Ertugliflozin/ Sitagliptin 5/50 Mg, 15/50 Mg, 5/100 Mg and 15/100 Mg
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Does Addition of Vildagliptin to Metformin Monotherapy Improve Glycemic Control in Patients with Type 2 Diabetes Mellitus?
PRACTICE pOINT www.nature.com/clinicalpractice/endmet Does addition of vildagliptin to metformin monotherapy improve glycemic control in patients with type 2 diabetes mellitus? Original article Bosi E et al. (2007) Effects of vildagliptin on OUTCOME MEASURES glucose control over 24 weeks in patients with type 2 diabetes The primary outcome measure was the change inadequately controlled with metformin. Diabetes Care 30: 890–895 in HbA1c level from baseline to study end. Secondary outcome measures included FPG SYNOPSIS levels, lipid profiles, β-cell function, and the KEYWORDS dipeptidyl peptidase 4 inhibitor, incidence and severity of adverse events. glycemic control, HbA1c, type 2 diabetes mellitus, vildagliptin RESULTS BACKGROUND The 50 mg vildagliptin, 100 mg vildagliptin Metformin is frequently prescribed as the and placebo groups comprised 177, 185, and first-line treatment for type 2 diabetes mellitus 182 patients, respectively. Participants were (T2DM); however, additional antidiabetic agents predominantly white and obese, with a mean might be required when glycemic control is age of 54 years. The mean duration of T2DM poor. was 6.2 years, the mean duration of metformin monotherapy was 17 months, and the mean OBJECTIVE metformin dose was 2,100 mg daily. The study To assess the efficacy and safety of the dipeptidyl was completed by >83% of patients in each peptidase 4 (DPP4) inhibitor vildagliptin as group. The mean baseline HbA1c level was 8.4% an add-on to metformin monotherapy. and the mean baseline FPG level was 9.9 mmol/l. Treatment with vildagliptin improved both of DESIGN AND INTERVENTION these parameters. The between-treatment This was a 24-week, multicenter, double- difference (vildagliptin minus placebo) in HbA1c blind, placebo-controlled, randomized study at study end was –0.7% and –1.1% with 50 mg of patients with T2DM inadequately controlled and 100 mg vildagliptin, respectively (P <0.001 with metformin monotherapy. -
Galvus Data Sheet
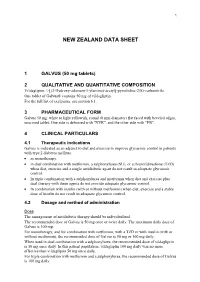
1 NEW ZEALAND DATA SHEET 1 GALVUS (50 mg tablets) 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Vildagliptin: 1-[(3-Hydroxy-adamant-1-ylamino)-acetyl]-pyrrolidine-2(S)-carbonitrile. One tablet of Galvus® contains 50 mg of vildagliptin. For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Galvus 50 mg: white to light yellowish, round (8 mm diameter) flat faced with beveled edges, unscored tablet. One side is debossed with "NVR", and the other side with "FB". 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Galvus is indicated as an adjunct to diet and exercise to improve glycaemic control in patients with type 2 diabetes mellitus. • as monotherapy. • in dual combination with metformin, a sulphonylurea (SU), or a thiazolidinedione (TZD) when diet, exercise and a single antidiabetic agent do not result in adequate glycaemic control. • In triple combination with a sulphonylurea and metformin when diet and exercise plus dual therapy with these agents do not provide adequate glycaemic control. • In combination with insulin (with or without metformin) when diet, exercise and a stable dose of insulin do not result in adequate glycaemic control. 4.2 Dosage and method of administration Dose The management of antidiabetic therapy should be individualized. The recommended dose of Galvus is 50 mg once or twice daily. The maximum daily dose of Galvus is 100 mg. For monotherapy, and for combination with metformin, with a TZD or with insulin (with or without metformin), the recommended dose of Galvus is 50 mg or 100 mg daily. When used in dual combination with a sulphonylurea, the recommended dose of vildagliptin is 50 mg once daily. -

Vildagliptin/Metformin Hydrochloride Novartis, INN-Vildagliptin/Metformin
European Medicines Agency Evaluation of Medicines for Human Use Doc.Ref.: EMEA/CHMP/656453/2008 ASSESSMENT REPORT FOR Vildagliptin/metformin hydrochloride Novartis International Nonproprietary Name: vildagliptin / metformin hydrochloride Procedure No. EMEA/H/C/001050 Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu © European Medicines Agency, 2008. Reproduction is authorised provided the source is acknowledged TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1 Submission of the dossier ........................................................................................................ 3 1.2 Steps taken for the assessment of the product.......................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1 Introduction.............................................................................................................................. 4 2.2 Quality aspects......................................................................................................................... 4 2.3 Non-clinical aspects................................................................................................................. 4 2.4 Clinical -

