMAR VIJAYAWADA 4 ANDHRA PRADESH 1141000411 PALIVALA SHIVA SRINIVAS VISAKHAPATNAM 5 ANDHRA PRADESH 1141000633 BHAVISHYA PAKERLA VISAKHAPATNAM 6 ANDHRA PRADESH 1141000808 YARLAGADDA HEMA JAHNAVI VISAKHAPATNAM 7 ANDHRA PRADESH 1141001673 JOSYULA V S V PRASADARAO VISAKHAPATNAM 8 ANDHRA PRADESH 1151000411 GEDDALA KISHORE VIJAYAWADA 9 ANDHRA PRADESH 1151000886 GADDAM SRINIVAS VIJAYAWADA 10 ANDHRA PRADESH 1151001389 INKOLLU SAI PRAVEEN VIJAYAWADA 11 ANDHRA PRADESH 1151002556 CHIMATA RAMAKRISHNA VIJAYAWADA 12 ANDHRA PRADESH 1151003005 VUPPU ALIVELU VIJAYAWADA 13 ANDHRA PRADESH 1151004107 GUNTUR ABHISHEK VISAKHAPATNAM 14 ANDHRA PRADESH 1151004274 ABHINAYA SREE JITTA VIJAYAWADA 15 ANDHRA PRADESH 1151004515 ISUKAPALLI KEERTHI VIJAYAWADA 16 ANDHRA PRADESH 1151005023 VADLAMANI BHARANI KUMAR VIJAYAWADA 17 ANDHRA PRADESH 1161000066 LAKSHMAN ABHISHEK NAIDU CHINTAKUNTA VIJAYAWADA 18 ANDHRA PRADESH 1161001188 SINGANAMALA SHIREESHA VIJAYAWADA 19 ANDHRA PRADESH 1161002020 RAMESH REDDY YESIREDDY VIJAYAWADA 20 ANDHRA PRADESH 1161002630 PAPPIREDDY BHANU RAHUL REDDY VIJAYAWADA 21 ANDHRA PRADESH 1171000015 GUBBALA SUNANDA VISAKHAPATNAM -
Chapter Ii Vizianagaram
CHAPTER II VIZIANAGARAM - THE LOCAL ENVIRONMENT 33 VIZIANAGARAM - THE LOCAL ENVIRONMENT Vizianagaram is situated half way between Calcutta and Madras, 507 miles from Calcutta and 522 from Madras. It was in the Vizagapatam District of the then Madras state with an area of more than 18,000 square miles and a population of 2,610,000.' Vizianagaram is situated in latitude 18°.2" North, and longitude 83° 32" east; at twelve miles distance from the sea. The garrison at this time consists of one Regiment of Native Infantry. At the distance of one mile from the cantonment, which is placed on ground sloping gently to the northward, are the fort and town, and laying midway is a large tank (Pedda Cheruvu), which contains water at all seasons of the year. The fort is entirely occupied by the palace and buildings of the Maharaja. The station contains about twenty officers' houses; the compounds are very prettily laid out with gardens, and surrounded with trim hedges. There is a small church; a chaplain is allowed for the station, but he is required to visit Bhimlipatam and Chicacole, two Sundays each month.^ Climate: Generally the climate of the time is nonnal, without extreme atmospheric variations. But at some seasons in an year, especially in the wintry months it is a bit less. To the north of the town there are hills and hillocks at a distance of about six miles that connect the Eastern Ghats. There 34 are few patches of shrub jungles nearby. The best season with average climate IS from September to March, Summer sets in April when the weather becomes hot and the hot winds commence blowing from the middle of the month. -

One God, Two Goddesses, Three Studies of South Indian Cosmology Jerusalem Studies in Religion and Culture
One God, Two Goddesses, Three Studies of South Indian Cosmology Jerusalem Studies in Religion and Culture Editors Guy Stroumsa David Shulman Hebrew University of Jerusalem Department of Comparative Religion VOLUME 18 The titles published in this series are listed at brill.com/jsrc One God, Two Goddesses, Three Studies of South Indian Cosmology by Don Handelman LEIDEn • bOSTON 2014 Library of Congress Cataloging-in-Publication Data Handelman, Don. One god, two goddesses, three studies of South Indian cosmology / by Don Handelman. pages cm. — (Jerusalem studies in religion and culture, ISSN 1570-078X ; volume 18) Includes bibliographical references and index. ISBN 978-90-04-25615-6 (hardback : alk. paper) — ISBN 978-90-04-25739-9 (e-book : alk. paper) 1. Hinduism—India, South—Rituals. 2. Murugan (Hindu deity)—Cult. 3. Hindu goddesses— India, South. 4. Hindu cosmology. I. Title. BL1226.2.H36 2013 294.5’211—dc23 2013026797 This publication has been typeset in the multilingual “Brill” typeface. With over 5,100 characters covering Latin, IPA, Greek, and Cyrillic, this typeface is especially suitable for use in the humanities. For more information, please see www.brill.com/brill-typeface. ISSN 1570-078x ISBN 978-90-04-25615-6 (hardback) ISBN 978-90-04-25739-9 (e-book) Copyright 2014 by Koninklijke Brill NV, Leiden, The Netherlands. Koninklijke Brill NV incorporates the imprints Brill, Global Oriental, Hotei Publishing, IDC Publishers and Martinus Nijhoff Publishers. All rights reserved. No part of this publication may be reproduced, translated, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without prior written permission from the publisher. -

