Fungi Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Boards' Fodder
boards’ fodder Medical Mycology By Adriana Schmidt, MD, and Natalie M. Curcio, MD, MPH. (Updated July 2015*) SUPERFICIAL ORGANISM CLINICAL HISTO/KOH TREATMENT MYCOSES* Pityriasis Malessezia furfur Hypo- or hyper-pigmented Spaghetti & meatballs: Antifungal shampoos and/or versicolor macules short hyphae + yeast PO therapy Tinea nigra Hortaea werneckii (formerly Brown-black non-scaly Branching septate hyphae Topical imidazoles or palmaris Phaeoannellomyces werneckii) macules + budding yeast allylamines Black piedra Piedraia hortae Hard firm black Dark hyphae around concretions acrospores Cut hair off, PO terbinafine, White piedra Trichosporon ovoides or inkin Soft loose white Blastoconidia, imidazoles, or triazoles (formely beigelii) concretions arthroconidia Fluorescent small Microsporum Canis KOH: spores on outside spore ectothrix: M. audouinii of the hair shaft; “Cats And Dogs M. distortum Wood’s lamp --> yellow Sometimes Fight T. schoenleinii fluorescence & Growl” M. ferrugineum+/- gypseum Large spore Trichophyton spp. (T. tonsurans in North America; T. violaceum in KOH: spores within hair Topical antifungals; PO endothrix Europe, Asia, parts of Africa). shaft antifungals for T. manuum, Tinea corporis T. rubrum > T. mentag. Majocchi’s granuloma: T. rubrum capitis, unguium T. pedis Moccasin: T. rubrum, E. floccosum. Interdigital/vesicular: T. mentag T. unguium Distal lateral, proximal and proximal white subungual: T. rubrum. White superficial: T. mentag. HIV: T. rubrum SUBQ MYCOSES** ORGANISM TRANSMISSION CLINICAL HISTO/KOH TREATMENT -

Black Fungal Extremes
Studies in Mycology 61 (2008) Black fungal extremes Edited by G.S. de Hoog and M. Grube CBS Fungal Biodiversity Centre, Utrecht, The Netherlands An institute of the Royal Netherlands Academy of Arts and Sciences Black fungal extremes STUDIE S IN MYCOLOGY 61, 2008 Studies in Mycology The Studies in Mycology is an international journal which publishes systematic monographs of filamentous fungi and yeasts, and in rare occasions the proceedings of special meetings related to all fields of mycology, biotechnology, ecology, molecular biology, pathology and systematics. For instructions for authors see www.cbs.knaw.nl. EXECUTIVE EDITOR Prof. dr Robert A. Samson, CBS Fungal Biodiversity Centre, P.O. Box 85167, 3508 AD Utrecht, The Netherlands. E-mail: [email protected] LAYOUT EDITOR S Manon van den Hoeven-Verweij, CBS Fungal Biodiversity Centre, P.O. Box 85167, 3508 AD Utrecht, The Netherlands. E-mail: [email protected] Kasper Luijsterburg, CBS Fungal Biodiversity Centre, P.O. Box 85167, 3508 AD Utrecht, The Netherlands. E-mail: [email protected] SCIENTIFIC EDITOR S Prof. dr Uwe Braun, Martin-Luther-Universität, Institut für Geobotanik und Botanischer Garten, Herbarium, Neuwerk 21, D-06099 Halle, Germany. E-mail: [email protected] Prof. dr Pedro W. Crous, CBS Fungal Biodiversity Centre, P.O. Box 85167, 3508 AD Utrecht, The Netherlands. E-mail: [email protected] Prof. dr David M. Geiser, Department of Plant Pathology, 121 Buckhout Laboratory, Pennsylvania State University, University Park, PA, U.S.A. 16802. E-mail: [email protected] Dr Lorelei L. Norvell, Pacific Northwest Mycology Service, 6720 NW Skyline Blvd, Portland, OR, U.S.A. -

