Sandwell COVID-19 Local Outbreak Management Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fr Reed Om of in Nform Matio On
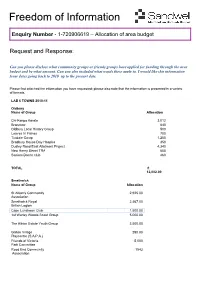
F reedom of Information Enquiry Number - 1-720906619 – Allocation of area budget Request and Response: Can you please disclose what community groups or friends grroups have applied forrf unding through the area budgeet and by what amount. Can you also included what wards these appply to. I wouuld like this information from dates going back to 2010 up to the present date. Please find attached the information you have requested; please also note that the information is presented in a variety of formats. LAB 6 TOWNS 2010-11 Oldbury Name of Group Allocation Chi-Kenpo Karate 3,012 Branzone 840 Oldbury Local History Group 500 Loaves 'n' Fishes 700 Tividale Co-op 1,200 Bradbury House Day Hospice 350 Dudley Road East Allotment Project 4,340 New Henry Street TRA 600 Seniors Dance club 460 TOTAL £ 12,002.00 Smethwick Name of Group Allocation St Alban's Community 2,925.00 Association Smethwick Royal 2,467.00 British Legion Cape Luncheon Club 1,500.00 1st Warley Woods Scout Group 5,000.00 The Albion Estate Youth Group 2,500.00 Galton Village 290.00 Playcentre (S.A.P.A.) Friends of Victoria 5,000 Park Committee Rood End Community 1543 Association Charles Pearson 769 Court Residents Association Midland Heart (on behalf of Penmakers Residents group) 350.00 Victoria Playcentre & 998 Out of School Club Warley Woods Community Trust 1420 Friends of Lightwoods Park 5000 TOTAL 29,762.00 Tipton Name of Group Allocation Tipton Community Association 350 Centenary Methodist Denbigh Playscheme 150 British Legion Tipton Salem Tea Dance 500 Loaves 'n' Fishes 500 -
Sandwell Health and Wellbeing Board
SANDWELL PHARMACEUTICAL NEEDS ASSESSMENT DRAFT VERSION 2.0 JANUARY 2018. CENTRAL HEALTH PHARMACEUTICAL NEEDS ASSESSMENT SANDWELL HEALTH AND WELLBEING BOARD Made in accordance with the National Health Service (Pharmaceutical Services and Local Pharmaceutical Services) Regulations 2013 May 2018 SANDWELL PHARMACEUTICAL NEEDS ASSESSMENT MAY 2018 Produced by: Central Health Solutions Limited In collaboration with: Public Health Department, Sandwell MBC Sandwell Local Pharmaceutical Committee Sandwell Healthwatch Sandwell Clinical Commissioning Group Approved by: Sandwell Health and Wellbeing Board 60 day consultation period: 15th February 2018 - 16th April 2018 Author: Michelle Dyoss, Director, Central Health Solutions Limited (CHSL) Acknowledgements: Jackie Buxton, Len Dalton, Yvonne Goulding, Bruce Prentice, Directors, CHSL Michelle Deenah, NHS England Public Health Analyst: Andy Evans PNA Steering Group Rachel Allchurch Members: Health and Wellbeing Board Project Officer, Sandwell MBC John Clothier Chair, Healthwatch Sandwell Valerie de Souza Consultant in Public Health, Sandwell MBC Ali Din Chief Officer, Sandwell LPC Michelle Dyoss Director, Central Health Solutions Limited Ciaran McSorley Vice Chair, Sandwell LPC Saba Rai Sandwell and West Birmingham CCG This document builds on Sandwell Health and Wellbeing Board’s first PNA published 1st April 2015. Please note data regarding community pharmacies are accurate to December 2017. Supplementary statements will be issued in response to significant changes to pharmaceutical services since the -