CBI Books 17 for Derogatory Remarks on SC, HC Judges
Follow us on: RNI No. APENG/2018/764698 @TheDailyPioneer facebook.com/dailypioneer Established 1864 Published From ANALYSIS 7 MONEY 8 SPORTS 11 VIJAYAWADA DELHI LUCKNOW NIX PRIORITY COVID HALTS SHOPPING MALL SMITH, WARNER'S PRESENCE BHOPAL RAIPUR CHANDIGARH SECTOR LENDING LAUNCHES ACROSS COUNTRY A CHALLENGE: PUJARA BHUBANESWAR RANCHI DEHRADUN HYDERABAD *Late City Vol. 3 Issue 11 VIJAYAWADA, TUESDAY NOVEMBER 17, 2020; PAGES 12 `3 *Air Surcharge Extra if Applicable AFTER A HOCKEY PLAYER, SUNDEEP TO PLAY A ROWDY NEXT { Page 12 } www.dailypioneer.com TODAY BJP man in a soup ALMANAC CBI books 17 for derogatory Month & Paksham: Kartik & Shukla Paksha for Godse tweet Panchangam PNS n VIJAYAWADA Tithi : Tritiya: 01:16 am (Next Day) Nakshatram: Jyeshtha: 12:21 pm remarks on SC, HC judges BJP state secretary Ramesh Time to Avoid: (Bad time to start SUMIT ONKA CBI’s Anti-Corruption Bureau Naidu Nagothu was on Panabaka is any important work) n VISAKHAPATNAM SC judge recuses from hearing pleas against CM (Vizag) based on the informa- Monday forced to retract his tion furnished by CID. tweet praising Gandhi’s assas- Rahukalam: 02:48 pm – 04:12 pm New Delhi: Supreme Court judge parties. I will pass an order for it Naidu pick for The CBI on Monday filed 12 UU Lalit on Monday recused to be listed before a Bench Two persons believed to be sin Nathuram Godse on Yamagandam: 09:13 am – 10:37 am cases against 17 persons, some himself from hearing pleas without me," Justice Lalit staying abroad are also in the Sunday following a severe Tirupati bypoll Varjyam: 07:47 pm – 09:16 pm, known and others unknown, seeking action against said. -

Investor First Name Investor Middle Name Investor Last Name Father
Investor First Name Investor Middle Name Investor Last Name Father/Husband First Name Father/Husband Middle Name Father/Husband Last Name Address Country State District Pin Code Folio No. DP.ID-CL.ID. Account No. Invest Type Amount Transferred Proposed Date of Transfer to IEPF PAN Number Aadhar Number 74/153 GANDHI NAGAR A ARULMOZHI NA INDIA Tamil Nadu 636102 IN301774-10480786-0000 Amount for unclaimed and unpaid dividend 160.00 15-Sep-2019 ATTUR 1/26, VALLAL SEETHAKATHI SALAI A CHELLAPPA NA KILAKARAI (PO), INDIA Tamil Nadu 623517 12010900-00960311-TE00 Amount for unclaimed and unpaid dividend 60.00 15-Sep-2019 RAMANATHAPURAM KILAKARAI OLD NO E 109 NEW NO D A IRUDAYAM NA 6 DALMIA COLONY INDIA Tamil Nadu 621651 IN301637-40636357-0000 Amount for unclaimed and unpaid dividend 20.00 15-Sep-2019 KALAKUDI VIA LALGUDI OPP ANANDA PRINTERS I A J RAMACHANDRA JAYARAMACHAR STAGE DEVRAJ URS INDIA Karnataka 577201 IN300360-10245686-0000 Amount for unclaimed and unpaid dividend 8.00 15-Sep-2019 ACNPR4902M NAGAR SHIMOGA NEW NO.12 3RD CROSS STREET VADIVEL NAGAR A J VIJAYAKUMAR NA INDIA Tamil Nadu 632001 12010600-01683966-TE00 Amount for unclaimed and unpaid dividend 100.00 15-Sep-2019 SANKARAN PALAYAM VELLORE THIRUMANGALAM A M NIZAR NA OZHUKUPARAKKAL P O INDIA Kerala 691533 12023900-00295421-TE00 Amount for unclaimed and unpaid dividend 20.00 15-Sep-2019 AYUR AYUR FLAT - 503 SAI DATTA A MALLIKARJUNAPPA ANAGABHUSHANAPPA TOWERS RAMNAGAR INDIA Andhra Pradesh 515001 IN302863-10200863-0000 Amount for unclaimed and unpaid dividend 80.00 15-Sep-2019 AGYPA3274E -

