Tef Jansma Master Thesis May 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Veilig Op De Fiets in Westerveld Een Inventarisatie Van De Verkeersveiligheid Voor Fietsers in De Gemeente Westerveld
Veilig op de fiets in Westerveld Een inventarisatie van de verkeersveiligheid voor fietsers in de gemeente Westerveld 2 Veilig op de fiets in Westerveld Een inventarisatie van de verkeersveiligheid voor fietsers in de gemeente Westerveld. Bart van Faassen September 2015 3 Inhoudsopgave 1. Waarom deze inventarisatie? ................................................................................................ 7 1.1 Iedereen neemt deel aan het verkeer ..................................................................................... 7 1.2 Verkeersveiligheid is verbeterd door Duurzaam Veilig Verkeer ............................................. 7 1.3 Toch stijgt het aantal ernstige fietsslachtoffers ...................................................................... 8 1.4 De fiets heeft vele voordelen .................................................................................................. 9 1.5 Opdracht tot lokale aanpak verbetering verkeersveiligheid ................................................... 9 1.6 Doelstelling notitie ................................................................................................................ 10 2. Wat speelt er in fietsland Nederland? .................................................................................. 11 2.1 Landelijk ................................................................................................................................. 11 2.1.1 Stijging aantal ernstige fietsongevallen ........................................................................ -

Lijn 20 Van Meppel Via Steenwijk En Dieverbrug Naar Assen Maandag T/M Vrijdag Normale Dienstregeling
Lijn 20 van Meppel via Steenwijk en Dieverbrug naar Assen maandag t/m vrijdag normale dienstregeling Ritnummer: 1 5 7 9 11 501 13 15 419 17 19 423 21 23 Station, Meppel V 06:21 07:17 08:19 09:16a 10:16a Burg. Knopperslaan, Meppel 06:22 07:18 08:20 09:17a 10:17a Hugo de Grootstraat, Meppel 06:23 07:19 08:21 09:18a 10:18a Steenwijkerstraatweg, Meppel 06:23 07:20 08:22 09:19a 10:19a Nijeveenseweg, Meppel 06:24 07:21 08:23 09:20a 10:20a De Schalle, Nijeveen 06:28 07:25 08:27 09:24a 10:24a Molenweg, Nijeveen 06:29 07:26 08:28 09:25a 10:25a Gemeentehuis, Nijeveen 06:29 07:27 08:29 09:25a 10:25a Kerkweg,Zonneberg,Veendijk, NijeveenVeendijk Nijeveen 06:31 07:29 08:31 09:27a 10:27a Bovenboer,Havelterberg,Rotonde, Havelterberg Veendijk Havelterberg 06:36 07:34 08:36 09:32a 10:32a Onnaseveld,Bedelaarspad, Steenwijk Steenwijk 06:38 07:36 08:38 09:34a 10:34a Kallenkoterallee, Steenwijk 06:39 07:38 08:39 09:35a 10:35a Gagelsweg,Oostercluft,'tWestercluft,Station, Schar, SteenwijkSteenwijk SteenwijkSteenwijk A 06:19 06:47 07:46 08:47 09:43a 09:48 10:43a 10:48 Station, Steenwijk V 06:48 07:47 08:48 Oostermeenthe, Steenwijk 06:20 06:49 07:48 08:49 09:49 10:49 Hooilanden,Bultweg, Eesveen Eesveen 06:23 06:52 07:51 08:52 09:52 10:52 De Eese, Eesveen 06:25 06:54 07:53 08:54 09:54 10:54 Gierwal,Bosschasteeg,Schoolweg, Eesveen Nijensleek Nijensleek 06:27 06:56 07:55 08:56 09:56 10:56 DeBeukenlaan, Delle, Frederiksoord Frederiksoord 06:29 06:58 07:57 08:58 09:58 10:58 VledderwegHertenkamp,Dorpsstraat,Brink, Vledder 23, VledderVledder Vledder 06:33 07:02 08:02 -