Wednesbury to Brierley Hill Metro Extension Business Case
Wednesbury to Brierley Hill Business Case Midland Metro Wednesbury to Brierley Hill Extension June 2017 The Midland Metro Alliance is a team of planning, design and construction specialists responsible for building a number of new tram extensions over the coming decade on behalf of the West Midlands Combined Authority. These exciting extensions will help deliver a lasting legacy, aiding social and economic regeneration across the region. Building on lessons from past projects and best practice from across the world, Midland Metro Alliance has goals which will ensure the 10 year plan will only be successfully delivered if all parties work together. This will give the best outcome for the travelling public and the local economy. ~,WEST MIDLAo DS TfW M WEST MIDLANDS `~ ♦-~- - -~-~-~ COMBINED AUTHORITY FOREWORD BY ANDY STREET — MAYOR FOR THE WEST MIDLANDS As the newly elected Mayor for the West Midlands, I am delighted to submit to you this Business Case for the Wednesbury to Brierley Hill Extension of the Midland Metro. One of my key manifesto promises was to start work on this extension within my first term, and this important first step, seeking to obtain the funding and approvals from Central Government, is one that ~I am proud to take within my first month as Mayor. NDS This route will be a key part of the tram network across the region, ■ ~ which will play a significant role in the regeneration and economic growth for the West Midlands. Our patronage on the existing service between Birmingham and Wolverhampton city centres is at an all-time high — 7.89 million passengers took the tram between June 2016 and May 2017. -

Sandwell Adult and Family Learning January 2017 Course Guide
Sandwell Adult and Family Learning January 2017 Course Guide something for everyone Tel: 0121 557 0837 www.learnsafl.ac.uk [email protected] 1 Why choose us for your education? We offer an adult learning experience, focusing on your personal needs and abilities. Whether you want to improve your: English or maths employment skills or start a new hobby improve your health and well-being help your children with their homework. Sandwell adult and family learning can help you! Learn with us for: small class sizes welcoming atmosphere personal learning and development plans for your future catering for all adults in and out of work face to face support. Information, Advice & Guidance Sessions We can help you: make important decisions about your future develop new skills find training for work make the most of workplace opportunities look at career options information about childcare Learn with us and CV writing you can apply for a NUS Extra Student job interview skills Discount Card. This provide information about learning opportunities enables you to get a help you gain a qualification. discount at a range of stores, restaurants and more. We ensure that the information we provide is impartial and confidential Fees and Concessions All of our courses are funded by the Skills Funding Agency which provides a subsidy towards the actual cost. It is therefore expected that where learners are able to pay a contribution towards their courses, they should do so. For the academic year 2016 - 2017, the following fee discounts/concessions will apply: Employability/English/maths courses are free of charge Level 2 and below. -

Appendix 1 Council Leisure and Culture Facilities in Sandwell
Appendix 1 Council Leisure and Culture Facilities in Sandwell Please note that this list does not include sports facilities and swimming pools. These have already been the subject of a review by the Select Committee for Leisure Provision since 2016. Oldbury Name Type of facility Ward Bleakhouse Library Library Bristnall Brandhall Library Library Old Warley Langley Library Library Langley Oldbury Library Library Oldbury Rounds Green Library Library Langley Hurst Road Community Centre Bristnall Community Centre Langley Lodge Community Centre Langley Community Centre Barnford Park Park Langley Tividale Park Park Oldbury Langley Park Park Langley Broadwell Park Park Langley Bury Hill Park Park Langley Rowley Regis Name Type of facility Ward Blackheath Library Library Blackheath Cradley Heath Library Library Cradley Heath and Old Hill Oakham Library Library Tividale Haden Hill House Historic Building and Cradley Heath and Museum Museum Old Hill Brickhouse Community Centre Rowley Community Centre Cradley Heath Community Centre Rowley Community Centre Haden Hill Park Park Cradley Heath and Old Hill Britannia Park Park Blackheath Mary MacArthur Park Cradley Heath and Gardens Old Hill Smethwick Name Type of facility Ward Smethwick Library Library Smethwick Thimblemill Library Library Abbey Community History Archives (local Smethwick and Archive Service history) (CHAS) Galton Valley Historic Building and St Paul’s Pumping Station Museum Lightwoods Park Park Abbey Victoria Park Park Soho and Victoria Warley Woods Park Abbey West Smethwick Park Park -