Dj15052015rcell.Pdf
HIGH COURT OF JUDICATURE AT HYDERABAD FOR THE STATE OF TELANGANA AND THE STATE OF ANDHRA PRADESH STATEMENT SHOWING THE LIST OF ELIGIBLE CANDIDATES WHO ARE APPLIED FOR THE 6 POSTS OF DISTRICT JUDGE UNDER DIRECT RECRUITMENT, NOTIFIED FOR THE YEAR 2014 SL Appl. NAME OF THE APPLICANT No. No.. ADDRESS 1. Venkata Narasimha Raju Krovvidi Plot No.44, Port Colony, 1 Back side of Nookambica Temple, Kasimkota Mandal, Kasimkota, Visakhapatnam District 531031 2. Suhasini Makina Dr.No.63-3-22/5, Flat No.202, 2 Dwarakamani Residence, Jawahar Nagar, Sriharipuram, Visakhapatnam 530011 3. Fareed Khan 3 4-10-6/1, Rajampet, Sanga Reddy Town, Medak District. 502001 4. Tejovathi Machisrajau Flot No.401, 4th Floor, 4 1-2-607/23/1/D, Om Nagar, Indira Park Road, Ashok Nagar, Hyderabad. 500080 5. Venkata Ratnakar Kondiparthi D.No.18-10-34, Zero Lane, 5 Kedareswarapet, Vijayawada, Krishna District 520003 6. Taruna Kumar Pillalamarri Door No.21-14-12-20/2A, Thota Vari 6 Street, 2nd Line, Ramalingeswarapet, Tenali, Guntur District. 522201 7. 7 Chandra Mohan Karumuru D.No.60-97-1, Nabikota, R.V.Nagar Post, Kadapa City and District 516003 8. Kasi Viswanadha Raju Alakunta 8 Dr.No.27-3-2, Rweddys Bazar, Near B.C. Colony, Burripalem Road, Tenali, Guntur District 522201 9. Subbalakshmi Nimmakayala C/o. V.Purushothama Rao, 10 Ramakrishna Homeo Hospita D.No.5-3-58, Konddappa Street, Pithapuram, East Godavari District 533450 10. Sreenivasulu Chennaiah Gari 11 H.No.87-1066, Ganesh Nagar-I, Kurnool Post, Kurnool Distrtict. 518002 11. Venkateshwarlu Vinjamuri H.No.8-2-338/1, Panchavati Co-Op 12 HSG Society, Road No3, Banjara Hills, Hyderabad. -