Gekleurde Dagroutes Voor Ruiters En Menners
Te paard door het Nationaal Park Dwingelderveld. Een geweldige ervaring. Staatsbosbeheer, Natuurmonumenten en de Vrijwilligersgroep Ruiters en Menners DWV hebben voor u een uitgebreid netwerk van ruiter- en men paden aangelegd door één van de grootste bijzondere natuurgebieden van Nederland. Het Nationaal Park heeft voor u drie Dagroutes uitgezet waarbij start- en eindpunt gelijk zijn. De Dagroutes zijn gekleurd, hebben een lengte van ongeveer 18 km, beginnen bij een (paardentrailer-)parkeerplaats en zijn in beide richtingen te berijden. De gekleurde nummering geeft u een oriëntatie in het veld. Op bepaalde nummers kunt u de route koppelen aan een andere kleur om de route langer of korter te maken. Soms zijn dit in het veld de witte verbindings- routes. De zwarte verbindingsroutes sluiten aan op de dorpskernen en maneges. Zie kaart achterzijde. Bewegwijzering ▶ Rijd alleen op de aangegeven Routes zijn aangegeven door ruiter-en menroutes paaltjes, meestal op kniehoogte en ▶ Laat uw paard niet uit vennen zijn voor ruiters en menners. drinken; ▶ Laat geen afval achter. Startpunten ▶ Passeer medegasten alleen in De startpunten zijn ruime verharde stap. parkeerplaatsen waar de trailers ▶ Ruim mest op bij de ruim kunnen parkeren en makkelijk parkeerplaats. weer wegrijden. In de regel vlak bij ▶ Laat eventueel uw mobiele een horecavoorziening. nummer zichtbaar achter op uw dashboard. Bij calamiteiten Rode route: 17 km. kunnen we contact opnemen. Paardentrailerparkeerplaats bij Natuurpoort Spier. Wij wensen u veel rij- en Adres: Oude Postweg, voorbij 12, menplezier in het Nationaal Park 9417TG Spier. Dwingelderveld! Langs de weg wordt de Opmerkingen of beschadigingen Paardentrailerparkeerplaats kunt u doorgeven via de website aangegeven. www.np-dwingelderveld .nl. -

Provincie Drenthe Jongere Bouwkunst En Stedeboüw
PROVINCIE DRENTHE JONGERE BOUWKUNST EN STEDEBOÜW 1850-1940 MIP/DRENTHE GEMEENTEBESCHRIJVING DWINGELOO (ontwerp) APRIL 1989 DWINGELOO Inleiding De gemeente Dwingeloo maakt deel uit van het inventarisatiegebied Zuidwest-Drenthe en omvat naast het hoofddorp Dwingeloo de nederzet- tingen Dieverbrug, Eemster, Geeuwenbrug, Leggeloo, Lhee en Lhee- broek. Het grondgebied wordt begrensd door in het noorden de gemeente Smilde, in het oosten de gemeente Beilen, in het zuiden de gemeente Ruinen, in het zuidwesten de gemeente Havelte en in het westen de gemeente Diever. De huidige omvang van Dwingeloo bedraagt 6.882 hec- tare. Het inwonertal vertoont sinds 1850 het volgende verloop: 1850- 1.437, 1900-2.357, 1940-3.227, 1988-3.687. Fysische gesteldheid De gemeente Dwingeloo is gelegen op een sterk door landijs beïnvloed gedeelte van het Drents Plateau. Talloze kleine en grotere smelt- waterdalen werden hier in het keileem uitgeslepen. Zo wordt het grondgebied van de gemeente Dwingeloo in een noordelijke en een zui- delijke helft verdeeld door een breed dal, waarin de Dwingelerstroom met zijn vertakkingen thans zijn beloop vindt. Tijdens de koudere periode van het Weichselien (laatste ijstijd) ontstonden talloze pingoruïnes (dobben) en kwam vrijwel het gehele grondgebied van de huidige gemeente onder een laag dekzand van wisselende dikte te lig- gen. Dit had tot gevolg dat de stroomdalen enigszins afgevlakt werden. Het microreliëf op de hoger gelegen plateau's werd ver- sterkt. In de stroomdalen trad in een latere warmere periode van het Holo- veen beekafzetting en veenvorming op. De bodems die hier voorkomen behoren tot de venige beekdalgronden. Het op geringe afstand (vrij- wel overal binnen 120 cm) onder het maaiveld voorkomen van keileem heeft tot gevolg gehad dat plaatselijk ook veenvorming op de hogere zandgronden kon optreden. -