Magazine | a BETTER LIFE for OVER 50S
Winter/Spring 2016 Agewell Magazine | A BETTER LIFE FOR OVER 50s Sponsored by: Agewell Magazine Inside this issue: There are now 11 Community Offers for older people up and running across Sandwell Special feature on pages 6-10 Also inside: Make volunteering your resolution this year | Page 3 Community policing concerns tackled head on | Page 4 Goodwill shop promises treasures for all | Page 5 News round-up | Page 11 Agewell www.agewelluk.org.ukPage 1 Magazine WELCOME Welcome to the Winter/Spring issue which is sponsored by Sandwell Council’s Community Offer. Greenwood, the Volunteer Lead for Sandwell and West Birmingham Hospitals NHS Trust’s Mi Volunteers service in the new Agewell Community Shop, which will sell a range of items including newspapers, sandwiches and snacks. Agewell staff and volunteers will also be reinstating the popular trolley–round to all wards. Look out for us in our purple T-shirts! We are very excited to have a permanent presence within the hospital which will build on the valuable hospital to home befriending, advocacy and support It’s over 12 months since Sandwell Council’s first service (known as Edna’s Army) already provided by Community Offers for older people went live. On Agewell. Do pop in and say hello. We are interested the centre pages we’ve featured some of the to hear what items you would like to see on sale in important work that we and our Community Offer the Hospital Shop. partners have been undertaking to help improve Before I finish, I’d like to officially the health and wellbeing of local older people. -

Social Work in Austerity, Public Health and Economy Dr John Middleton
Social work in austerity, public health and economy Dr John Middleton Director of Public Health Sandwell • Harvey Brenner Int Journal Epidemiology • 2005, 34, 6: 1214 Reality very different And the peculiar evil is, the less money you have , the less inclined you feel to spend it on wholesome food. A millionnaire may enjoy breakfasting on orange juice and Ryvita biscuits; an unemployed man doesn’t When you are unemployed, which is to say when you are underfed, harassed,bored, and miserable you don’t want to eat dull wholesome food…… George Orwell, The Road To Wigan pier. 11 Recession and policy changes Health impacts of economic downturn • Widening health inequalities • Worse mental health –including depression, and possibly lower levels of wellbeing • More suicides and attempted suicides; • Possibly more homicides and domestic violence • Fewer road traffic fatalities • Worse infectious disease outcomes such as tuberculosis and HIV Source: The poverty site http://www.poverty.org.uk/09/index.shtml The Marmot Review • The best evidence for what we need to do • The biggest influences on health & wellbeing are the ‘social determinants’ of health • The ability to influence these sits largely with the local authority 14 Life expectancy & disability free life expectancy at birth, by neighbourhood income level, England and Sandwell 1999-2003 Age Neighbourhoods by income deprivation (population 15 percentiles) Housing benefit reductions by Wednesbury North Friar Park Great Barr ward – under- with Yew Tree Charlemont with Grove Vale occupying Princes -