Indoor Wet Cells As a Habitat for Melanized Fungi, Opportunistic
www.nature.com/scientificreports OPEN Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other Received: 23 June 2017 Accepted: 30 April 2018 vertebrates Published: xx xx xxxx Xiaofang Wang1,2, Wenying Cai1, A. H. G. Gerrits van den Ende3, Junmin Zhang1, Ting Xie4, Liyan Xi1,5, Xiqing Li1, Jiufeng Sun6 & Sybren de Hoog3,7,8,9 Indoor wet cells serve as an environmental reservoir for a wide diversity of melanized fungi. A total of 313 melanized fungi were isolated at fve locations in Guangzhou, China. Internal transcribed spacer (rDNA ITS) sequencing showed a preponderance of 27 species belonging to 10 genera; 64.22% (n = 201) were known as human opportunists in the orders Chaetothyriales and Venturiales, potentially causing cutaneous and sometimes deep infections. Knufa epidermidis was the most frequently encountered species in bathrooms (n = 26), while in kitchens Ochroconis musae (n = 14), Phialophora oxyspora (n = 12) and P. europaea (n = 10) were prevalent. Since the majority of species isolated are common agents of cutaneous infections and are rarely encountered in the natural environment, it is hypothesized that indoor facilities explain the previously enigmatic sources of infection by these organisms. Black yeast-like and other melanized fungi are frequently isolated from clinical specimens and are known as etiologic agents of a gamut of opportunistic infections, but for many species their natural habitat is unknown and hence the source and route of transmission remain enigmatic. Te majority of clinically relevant black yeast-like fungi belong to the order Chaetothyriales, while some belong to the Venturiales. Propagules are mostly hydro- philic1 and reluctantly dispersed by air, infections mostly being of traumatic origin. -

Redalyc.Moringa Oleifera Inhibits Growth of Candida Spp. And
Ciência Rural ISSN: 0103-8478 [email protected] Universidade Federal de Santa Maria Brasil Gadelha Rocha, Marcos Fábio; Pereira de Alencar, Lucas; Nogueira Brilhante, Raimunda Sâmia; de Alencar Sales, Jamille; Brito de Ponte, Yago; de Aragão Rodrigues, Pedro Henrique; de Souza Sampaio, Célia Maria; de Aguiar Cordeiro, Rossana; de Souza Collares Maia Castelo-Branco, Débora; de Oliveira, Francisco Carlos; Barbosa, Francisco Geraldo; Cordeiro Teixeira, Carlos Eduardo; de Araújo Neto Paiva, Manoel; Pinheiro Gomes Bandeira, Tereza de Jesus; Bezerra Moreira, José Luciano; Costa Sidrim, José Júlio Moringa oleifera inhibits growth of Candida spp. and Hortaea werneckii isolated from Macrobrachium amazonicum prawn farming with a wide margin of safety Ciência Rural, vol. 44, núm. 12, diciembre, 2014, pp. 2197-2203 Universidade Federal de Santa Maria Santa Maria, Brasil Available in: http://www.redalyc.org/articulo.oa?id=33132701016 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Ciência Rural, San Mtao rMinagraia o, lve.i4fe4r, an i.n1h2i, bpi.t2s 1g9r7o-w2t2h0 o3f, dCeazn, d2i0d1a4 s p p . a n d H o r t a e a w e r n eckii i shottlpa:t/e/d xfr.doomi. oMrga/c1r0o.b1r5a9c0h/0iu1m03..-.8478cr201402216967 ISSN 0103-8478 Moringa oleifera inhibits growth of Candida spp. and Hortaea werneckii isolated from Macrobrachium -
Monograph on Dimorphic Fungi
Monograph on Dimorphic Fungi A guide for classification, isolation and identification of dimorphic fungi, diseases caused by them, diagnosis and treatment By Mohamed Refai and Heidy Abo El-Yazid Department of Microbiology, Faculty of Veterinary Medicine, Cairo University 2014 1 Preface When I see the analytics made by academia.edu for the visitors to my publication has reached 244 in 46 countries in one month only, this encouraged me to continue writing documents for the benefit of scientists and students in the 5 continents. In the last year I uploaded 3 monographs, namely 1. Monograph on yeasts, Refai, M, Abou-Elyazeed, H. and El-Hariri, M. 2. Monograph on dermatophytes, Refai, M, Abou-Elyazeed, H. and El-Hariri, M. 3. Monograph on mycotoxigenic fungi and mycotoxins, Refai, M. and Hassan, A. Today I am uploading the the 4th documents in the series of monographs Monograph on dimorphic fungi, Refai, M. and Abou-Elyazeed, H. Prof. Dr. Mohamed Refai, 2.3.2014 Country 30 day views Egypt 51 2 Country 30 day views Ethiopia 22 the United States 21 Saudi Arabia 19 Iraq 19 Sudan 14 Uganda 12 India 11 Nigeria 9 Kuwait 8 the Islamic Republic of Iran 7 Brazil 7 Germany 6 Uruguay 4 the United Republic of Tanzania 4 ? 4 Libya 4 Jordan 4 Pakistan 3 the United Kingdom 3 Algeria 3 the United Arab Emirates 3 South Africa 2 Turkey 2 3 Country 30 day views the Philippines 2 the Netherlands 2 Sri Lanka 2 Lebanon 2 Trinidad and Tobago 1 Thailand 1 Sweden 1 Poland 1 Peru 1 Malaysia 1 Myanmar 1 Morocco 1 Lithuania 1 Jamaica 1 Italy 1 Hong Kong 1 Finland 1 China 1 Canada 1 Botswana 1 Belgium 1 Australia 1 Argentina 4 1. -
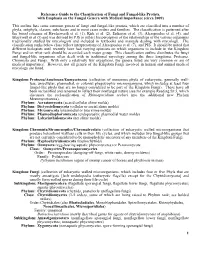
Reference Guide to the Classification of Fungi and Fungal-Like Protists, with Emphasis on the Fungal Genera with Medical Importance (Circa 2009)
Reference Guide to the Classification of Fungi and Fungal-like Protists, with Emphasis on the Fungal Genera with Medical Importance (circa 2009) This outline lists some common genera of fungi and fungal-like protists, which are classified into a number of phyla, subphyla, classes, subclasses and in most cases orders and families. The classification is patterned after the broad schemes of Hawksworth et al. (1), Kirk et al. (2), Eriksson et al. (3), Alexopoulos et al. (4), and Blackwell et al (5) and was devised by PJS to reflect his perception of the relationships of the various organisms traditionally studied by mycologists and included in textbooks and manuals dealing with mycology. The classification ranks below class reflect interpretations of Alexopoulos et al. (7), and PJS. It should be noted that different biologists until recently have had varying opinions on which organisms to include in the Kingdom Fungi and on what rank should be accorded each major group. This classification outline distributes the fungi and fungal-like organisms often dealt with in traditional mycology among the three kingdoms, Protozoa, Chromista and Fungi. With only a relatively few exceptions, the genera listed are very common or are of medical importance. However, not all genera of the Kingdom Fungi involved in human and animal medical mycology are listed. Kingdom: Protozoa/Amebozoa/Eumycetozoa (collection of numerous phyla of eukaryotic, generally wall- less, unicellular, plasmodial, or colonial phagotrophic microorganisms, which includes at least four fungal-like phyla that are no longer considered to be part of the Kingdom Fungi). These have all been reclassified and renamed to reflect their nonfungal nature (see for example Reading Sz 5, which discusses the reclassification of Rhinosporidium seeberi into the additional new Phylum Mezomycetozoea). -