Gebruikersplatform Dinsdagavond 2 April 2019 | Camping Diever
Gebruikersplatform Dinsdagavond 2 april 2019 | Camping Diever Aanwezig: Catrien Scholten (Provincie Drenthe), Henk van Hooft (voorzitter Stuurgroep), Nico Driessen (IVN), Corné Joziasse (Staatsbosbeheer), Patrick Witteveen (Plaatselijk belang Appelscha), Appie Boonstra (Plaatselijk belang Appelscha), Jan Mos (Plaatselijk belang Appelscha), Lian Fikkema (Natuurmonumenten), Jantsje Bijmholt (Plaatselijk belang Langedijke), Inge Jager (Plaatselijk belang Dieverbrug), Rikus Kloeze (Dorpsbelangen Diever), Ard Oudshoorn (Plaatselijk belang Elsloo), Gerard Gomarus (Stichting sportpromotie en wandelvierdaagse Diever), Clara Boschma (Dorpsgemeenschap Doldersum), Frans van Rossum (De Veldmenners), Jan Hoeks (Dorpsbelang Hoogersmilde), Marjan Ike (Camping Diever), Elaine Sapulete (Provincie Drenthe) 1. Opening Catrien opent de vergadering en heet iedereen van harte welkom. - Appie Boonstra en Jan Mos van plaatselijk belang Appelscha zullen Patrick Witteveen vervangen. 2. Wilde natuur stand van zaken Toegelicht door Catrien aan de hand van een presentatie. Vragen vanuit de groep over de stilte gebieden. Wat houdt het in voor de recreatie? De routes worden verlegd maar hoe wordt het proces aangepakt? Grote groepen mensen kun je gaan sturen, door de routes te verplaatsen. Hoe gaan de routes eruit zien. Hoe wordt dat proces voor hoe het wordt ingevuld? Je kunt niet alle paaltjes in een keer weg gaan halen en maar hopen dat het nieuwe vanzelf goed komt. Mensen willen toch de natuur in want dat is toch ook wel de reden waarom de mensen naar Drenthe komen. Hoe wordt dit duidelijk gemaakt richting de mensen? - Dat de mensen het bos niet meer in mogen of kunnen is een misverstand. Er blijven wel gewoon paadjes bestaan in het midden en in de randzones blijven ook gewoon bordjes staan! Overal liggen nu routes, hiervan zullen een aantal verdwijnen. -

Nr 1 Visiekaart
+ Kollum Burum + Grijpskerk Niezijl + DOLLARD + Zuidwolde Wagenborgen Kollumerzwaag + Visvliet Noordhorn + Siddeburen + + Eemskanaal Nieuwolda + Aduard + Buitenpost + Zwaagwesteinde Zuidhorn + GRONINGEN + + + Gerkesklooster + + Prinses Margriet Kanaal Schildwolde + Actualisatie + + Lutjegast + + Twijzel + + Niekerk + Hoogkerk + Slochteren Drieborg + Harkstede Kootstertille + Augustinusga + Oostwold + + Eestrum Finsterwolde + + Noordbroek + Midwolda + Surhuizum Grootegast + + Nieuweschans ++ Drogeham Doezum + ++ A7 ++ Nieuw-Beerta + + Bergumer Kolham + + Boerakker W + + meer i + Surhuisterveen nsc h + ote r A7 + Kornhorn Hoornse die meer p + + Beerta + Scheemda Oostermeer Harkema + SAPPEMEER + Eelderwolde Roderwolde Foxholster Zuidbroek + Opende Paterswolde- + meer Lits Haren meer + + + VISIEKAART Nietap Boelenslaan Leek + + + Peize + De Leijen + Paterswolde + Houtigehage Rottevalle + Heerenland 2020 Roden + + HOOGEZAND Oudeschans Marum + + Zuidlaarder WINSCHOTEN + Glimmen + Altena + Eelde meer + Opeinde Winde ++ Drachtstercompagnie + Zevenhuizen + ++ Blijham + + Bunne De Wilp VEENDAM + Oude Pekela DRACHTEN Lieveren + Yde De Punt Midlaren + Roderesch De Groeve Bellingwolde + + + + Legenda Zuidlaarderveen + + Frieschepalen + Steenbergen Donderen A28 + + Zuidlaren + + Langelo Ontwikkelingsopgave Ureterp + Westlaren + Annerveensche- + Robuust natuursysteem kanaal Wildervank + Boornbergum Nieuwe Pekela Vriescheloo + Schuilingsoord Spijkerboor Een + + Robuust natuursysteem Bakkeveen + Tynaarlo Zeegse Schipborg + Haulerwijk Norg Vries + + Annen -