Demolished Properties
Press 'Ctrl F' to search information COUNCIL OR POST PROPERTY NAME OR DATE OF STREET TOWN DESCRIPTION PRIVATE CODE NUMBER DEMOLITION DEMOLITION Surrey Crescent West Bromwich Garages Garages Private 26-Mar-15 The Sandwell and West Grove Lane Smethwick B66 2QT Birmingham NHS Trust Plot 33 & NHS Property Council 20-Mar-15 34 Charles Street West Bromwich B70 0FD Waterside House Offices Private 4-Mar-15 Trinity Street Oldbury B69 4LN Sub Station at Solvay Private 24-Feb-15 St Matthews CE Primary School Windmill Lane Smethwick B66 3LX School Council 20-Feb-15 Caretakers House Oldbury Ringway Oldbury B69 4JW Arnold Clark Private 11-Feb-15 Cranford Street Smethwick B66 2RX Atlas House Commercial Private 11-Feb-15 Apsley Road Oldbury B68 0QY Perryfields Primary School School Private 10-Feb-15 Crosswells Road Oldbury B68 8HA Alcohols Limited, The Distillery Commercial Private 19-Jan-15 Carters Green West Bromwich B70 9LG 38, YMCA John Lees House Private 16-Jan-15 Throne Road Rowley Regis B65 9LD St Michaels CE High School School Private 6-Jan-15 Gerry Simon Clinic, Heath Lane Heath Lane West Bromwich B71 2BG NHS Property Private 4-Dec-14 Hospital Great Bridge Street West Bromwich B70 0DA 65-91 Private 20-Nov-14 Groveland Road Tipton DY4 7TB Commercial Body Fittings Limited Commercial Private 20-Nov-14 Crankhall Lane Wednesbury WS10 0EB 158 Friar Park Chemist Commercial Private 20-Nov-14 Whitehall Road Tipton DY4 7JU IBP Conex Limited Industrial Private 19-Nov-14 Wrights Lane Cradley Heath B64 6QY 41 Prince of Wales PH Public House Private 19-Nov-14 -
Claimant Count Summary for April 2020: Released May 20201
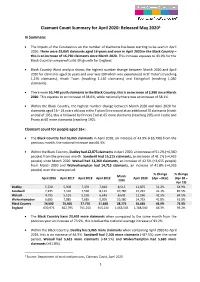
Claimant Count Summary for April 2020: Released May 20201 In Summary: • The impact of the Coronavirus on the number of claimants has been starting to be seen in April 2020. There were 55,065 claimants aged 16 years and over in April 2020 in the Black Country – this is an increase of 16,790 claimants since March 2020. This increase equates to 43.9% for the Black Country compared to 66.3% growth for England. • Black Country Ward analysis shows the highest number change between March 2020 and April 2020 for claimants aged 16 years and over was 290 which was experienced in St’ Peter’s (reaching 1,270 claimants), Heath Town (reaching 1,140 claimants) and Ettingshall (reaching 1,080 claimants). • There were 10,740 youth claimants in the Black Country, this is an increase of 2,990 since March 2020. This equates to an increase of 38.6%, while nationally there was an increase of 58.1%. • Within the Black Country, the highest number change between March 2020 and April 2020 for claimants aged 16 – 24 years old was in the Tipton Green ward at an additional 70 claimants (reach a total of 195), this is followed by Princes End at 65 more claimants (reaching 205) and Castle and Priory at 60 more claimants (reaching 190). Claimant count for people aged 16+: • The Black Country had 55,065 claimants in April 2020, an increase of 43.9% (+16,790) from the previous month, the national increase was 66.3%. • Within the Black Country, Dudley had 12,875 claimants in April 2020, an increase of 51.2% (+4,360 people) from the previous month. -

Character Appraisal Study and Boundary Review of the Factory Locks Conservation Area, Tipton
Character Appraisal Study and Boundary Review of the Factory Locks Conservation Area, Tipton Prepared for Sandwell Metropolitan Borough Council By Sandwell Historic Environment Team and Birmingham Archaeology Heritage Services 2008 Character Appraisal Study and Boundary Review of the Factory Locks Conservation Area, Tipton CONTENTS 1.0 INTRODUCTION 2.0 PLANNING POLICY CONTEXT 3.0 LOCATION AND SETTING 3.1 Location and Context 3.2 General Character and Plan Form 3.3 Landscape Setting 4.0 HISTORIC DEVELOPMENT AND ARCHAEOLOGY 4.1 The Origins and Historic Development of the Area 4.2 The Factory Locks Conservation Area 4.3 The Morphology of the Area 4.4 Archaeology 5.0 SPATIAL ANALYSIS 5.1 The Character and Interrelationship of Spaces within the Area 5.2 Key Views and Vistas 6.0 CHARACTER ANALYSIS 6.1 Defi nition of the Character Areas (Zones) 6.2 Activity within the Area, and its Infl uences 6.3 Architectural and Historic Qualities of the Buildings 6.4 The Contribution of Key Unlisted Buildings 6.5 Local Details 6.6 Prevalent and Traditional Building Materials 6.7 Audit of Heritage Assets 6.8 Contribution made by Greenery and Green Spaces 6.9 Negative Factors 6.10 Neutral Areas 6.11 General Condition 6.12 Problems, Pressures and Capacity for Change 7.0 SUGGESTED BOUNDARY CHANGES 8.0 LOCAL GENERIC GUIDANCE 8.1 Opportunities for Enhancement 8.2 Planning Policy and Guidance 8.3 Protection, Restoration and Enhancement 8.4 Potential HERS and THI Projects 8.5 Research Strategy for Archaeological Evaluation and Historic Building Recording APPENDICES 1 Audit of Heritage Assets 2 SMR Summary Sheet ILLUSTRATIONS Maps 1. -