Dipeptidyl Peptidase-4 Inhibitor Switching
abetes & Di M f e t o a Tanaka et al., J Diabetes Metab 2016, 7:9 l b a o n l r i DOI: 10.4172/2155-6156.1000701 s u m o J Journal of Diabetes & Metabolism ISSN: 2155-6156 Research Article Open Access Dipeptidyl Peptidase-4 Inhibitor Switching as an Alternative Add-on Therapy to Current Strategies Recommended by Guidelines: Analysis of a Retrospective Cohort of Type 2 Diabetic Patients Masami Tanaka*, Takeshi Nishimura, Risa Sekioka and Hiroshi Itoh Department of Internal Medicine, School of Medicine, Keio University 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan Abstract Objective: This retrospective cohort study aimed to investigate the significance of dipeptidyl peptidase-4 (DPP- 4) inhibitor switch therapy, which is currently not recommended by major diabetes guidelines. Methods: The subjects were 238 outpatients with type 2 diabetes who had been prescribed sitagliptin 50 mg daily, which was subsequently changed in one of three ways. Patients whose sitagliptin was switched to vildagliptin 50 mg twice daily were defined as the switched group. Patients whose sitagliptin was increased to 100 mg once daily were defined as the increased group. Patients who received an additional alfa-glucosidase inhibitor (α-GI) three times daily prior to meals and sitagliptin 50 mg once daily were defined as the added group. The primary endpoint was the glycated hemoglobin (HbA1c) value at 6 months after the medication change. Patients whose oral hypoglycemic agents were changed within 6 months after switching to vildagliptin, increasing sitagliptin, or adding α-GI were excluded from the full analysis set and the remaining patients were included in the per protocol analysis. -

Eucreas, INN-Vildagliptin / Metformin Hydrochloride
SCIENTIFIC DISCUSSION 1. Introduction The pathophysiology of Type 2 diabetes mellitus (T2DM) is characterised by deficient insulin activity arising from decreased insulin secretion secondary to beta cell failure, and/or compromised insulin action in peripheral target tissues (insulin resistance). This abnormal metabolic state is exacerbated by excess hepatic glucose production and altered metabolism of proteins and lipids, which along with hyperglycaemia, contribute to microvascular and macrovascular complications. T2DM accounts for approximately 85% to 95% of diabetes cases in developed regions like the European Union. Age and weight are established risk factors for T2DM. The majority of patients with T2DM are overweight or obese. Diet modification and exercise is the first line of treatment for T2DM. Pharmacologic intervention with one oral antidiabetic drug (OAD) is usually the next step in treatment. After 3 to 9 years of OAD monotherapy, patients typically require an additional intervention. The recommended first line treatment is metformin, which restrains hepatic glucose production and decreases peripheral insulin resistance. Sulphonylureas, which are insulin secretagogues, may be used as an alternative to patients intolerant to metformin, or as an addition to metformin. Other second line oral treatment alternatives include alpha-glucosidase inhibitors, meglitinides and thiazolidinediones. Recently the first GLP-1 analogue, exenatide, and the first DPP-4 inhibitors, sitagliptin and vildagliptin, were approved by the CHMP. Vildagliptin belongs to a new class of oral anti-diabetic drugs and is a selective and reversible inhibitor of Dipeptidyl peptidase 4 (DPP-4), the enzyme which inactivates the incretin hormones, glucagon-like peptide-1 (GLP-1), and glucose-dependent insulinotropic polypeptide (GIP), hormones which significantly contribute to the maintenance of glucose homeostasis. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -

Essential Medicines List (EML) 2017 Application for the Revision Of
Essential Medicines List (EML) 2017 Application for the revision of second line treatments of type II diabetes: considered agents that can be used in combination with metformin are sulfonylureas, meglitinides, alpha-glucosidase inhibitors, TZDs, DPP-4 inhibitors, SGLT-2 inhibitors, GLP-1 agonists, basal insulins, bolus insulins, and biphasic insulins. General items 1. Summary statement of the proposal for inclusion, change or deletion In type 2 diabetes, when initial therapy with lifestyle interventions and metformin monotherapy are unsuccessful, a second oral or injectable agent is recommended. This is referred to as ‘second-line therapy’. Historically, insulin or sulfonylureas have been preferred second-line agents because of efficacy, side-effect profiles, long-term safety, and relative cost. Both insulin and sulfonylurea are listed as essential medicines, along with metformin. In 2013 the Expert Committee of Essential Medicines Selection and Use evaluated evidence comparing four groups of oral hypoglycemics: (1) dipeptidyl peptidase-4 (DPP-4) inhibitors, (2) thiazolidinediones, (3) alpha-glucosidase inhibitors, such as acarbose, and (4) meglitinides, against metformin (biguanide) and sulfonylureas (WHO Technical Report Series 985). The results from the 2013 review indicated that there were no apparent differences in efficacy across drug classes, and that sulfonylureas were the most cost-effective treatment option. Based on these analyses, the Expert Committee recommended that “there was insufficient evidence to show that any of the medicines in the four groups (DPP-4 inhibitors, alphaglucosidase inhibitors, meglitinides, or thiazolidinediones) offered any efficacy or safety advantages over the existing medicines included in the EML”, (i.e. metformin first line and sulfonylurea second line). Since then, a new drug class has entered the market of several countries for the treatment of patients with T2D — sodium-glucose cotransporter-2 (SGLT-2) inhibitors. -