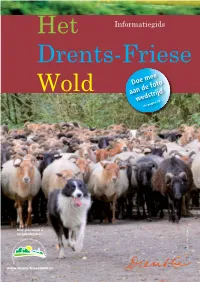
Informatiegids Drents-Friese
Het Informatiegids Drents-Friese Doe mee Wold aan de foto wedstrijd zie pagina 47 Deze gids wordt u aangeboden door: foto: Klaas Dijkstra www.drents-friesewold.nl 5 www.drents-friesewold.nl 15 22 14 28 31 19 9 12 25 10 20 13 23 26 17 16 21 27 19 30 6 1 2 29 18 3 4 Leden; Recreatieondernemers in en rond het Drents-Friese Wold 2 1. Camping Noordenveld Smitstede 1, 7983 LA 19. Bungalow Diever Haarweg 8, 7981 LW Diever Wapse, 0521-551502, [email protected], (adres vakantiehuizen),- contactadres: Lhee 5a www.hetnoordenveld.nl 7991 PE Lhee-Dwingeloo 06-54995884, 2. Camping Diever Haarweg 2, 7981 LW Diever, [email protected], www.bungalowdiever.nl 0521-591644 [email protected], 20.B&B het Kragelhuus Boylerweg 16, 8392 NH 24 www.campingdiever.nl Boyl, 06-25234399, [email protected], 3. Camping Wittelterbrug Wittelterweg 31, 7986 PL www.kragelhuus.nl 33 Wittelte,0521-598288 [email protected], 21. Forellenvijvers en Outdoor Het Oosterseveld www.wittelterbrug.nl Oosterseveldweg 16, 8388 MB Oosterstreek, 7 4. De Vier Eiken Oosteinde 14, 8351 HB 0561-430020/b.g.g. 06-40777624 Wapserveen, 0521-321488 [email protected], [email protected], www.deviereiken.nl www.forellenvijvershetoosterseveld.nl 5. Kramer Fietsservice Boerenstreek 12, 8426 BP 22. Boscamping en Groepsaccommodatie Appelscha Appelscha, 0516-433699 [email protected], Oude Willem 3, 8426 SM Appelscha, www.fietsservice.nl 0516-431391 [email protected], 6. HR De Wapser Herberg Ten Darperweg 104, www.boscampingappelscha.nl 7983 KP Wapse, 0521- 551278 23. Hoeve aan den Weg Bosweg 12, 8439 SN Oude [email protected], www.wapserherberg.nl Willem, 0521-387269 [email protected] 32 7. -

623-Technische-Gids.Pdf
Drentse Acht van Westerveld -zondag 12 maart 2017 38 39 40 KM te rijden Omschrijving Tijdschema Start Dwingeloo-Hotel Wesseling Brink 13:00 13:00 13:00 Neutralisatie Neutrale start Hotel Wesseling Brink - l.a. Brink - Drift - r.a. Esweg - r.a. Poolweg - r.a. Heuvelenweg - rechtdoor Brink Hampshire Hotel Wesseling - Enthingeweg - Einde Dwingeloo - \ rotonde rechtdoor Dwingelderdijk Officiele start Dwingelderdijk 0 143,1 Dwingelderdijk 13:08 13:08 13:08 1,0 142,1 Dieverbrug 13:09 13:09 13:09 1,5 141,6 r.a. Dwingelderdijk 13:10 13:10 13:10 1,7 141,4 Rotonde rechtdoor 13:10 13:10 13:10 2,3 140,8 Einde Dieverbrug 13:11 13:11 13:11 2,8 140,3 Diever 13:12 13:12 13:12 2,9 140,2 Moleneinde, Hoofdstraat 13:12 13:12 13:12 3,1 140,0 l.a. Peperstraat 13:12 13:12 13:12 3,4 139,7 r.a. Hoofdstraat 13:13 13:13 13:13 3,9 139,2 Einde Diever 13:14 13:14 13:13 4,0 139,1 Voorrangsweg l.a. Ten Darperweg 13:14 13:14 13:13 6,9 136,2 Wapse 13:18 13:18 13:18 7,6 135,5 Einde Wapse 13:19 13:19 13:19 10,0 133,1 Wapserweg 13:23 13:23 13:22 10,7 132,4 Vledder 13:24 13:24 13:23 11,1 132,0 r.a. Brink, De Hoek, Torenlaan 13:25 13:25 13:24 11,7 131,4 r.a. -

Informatiemap Hervormde Gemeenten Diever En Dwingeloo Profiel Van Gemeenten En Predikant 2019-2020