Tinea Nigra by Hortaea Werneckii, a Report of 22 Cases from Mexico
available online at www.studiesinmycology.org STUDIE S IN MYCOLOGY 61: 77–82. 2008. doi:10.3114/sim.2008.61.07 Tinea nigra by Hortaea werneckii, a report of 22 cases from Mexico A. Bonifaz1*, H. Badali3,4,5, G.S. de Hoog3,4, M. Cruz2, J. Araiza1, M.A. Cruz2; L. Fierro2 and R.M. Ponce2 1Department of Mycology and 2Dermatology Service, Hospital General de México, Sánchez Azcona 317-202, Col del Valle, México D.F. CP 03020, Mexico; 3CBS Fungal Biodiversity Centre, P.O. Box 85167, NL-3508 AD Utrecht, The Netherlands; 4Institute of Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands; 5Department of Medical Mycology and Parasitology, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran *Correspondence: Alexandro Bonifaz, [email protected]. Abstract: Tinea nigra is a superficial mycosis caused by Hortaea werneckii. It is an infrequent asymptomatic infection that affects human palms and soles, and is mostly observed in tropical countries. We evaluate retrospectively twenty-two confirmed cases of tinea nigra from a total of eleven yr (1997–2007) and discuss the epidemiology, clinical features and treatment of this disease. In twelve cases, adults were involved, in 10, children. In nineteen cases the disorder was located on palms of hands and in three on soles of feet. In all cases, the obtained isolates were morphologically identified asHortaea werneckii and the identification of ten isolates was retrospectively confirmed with the help of sequences of the internal transcribed spacer regions of the ribosomal DNA. The patients received topical treatment with Whitfield ointment, ketoconazole, bifonazole, or terbinafine. -