State District Branch Address Centre Ifsc
STATE DISTRICT BRANCH ADDRESS CENTRE IFSC CONTACT1 CONTACT2 CONTACT3 MICR_CODE A.N.REDDY NAGAR ANDHRA A N REDDY BR,NIRMAL,ANDHRA PRADESH ADILABAD NAGAR PRADESH NIRMAL ANDB0001972 8734243159 NONMICR 3-2-29/18D, 1ST CH.NAGAB FLOOR, AMBEDKAR HUSHANA ANDHRA CHOWK ADILABAD - M 08732- PRADESH ADILABAD ADILABAD 504 001 ADILABAD ANDB0000022 230766 TARA COMPLEX,MAIN ANDHRA ROAD,ASIFABAD,ADI 08733 PRADESH ADILABAD ASIFABAD LABAD DT - 504293 ASIFABAD ANDB0002010 279211 504011293 TEMPLE STREET, BASARA ADILABAD, ANDHRA ADILABAD, ANDHRA 986613998 PRADESH ADILABAD BASARA PRADESH-504104 BASAR ANDB0001485 1 Bazar Area, Bellampally , Adilabad G.Jeevan Reddy ANDHRA Dist - - 08735- PRADESH ADILABAD Bellampalli Bellampalli ADILABAD ANDB0000068 504251 2222115 ANDHRA BANK, BHAINSA BASAR P.SATYAN ROAD BHAINSA- ARAYANA - ANDHRA 504103 ADILABAD 08752- PRADESH ADILABAD BHAINSA DIST BHAINSA ANDB0000067 231108 D.NO 4-113/3/2,GOVT JUNIOR COLLEGE ROAD,NEAR BUS ANDHRA STAND,BOATH - 949452190 PRADESH ADILABAD BOATH 504305 BOATH ANDB0002091 1 MAIN ROAD,CHENNUR, ADILABAD DIST, ANDHRA CHENNUR, ANDHRA 087372412 PRADESH ADILABAD CHENNUR PRADESH-504201 CHINNOR ANDB0000098 36 9-25/1 BESIDE TANISHA GARDENS, ANDHRA DASNAPUR, PRADESH ADILABAD DASNAPUR ADILABAD - 504001 ADILABAD ANDB0001971 NO NONMICR ORIENT CEMENT WORKS CO, DEVAPUR,ADILABAD DIST, DEVAPUR, ANDHRA ANDHRA PRADESH- 08736 PRADESH ADILABAD DEVAPUR 504218 DEVAPUR ANDB0000135 240531 DOWEDPALLI, LXXETTIPET 08739- ANDHRA VILLAGE, GANDHI DOWDEPAL 233666/238 PRADESH ADILABAD DOWDEPALLI CHOWK LI ANDB0000767 222 H NO 1-171 VILL -

Appendixes Appendix 1 on Mackenzie’S Historical Enquiries: a Memorandum
Appendixes Appendix 1 On Mackenzie’s Historical Enquiries: A Memorandum. Madras—Feb. 14th, 1808. Major Mackenzie has for some time past/ thro’ the good offices of his Friends/ Collected various Materials, that are supposed to con- vey considerable information, on the Ancient History, State, and Institutions of the South of India, but he finds Several parts are still doubtful; which he believes might be yet illustrated by materials of various descriptions, in the hands of the Natives, and which from their obscurity are liable to be neglected and lost; but might be still recovered by the interposition of the Gentlemen in the Diplomatic, Judicial, Revenue, and Medical Departments particularly—He has already derived much aid from the liberal Support of such as he has the honor to be acquainted with, and doubts not but others would be equally willing to forward a design presumed to be advantageous to the Cultivation of this branch of General knowledge, In the Southern Provinces he is desirous of obtaining Copies or Originals of any Native MS in any language; relating to the ancient Government, of the Pandeyan and Cholla Kings or other Dynasties, that have ruled in these Countries; several accounts are already obtained, but they are still defective, and it is supposed further con- siderable lights are procurable, At Madura and other ancient Religious Establishments some notices, it is supposed are still preserved in the hands of the Bramins, which may throw light on the Ancient Government, and Colonies that are supposed to have emigrated to the Western and Eastern parts of the Coast as appears by traces in these Provinces—Accounts are also said to be preserved of the Religious contentions, that took place between the Bramins, Jain and other Sects. -