Informatiemap Hervormde Gemeenten Diever en Dwingeloo Profiel van gemeenten en predikant 2019-2020 1 Inleiding Voor u ligt de informatiemap van onze beide hervormde gemeenten. Als al onze plannen doorgaan zal er binnen enkele jaren sprake zijn van één kerkelijke gemeente, het proces daartoe is in volle gang. Voor deze gemeente(n) zoeken wij een predikant, omdat het echtpaar dat als predikant Diever en Dwingeloo bediende met emeritaat is gegaan. De informatiemap is bedoeld om uw belangstelling voor deze vacature(s) aan te sporen. Een fijne woonomgeving en meelevende enthousiaste gemeenteleden moeten voor een predikant een aantrekkelijke vacature bieden. Wij zien uit naar uw reactie. Voorzitters van de kerkenraden van Diever en Dwingeloo, Tom Griffioen en Gert Jan van Muijen Visie en Missie (vastgesteld 2019) Hervormde Gemeenten te Diever en Dwingeloo deel uitmakend van de Protestantse Kerk in Nederland Visie De gemeenten willen in beide dorpen een plek zijn waar mensen in een vertrouwde omgeving God en elkaar kunnen ontmoeten. Het woord van God, zoals wij dat in de bijbel vinden, is onze bron. We geven ruimte voor ieders eigen beleving, waarin we elkaar respecteren, zodat ieder zich veilig en gezien voelt. De kerkelijke gemeenschap is een plaats van bezinning om te zoeken naar: - de uitdaging om het goede te doen - troost, rust en bemoediging - geborgenheid voor een ieder, ongeacht geaardheid of afkomst - hulp voor wie dat nodig heeft. Missie Dit brengen wij in praktijk door: - Gods naam “Ik zal er zijn” zichtbaar proberen te maken - het -

Ontsluitingen Nationaal Park Drents-Friese Wold
Ontsluitingen Nationaal Park Drents-Friese Wold Eindrapport Provincie Drenthe Grontmij ICT Assen, 20 juni 2002 @ Grontmij , rev. Verantwoording Titel : Ontsluitingen Nationaal Park Drents-Friese Wold Projectnummer : 0112961 Documentnummer : Revisie : Datum : 20 juni 2002 Auteur(s) : Iwan Veeman en Ru Bijlsma (landschapsecologie) H. Hoekstra, I. Veeman, A. Niemeijer, R. Bijlsma en T. Wassenaar (projectleider) Fotoùs Grontmij e-mail adres : [email protected] Gecontroleerd : Paraaf gecontroleerd : Goedgekeurd : Paraaf goedgekeurd : @ Grontmij blad 2 van 58 Inhoudsopgave 1 Hoofdrapport................................................................................ 5 1.1 Inleiding ........................................................................................ 5 1.2 Werkwijze...................................................................................... 5 1.3 Status van het rapport ................................................................... 6 1.4 Landschapsecologische situatie...................................................... 6 1.5 Hydrologische situatie ................................................................... 7 1.6 Verkeerskundige situatie................................................................ 8 1.7 Maatregelen................................................................................... 8 2 Achtergronddocument - Inleiding................................................ 17 2.1 Aanleiding onderzoek.................................................................. 17 2.2 Doel ........................................................................................... -

Gemeente Westerveld & Actium