White Piedra, Black Piedra, Tinea Versicolor, and Tinea Nigra
IMAGES IN DERMATOLOGY 413 s White piedra, black piedra, tinea versicolor, and tinea nigra: contribution to the diagnosis of superficial mycosis* John Verrinder Veasey1 Ricardo Bertozzi de Avila1 Barbara Arruda Fraletti Miguel1 Laura Hitomi Muramatu1 DOI: http://dx.doi.org/10.1590/abd1806-4841.20176018 Abstract: Superficial mycoses are fungal infections restricted to the stratum corneum and to the hair shafts, with no penetra- tion in the epidermis; they are: white piedra, black piedra, tinea versicolor, and tinea nigra. This study presents images of mycological tests performed in the laboratory, as well as exams performed at the authors office, in order to improve the der- matologist’s knowledge about the diagnosis of these dermatoses, which are common in many countries. Keywords: Culture; Culture media; Dermoscopy; Malassezia; Mycology; Mycoses; Physical examination; Phaeohyphomyco- sis; Piedra; Tinea; Tinea versicolor Skin mycoses are frequent causes of dermatological medi- ed with the agent’s isolation in a fungus culture, with a macroscopic cal appointments in Brazil, whether in public or private healthcare and microscopic mycelium analysis. services.1 These are fungal infections that affect superficial layers of In white piedra, DME reveals hyaline nodules consisting of the skin, hair, and nails, and may be clinically classified as super- arthroconidia and some blastoconidia. The culture is white-yellow- ficial mycoses or deep mycoses. Superficial mycoses are divided ish yeast-like, with a cerebriform aspect. In micromorphology, it is into actual superficial mycoses, superficial cutaneous mycoses, and possible to view rectangular, oval, or round arthroconidia, as well as superficial cutaneous-mucosal mycoses.2,3 the presence of blastoconidia (Figure 2).2,4,5 Actual superficial mycoses are fungal infections of the In black piedra, DME reveals dark nodules attached to the corneum layer or hair cuticle, in which the host’s cell-mediated shaft, containing several ascus, with two to eight fusiform, curved immune response is minimal or absent. -

Atlas of Clinically Important Fungi
Atlas of Clinically Important Fungi Atlas of Clinically Important Fungi Carmen V. Sciortino, Jr. Division of Infectious Diseases University of Louisville School of Medicine, and Robley Rex Veterans Healthcare Medical Center Louisville, Kentucky, USA Copyright © 2017 by John Wiley & Sons, Inc. All rights reserved Published by John Wiley & Sons, Inc., Hoboken, New Jersey Published simultaneously in Canada No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, scanning, or otherwise, except as permitted under Section 107 or 108 of the 1976 United States Copyright Act, without either the prior written permission of the Publisher, or authorization through payment of the appropriate per‐copy fee to the Copyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923, (978) 750‐8400, fax (978) 750‐4470, or on the web at www.copyright.com. Requests to the Publisher for permission should be addressed to the Permissions Department, John Wiley & Sons, Inc., 111 River Street, Hoboken, NJ 07030, (201) 748‐6011, fax (201) 748‐6008, or online at http://www.wiley.com/go/permissions. Limit of Liability/Disclaimer of Warranty: While the publisher and author have used their best efforts in preparing this book, they make no representations or warranties with respect to the accuracy or completeness of the contents of this book and specifically disclaim any implied warranties of merchantability or fitness for a particular purpose. No warranty may be created or extended by sales representatives or written sales materials. The advice and strategies contained herein may not be suitable for your situation. -

Sequence of Cryomyces Antarcticus, the Most Extremophilic Fungus from Antarctica
Nothing Special in the Specialist? Draft Genome Sequence of Cryomyces antarcticus, the Most Extremophilic Fungus from Antarctica Katja Sterflinger1*, Ksenija Lopandic1, Ram Vinay Pandey2,3, Barbara Blasi1, Albert Kriegner2 1 VIBT Extremophile Center, University of Natural Resources and Life Sciences, Vienna, Austria, 2 Austrian Institute of Technology, Vienna, Austria, 3 Institute of Population Genetics, University of Veterinary Medicine, Vienna, Austria Abstract The draft genome of the Antarctic endemic fungus Cryomyces antarcticus is presented. This rock inhabiting, microcolonial fungus is extremely stress tolerant and it is a model organism for exobiology and studies on stress resistance in Eukaryots. Since this fungus is a specialist in the most extreme environment of the Earth, the analysis of its genome is of important value for the understanding of fungal genome evolution and stress adaptation. A comparison with Neurospora crassa as well as with other microcolonial fungi shows that the fungus has a genome size of 24 Mbp, which is the average in the fungal kingdom. Although sexual reproduction was never observed in this fungus, 34 mating genes are present with protein homologs in the classes Eurotiomycetes, Sordariomycetes and Dothideomycetes. The first analysis of the draft genome did not reveal any significant deviations of this genome from comparative species and mesophilic hyphomycetes. Citation: Sterflinger K, Lopandic K, Pandey RV, Blasi B, Kriegner A (2014) Nothing Special in the Specialist? Draft Genome Sequence of Cryomyces antarcticus, the Most Extremophilic Fungus from Antarctica. PLoS ONE 9(10): e109908. doi:10.1371/journal.pone.0109908 Editor: Jason E. Stajich, University of California-Riverside, United States of America Received April 3, 2014; Accepted September 12, 2014; Published October 8, 2014 Copyright: ß 2014 Sterflinger et al. -