Lok Sabha Secretariat
LOK SABHA SECRETARIAT Details of expenditure incurred on HS/HDS/LOP/MP(s)* During the Period From 01/03/2015 To 31/03/2015 Office Salary for Arrears(if SL ICNO Name of MP/ Salary Constituency Travelling/ Expense/ Available) State Allowance Secretarial daily Sumptury Assistant Allowence Allowance 160001 Shri Godam Nagesh 1 50000 45000 15000 30000 190237 0 Andhra Pradesh 160002 Shri Balka Suman 2 50000 45000 15000 30000 422160 0 Andhra Pradesh 160003 Shri Vinod kumar 3 50000 45000 15000 30000 149967 Boianapalli 0 Andhra Pradesh 160004 Smt. Kalvakuntla Kavitha 4 50000 45000 15000 30000 338803 0 Andhra Pradesh 160005 Shri Bheemrao 5 50000 45000 15000 30000 0 Baswanthrao Patil 0 Andhra Pradesh 160006 Shri Kotha Prabhakar 6 50000 45000 15000 30000 0 Reddy 0 Andhra Pradesh 160007 Ch.Malla Reddy 7 50000 45000 15000 30000 60049 0 Andhra Pradesh 160008 Shri Bandaru Dattatreya 8 0 0 0 0 0 0 Andhra Pradesh 160009 Shri Owaisi Asaduddin 9 50000 45000 15000 30000 380985 0 Andhra Pradesh 160010 Shri Konda Vishweshar 10 50000 45000 15000 30000 0 Reddy 0 Andhra Pradesh 160011 Shri A.P.Jithender Reddy 11 50000 45000 15000 30000 285003 0 Andhra Pradesh 160012 Shri Yellaiah Nandi 12 50000 45000 15000 30000 93142 0 Andhra Pradesh 160013 Shri Gutha Sukender 13 50000 45000 15000 30000 312448 Reddy 0 Andhra Pradesh 160014 Dr.Boora Narsaiah Goud 14 50000 45000 15000 30000 30400 0 Andhra Pradesh 160015 Shri Kadiyam Srihari 15 50000 45000 15000 30000 0 0 Andhra Pradesh 160016 Prof. Azmeera Seetaram 16 50000 45000 15000 30000 533922 Naik 0 Andhra Pradesh 160017 ShriPonguleti Srinivasa 17 50000 45000 15000 30000 329755 Reddy 0 Andhra Pradesh LOK SABHA SECRETARIAT Details of expenditure incurred on HS/HDS/LOP/MP(s)* During the Period From 01/03/2015 To 31/03/2015 Office Salary for Arrears(if SL ICNO Name of MP/ Salary Constituency Travelling/ Expense/ Available) State Allowance Secretarial daily Sumptury Assistant Allowence Allowance 160018 Smt. -

The Political Awakening and National Struggle in Nellore District
International Journal of Research in Humanities and Social Studies Volume 3, Issue 7, July 2016, PP 7-22 ISSN 2394-6288 (Print) & ISSN 2394-6296 (Online) The Political Awakening and National Struggle in Nellore District Dr.K.Sravana Kumar M.A.Ph.D. Lecturer in History, N.B.K.R. Science and Arts College, Vidya Nagar, Kota Mandal Nellore District, Andhra Pradesh, India ABSTRACT The Indian national movement was undoubtedly one of the biggest mass movements in modern society has ever seen. It was a movement which galvanised millions of people of all classes and ideologies into political action and brought to its knees a mighty colonial empire. Basically nationalism in India arose to meet the challenge of foreign domination. The very existence of a foreign rule helped the growth of national sentiment among the people. There was also a clash between the British interests in India and those of the Indian people. The British had conquered India to promote their own interests and they ruled over her primarily with that object in view. With the passage of time there was a realisation in India and that realization brought bitterness against foreign rule and that was responsible for the growth of the nationalist movement to drive out the foreigners from the country. The intelligentsia in India the peasants, the artisans and the workers all played their part in the freedom struggle. Keywords: the political awakening and national struggle nationalist movement. INTRODUCTION The nationalist movement in India was the outcome of a large number of factors and the most important among them was British imperialism which helped the process of the unification of the country. -

District Census Handbook, Vizianagaram, Part XIII a & B
CENSUS OF INDIA 1981 SERIES 2 ANDHRA PRADESH DISTRICT CENSUS HANDBOOK VIZIANAGARAM PARTS Xlfl-A & B VILLAGE & TOWN DIRECTORY VILLAGE & TOWNWISE PRIMARY CENSUS ABSTRACT S. S. JAYA RAD' OF THE INDIAN ADMINISTRATIVE SERVICE' DIRECTOR OF CENSUS OPERA nONS· ANDHRA PRADESH P1)IIL1SHBD BY THE GOVERNMENT OF ANDHRA PRADESH 198& The musical instruments depicted on the cover page as motif represent the greatness of the district Vizianagaram in the fields of music and culture. Vizianagaram is a place of historical importance and it attained great importance in the past as the centre of arts and culture under the patronage of the enlightened ruling family of Vizianagaram. It is one of the centres of cultural development in the State. Music is the foremost of the Fine Arts to transport man from his terrestrial surroundings and take him to realms of ecstasy. Perhaps that is the reason, why the Hindus honourerj the musical instruments by placing Veena in the hands of Saraswathi the goddess of learning. Mrudangam in the hands of Vishnu who is known to play it to synchronise with the dance of Lord Siva. Lord Krishna the divine teacher and preacher was a/so the famous flute player. Violin and Harmonium were also there to indicate the largeness of the Indian heart to welcome anything good from the foreign lands. The Veena manufactured in Bobbili of Vizianagaram district is famous throughout India. It is no wonder than that the first written book of the world, Ramayana, by Sage Valmik( was so composed that it could be played on a stringed instrument (~oL.\ odi> ;;)::»~~C;O).