Gemeente Westerveld & Actium Woningmarktverkenning 25 november 2016 DATUM 25 november 2016 TITEL Woningmarktverkenning ONDERTITEL Definitieve versie Boulevard Heuvelink 104 6828 KT Arnhem Postbus 1174 6801 BD Arnhem OPDRACHTGEVER Gemeente Westerveld & Actium [email protected] www.companen.nl (026) 351 25 32 @Companen BTW NL001826517B01 IBAN NL95RABO0146973909 KVK 09035291 AUTEUR(S) Koen van der Most Bram Klouwen PROJECTNUMMER 1701.101 Inhoud 1 Inleiding 1 1.1 Vraagstelling 1 1.2 Aandachtspunten bij de vraagstelling 1 1.3 Leeswijzer 3 2 ‘Foto’ van de huidige woningmarkt 4 2.1 Demografische ontwikkelingen 4 2.2 Bevolkingssamenstelling 9 2.3 Uitkomsten leefstijlenonderzoek 10 2.4 Samenstelling van de woningvoorraad 11 2.5 Bestaand beleid 15 3 Toekomstige woningbehoefte 18 3.1 Kwantitatieve woningbehoefte 18 3.2 Vraag naar sociale huurwoningen 21 3.3 Woonwensen 23 3.4 Toekomstige kwalitatieve woningbehoefte 26 3.5 Confrontatie huidige plancapaciteit 31 3.6 Conclusies rond mismatch en plannen 32 4 Wonen met zorg 33 Bijlage 37 1 Inleiding De gemeente Westerveld vindt het belangrijk om meer richting te geven aan een prettig woonklimaat. Eind 2016 wil de gemeente in een woonvisie de ambities en (maatschappelijke) opgaven om het woonklimaat te behouden en versterken vastleggen. Om dit mogelijk te maken is een goede analyse van de woningmarkt een vereiste. Op dit moment zijn er namelijk nog teveel onzekerheden over het functioneren van de lokale woningmarkt. Discussies gaan hierdoor vooral over opvattingen en slechts beperkt over feiten. Dit vraagt om een goede analyse van bijvoorbeeld verhuispatronen, toekomst- verwachtingen rond de woningbehoefte, prognoses en maatschappelijke ontwikkelingen. De gemeente heeft daarom samen met Actium een woningmarktanalyse laten uitvoeren die als onderlegger dient voor de komende woonvisie. -

PERS1995016001002.Pdf
PERSOONIA Published by Rijksherbarium / Hortus Botanicus, Leiden Volume Part 81-122 16, 1, pp. (1995) Taxonomical notes on macrofungi in roadside verges planted with trees in Drenthe (The Netherlands) — II Peter-Jan Keizer & Eef Arnolds Biological Station, Wijster (Drenthe), The Netherlands In the second part of this study special attention is paid to the genera Hebeloma, Psathyrel la and Russula. Psathyrella rhombispora is described as a new species. Russula cicatricata of Romagn., R. elaeodes (Bres.) Romagn. and R. purpurata Crawsh. are reduced to formae R. graveolens Romell. in Britz. of earlier & It This paper is a continuation an paper (Keizer Arnolds, 1994). presents descriptions, drawings and observations of rare, critical or less well-known macromycetes carried in road-side that were encountered during mycocoenological investigations out with robur For further verges planted Quercus (53 plots) or Fagus sylvatica (23 plots). of this the reader is referred the first of this details on the scope study, to part paper (Keizer & Arnolds, I.e.). MATERIAL AND METHODS The fungi dealt with in this study comprise the Macrofungi. Groups with relatively of the small orhidden fruit-bodies (e.g. the majority Helotiales, resupinate Aphyllophora- les) have been omitted because a complete inventory would require a much more time consuming search strategy. The following groups have been included: Basidiomycetes: Agaricales; Gasteromycetes; non-resupinate Aphyllophorales and Heterobasidiomycetes. Ascomycetes: Clavicipitales: Cordyceps; Elaphomycetales: Elaphomyces; Helotiales: Geo- glossum, Leotia; Pezizales: Helvellaceae, Pezizaceae, Tuberaceae; Deuteromycetes: Paeci- lomyces. The nomenclature of the Basidiomycetes is mainly after Kreisel (1987) or Arnolds (1984) if species are not mentioned in the former work.