Product: 366 - Molds, Rusts and Smuts, Absidia Ramosa
Product: 366 - Molds, Rusts and Smuts, Absidia ramosa Manufacturers of this Product Antigen Laboratories, Inc. - Liberty, MO (Lic. No. 468, STN No. 102223) Search Strategy PubMed: absidia and hypersensitivity; absidia and allergy; absidia ramosa; absidia corymbifera allergy Google: absidia ramosa allergy; absidia ramosa allergy adverse; absidia ramosa allergen; absidia ramosa allergen adverse Nomenclature ATCC website: Absidia ramosa (Lindt) Lendner, teleomorph deposited as Tieghemella italiana (Costantin et Perin) Naumov, teleomorph. Stedmans Book (ATCC Fungus Names, 1993): Absidia corymbifera (Cohn) Saccardo et Trotter,1912. Index Fungorum website: Absidia ramosa (Zopf) Lendn., Mat. fl. crypt. Suisse 3(1): 144 (1908) & Lichtheimia ramosa (Zopf) Vuill., Bull. Soc. mycol. Fr. 19: 126 (1903). Parent Product 366 - Molds, Rusts and Smuts, Absidia ramosa Published Data No supportive data were identified. A. ramosais is an organism associated with mucormycosis and farmers' lung. These are hypersensitivity reactions and do not affect the safety of the extract. Panels: Original Panel Recommendation Reclassification Panel Recommendation Diagnosis: none none Therapy: none none Page 1 of 180 9/9/2011 Product: 367 - Molds, Rusts and Smuts, Achorion (Trichophyton) schoenleinii Recommended Scientific Name Trichophyton schoenleinii Manufacturers of this Product Antigen Laboratories, Inc. - Liberty, MO (Lic. No. 468, STN No. 102223) Search Strategy PubMed: trichophyton schoenleinii and allergy (or allergen); trichophyton schoenleinii Google: trichophyton schoenleinii allergy; trichophyton schoenleinii allergy adverse; trichophyton schoenleinii allergen; trichophyton schoenleinii allergen adverse Nomenclature ATCC website: Trichophyton schoenleinii (Lebert) Langeron et Milochevitch, anamorph deposited as Achorion schoenleinii Remak ex Gueguen, anamorph. Stedmans Book (ATCC Fungus Names, 1993): Trichophyton schoenleinii (Lebert) Langeron et Milochevitch Index Fungorum website: Trichophyton schoenleinii (Lebert) Langeron & Miloch. -

The First Isolation of Hortaea Zverneckii from a Household Guinea Pig
Jpn. J. Med. Mycol. Vol. 43, 175-180, 2002 ISSN 0916-4804 Original Article The First Isolation of Hortaea zverneckii from a Household Guinea Pig Shahana Sharmin1, Kumiko Haritani2, Reiko Tanaka1, Paride Abliz1, Kayoko Takizawa1, Ayako Sano1, Kazutaka Fukushima1, Kazuko Nishimura1, Makoto Miyaji1 1 Research Center for Pathogenic Fungi and Microbial Toxicoses, Chiba University, 1-8-1 Inohana, Chuo-ku, Chiba 260-8673, Japan. 2Namiki Animal Hospital , 7-2-4 Namiki, Abiko, Chiba 270-0011, Japan. Received: 14, March 2002. Accepted: 26, April 2002] Abstract Hortaea werneckii, a black yeast and the causative agent of tinea nigra (a superficial type of dermatomycosis), is a human pathogen and is also found in the environment. It is not highly patho- genic but in the last fifteen to twenty years has been isolated from various human and environmental sources in Japan. As far as we know, there has been no report on the isolation of H. werneckii from animals. Recently, we found a case of a guinea pig with dark superficial lesions on the palm and dor- sal areas. Cultural and morphological studies of scrapings from the lesion showed that the causative agent was a black yeast, which was identified as H. werneckii by morphological study and molecular biological screening. Dl/D2 region of the 26S large subunit rDNA gene of this isolate was identical to those of 11 other H. werneckii isolates used as reference strains in this study. This is the first case recorded of tinea nigra caused by H, werneckii in a guinea pig. Key words: guinea pig, Hortaea werneckii, LSU rDNA gene, tinea nigra zverneckii.