INSPECTION REPORT TIPTON GREEN JUNIOR SCHOOL Tipton
INSPECTION REPORT TIPTON GREEN JUNIOR SCHOOL Tipton LEA area: Sandwell Unique reference number: 103928 Headteacher: Mr L Rouse Reporting inspector: Barbara Crane 21227 Dates of inspection: 14th – 18th January 2002 Inspection number: 194461 Full inspection carried out under section 10 of the School Inspections Act 1996 © Crown copyright 2002 This report may be reproduced in whole or in part for non-commercial educational purposes, provided that all extracts quoted are reproduced verbatim without adaptation and on condition that the source and date thereof are stated. Further copies of this report are obtainable from the school. Under the School Inspections Act 1996, the school must provide a copy of this report and/or its summary free of charge to certain categories of people. A charge not exceeding the full cost of reproduction may be made for any other copies supplied. INFORMATION ABOUT THE SCHOOL Type of school: Junior School category: Community Age range of pupils: 7 – 11 Gender of pupils: Mixed School address: Park Lane West Tipton Sandwell West Midlands Postcode: DY4 8LE Telephone number: 0120 5579242 Fax number: 0121 5202393 Appropriate authority: Governing body Name of chair of governors: Mr Keith Aston Date of previous inspection: March 1997 Tipton Green Junior School - 3 INFORMATION ABOUT THE INSPECTION TEAM Team members Subject Aspect responsibilities responsibilities 21227 Barbara Crane Registered English, information and The school’s results and inspector communication achievements. technology, art, design How well are pupils taught? and technology, physical education, special How well is the school led educational needs. and managed? What should the school do to improve further? 19430 Trevor Hall Lay inspector Pupils’ attitudes, values and personal development. -

Register of Charles Wesley's Preaching
Page 1 -- 1735-36 Register of Charles Wesley’s Preaching [updated April 24, 2021] Date / Day Text [or topic] Site Source 10/21/35 T Phil. 3:13–14 On board the “Simmonds,” bound for Georgia CW notation1 11/30/35 S 1 Kgs. 18:21 Cowes, Isle of Wight, St. Mary’s church CW notation2 [12/07/35 S] John 4:41 Cowes, Isle of Wight, St. Mary’s church CW title3 03/09/36 T arrives at Frederica, begins leading regularly in prayers 03/11/36 Th Luke 224 Frederica, Georgia MS Journal 03/14/36 S Matt. 6:22–235 Frederica, Georgia MS Journal; CW notation 04/04/36 S Ps. 37:37 Frederica, Georgia MS Journal 04/18/36 S Ps. 126:7 (BCP)6 Frederica, Georgia MS Journal 05/09/36 S Luke 16:87 Frederica, Georgia CW notation 05/11/36 T [2 Kgs. 4; Matt. 9]8 Frederica, Georgia MS Journal 05/12/36 W Matt. 10:16–269 Frederica, Georgia MS Journal 05/13/36 Th leaves for Savannah 05/16/36 S not specified Skidaway Island, Georgia MS Journal 05/19/36ff [lesson am & pm]10 Savannah, Georgia MS Journal 05/23/36 S Matt. 6:22–23 Savannah, Georgia CW notation11 1A manuscript text of this sermon has survived, including a notation of when it was preached (MARC, MA 1977/597/1). A published transcription is available in Sermons, 95–106. 2A manuscript text of this sermon has survived, including a notation of being preached this time (MARC, MA 1977/597/4).