Vildagliptin/Metformin Hydrochloride) Film-Coated Tablet
AUSTRALIAN PRODUCT INFORMATION – GALVUMET® (VILDAGLIPTIN/METFORMIN HYDROCHLORIDE) FILM-COATED TABLET 1 NAME OF THE MEDICINE vildagliptin/metformin hydrochloride 2 QUALITATIVE AND QUANTITATIVE COMPOSITION GALVUMET film coated tablets are available in 3 strengths: • GALVUMET 50/500: 50 mg vildagliptin and 500 mg metformin hydrochloride • GALVUMET 50/850: 50 mg vildagliptin and 850 mg metformin hydrochloride • GALVUMET 50/1000: 50 mg vildagliptin and 1,000 mg metformin hydrochloride For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM GALVUMET 50/500: light yellow, ovaloid bevelled edge, film-coated tablet imprinted with "NVR" on one side and "LLO" on the other side. GALVUMET 50/850: yellow, ovaloid bevelled edge, film-coated tablet imprinted with "NVR" on one side and "SEH" on the other side. GALVUMET 50/1000: dark yellow, ovaloid bevelled edge, film-coated tablet imprinted with "NVR" on one side and "FLO" on the other side. 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS For patients with Type 2 diabetes mellitus (T2DM): GALVUMET is indicated as an adjunct to diet and exercise to improve glycaemic control in patients whose diabetes is not adequately controlled on metformin hydrochloride alone or who are already treated with the combination of vildagliptin and metformin hydrochloride, as separate tablets. Treatment should not be initiated with this fixed-dose combination. GALVUMET is indicated in combination with a sulfonylurea (i.e. triple combination therapy) as an adjunct to diet and exercise in patients inadequately controlled with metformin and a sulfonylurea. GALVUMET is indicated as add-on to insulin as an adjunct to diet and exercise to improve glycaemic control in patients when stable dose of insulin and metformin alone do not provide adequate glycaemic control. -

Adverse Drug Effects Observed with Vildagliptin Versus Pioglitazone Or
Bundhun et al. BMC Pharmacology and Toxicology (2017) 18:66 DOI 10.1186/s40360-017-0175-0 RESEARCH ARTICLE Open Access Adverse drug effects observed with vildagliptin versus pioglitazone or rosiglitazone in the treatment of patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials Pravesh Kumar Bundhun1, Girish Janoo2, Abhishek Rishikesh Teeluck2 and Feng Huang3* Abstract Background: Vildagliptin and pioglitazone/rosiglitazone are emerging Oral Hypoglycemic Agents (OHAs) which are used to treat patients suffering from Type 2 Diabetes Mellitus (T2DM). In this analysis, we aimed to systematically compare the adverse drug events which were observed with the use of vildagliptin versus pioglitazone or rosiglitazone respectively. Methods: Online databases were searched for studies comparing vildagliptin with pioglitazone/rosiglitazone. Adverse drug events were considered as the clinical endpoints in this analysis. We calculated Odds Ratios (OR) with 95% Confidence Intervals (CIs) using the RevMan 5.3 software. All the authors had full access to the data which were used and approved the final version of the manuscript. Results: A total number of 2396 patients were analyzed (1486 and 910 patients were treated with vildagliptin and pioglitazone/rosiglitazone respectively). Vildagliptin and pioglitazone/rosiglitazone were both associated with similar overall adverse drug events (OR: 1.00, 95% CI: 0.81–1.24; P = 1.00). Headache (OR: 0.88, 95% CI: 0.60–1.27; P = 0.49) and upper respiratory tract infection (OR: 0.95, 95% CI: 0.71–1.27; P = 0.75) were similarly observed. However, dizziness was significantly lower with pioglitazone/rosiglitazone (OR: 0.63, 95% CI: 0.43–0.92; P = 0.02). -

Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use
F E A T U R E A R TICLE Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use John R. White, Jr., PA, PharmD decade and a half ago, the on insulin biosynthesis and its inhibition creation of molecules that circumvent or choice of an oral antihypergly- of glucagon release.2 reduce the rate degradation by DPP-IV Acemic agent for any particu- Because GLP-1 stimulates insulin while maintaining the agonist effects of lar patient was in some ways a debate secretion only under hyperglycemic GLP-1 has been pursued aggressively. of nuance. Sulfonylureas (SUs) were conditions, there is minimal risk of One GLP-1 analog (exenatide) is avail- the only class available, and provid- hypoglycemia, making this molecule and able in the United States, and another ers were left to sift though pharmacoki- its congeners likely candidates for use as (liraglutide) is in phase III trials. netic, small efficacy, and sometimes sig- antihyperglycemic agents. GLP-1 is also In addition to GLP-1 analogs, mol- nificant side effect differences among associated with increased satiety, possi- ecules that inhibit the activity of DPP-IV the various choices within this class. The bly because it reduces the rate of gastric and thereby prolong the activity of situation today demands a more robust emptying. People with type 2 diabetes endogenous GLP-1 are of great interest. evaluation of multiple categories of med- have reduced circulating levels of GLP-1 Because GLP-1 analogs are proteina- ications with different mechanisms of but retain their ability to respond to this cious in structure, they will most likely action. -

Efficacy and Short-Term Side Effects of Sitagliptin, Vildagliptin and Saxagliptin in Chinese Diabetes: a Randomized Clinical Trial
ID: 18-0523 8 4 X Zhou, L Ding et al. Efficacy and short-term side 8:4 318–325 effects of DPP4 inhibitors RESEARCH Efficacy and short-term side effects of sitagliptin, vildagliptin and saxagliptin in Chinese diabetes: a randomized clinical trial Xiao-jun Zhou1,*, Lin Ding1,*, Jia-xin Liu1, Le-qun Su2, Jian-jun Dong3 and Lin Liao1 1Department of Endocrinology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, Shandong, China 2Department of Pharmacy, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, Shandong, China 3Division of Endocrinology, Department of Medicine, Qilu Hospital of Shandong University, Shandong University, Jinan, Shandong, China Correspondence should be addressed to L Su or J Dong or L Liao: [email protected] or [email protected] or [email protected] *(X Zhou and L Ding contributed equally to this work) Abstract Aims: To investigate the difference in the efficacy among dipeptidyl peptidase-4 (DPP-4) Key Words inhibitors in Chinese adults with newly diagnosed diabetes. f dipeptidyl peptidase-4 Materials and methods: In a multicenter, randomized study, we enrolled adults who were inhibitors either treatment naive or off prior anti-hyperglycemic therapy for at least 3 months. f hemoglobin A1c Eligible patients had hemoglobin A1c (HbA1c) concentrations of 6.5–9.5%. Three hundred f Chinese patients had been randomly allocated to sitagliptin 100 mg, once daily; vildagliptin 50 mg, f diabetes twice daily and saxagliptin 5 mg, once daily for 12 weeks. Patients and investigators were masked to treatment assignment. The primary endpoint was change from baseline in HbA1c at week 12. This study was completed and registered with ClinicalTrials.gov, number NCT 01703637. -

Is the Use of DPP-4 Inhibitors Associated with an Increased Risk for Heart Failure?
S210 Diabetes Care Volume 39, Supplement 2, August 2016 Is the Use of DPP-4 Inhibitors Guntram Schernthaner,1 Avivit Cahn,2 and Itamar Raz2 RECENT OUTCOME STUDIES Associated With an Increased Risk for Heart Failure? Lessons From EXAMINE, SAVOR-TIMI 53, and TECOS Diabetes Care 2016;39(Suppl. 2):S210–S218 | DOI: 10.2337/dcS15-3009 About 40 years ago, the Framingham study first documented that the risk for heart failure (HF) in patients with diabetes was about twofold higher in men and fivefold in women compared with individuals without diabetes (1). The UK Prospective Di- abetes Study (UKPDS) reported that the incidence of hospital admission for HF was similar to that of nonfatal myocardial infarction and nonfatal stroke (2). A more recent 6-year follow-up study of 65,619 patients with type 2 diabetes treated with insulin reported that the hospital admission rate due to HF (243 of 10,000) was higher than that due to myocardial infarction (97 of 10,000) or stroke (151 of 10,000) (3). The pathogenesis of HF in diabetes is multifactorial but can largely be attributed to four key factors: coronary artery disease (CAD), hypertension, diabetic cardio- myopathy, and extracellular fluid volume expansion (4,5). Remarkably, type 2 di- abetes itself is a recognized risk factor for HF, independent of CAD and hypertension (4), suggesting that glycemic control may influence the development of HF. Hyper- glycemia can exert deleterious effects on the myocardium and has been shown to increase oxidative stress, promote accumulation of advanced glycation end prod- ucts, and cause interstitial fibrosis (6).