Afghan Nomads' Perceptions of Diarrhea
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mohmad Agency Blockwise
POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL FATA (MOHMAND AGENCY) ADMIN UNIT POPULATION NO OF HH MOHMAND AGENCY 466,984 48,118 AMBAR UTMAN KHEL TEHSIL 62,109 6,799 AMBAR UTMAN KHEL TRIBE 62,109 6799 BAZEED KOR SECTION 21,174 2428 BAHADAR KOR 4,794 488 082050106 695 50 082050107 515 54 082050108 256 33 082050109 643 65 082050110 226 35 082050111 326 39 082050112 425 55 082050113 837 64 082050114 192 24 082050115 679 69 BAZID KOR 8,226 943 082050116 689 71 082050117 979 80 082050118 469 45 082050119 1,062 128 082050120 1,107 145 082050121 655 72 082050122 845 123 082050123 1,094 111 082050124 455 60 082050125 871 108 ISA KOR 3,859 490 082050126 753 93 082050127 1,028 104 082050128 947 118 082050129 715 106 082050130 416 69 KOT MAINGAN 673 79 082050105 673 79 WALI BEG 3,622 428 082050101 401 49 082050102 690 71 082050103 1,414 157 082050104 1,117 151 MAIN GAN SECTION 40,935 4371 AKU KOR 5,478 583 082050223 1,304 117 082050224 154 32 082050225 490 41 082050226 413 40 082050227 1,129 106 082050228 1,988 247 BANE KOR 8,626 1012 Page 1 of 12 POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL FATA (MOHMAND AGENCY) ADMIN UNIT POPULATION NO OF HH 082050214 1,208 121 082050215 1,363 141 082050216 672 67 082050217 901 99 082050218 1,117 175 082050219 1,507 174 082050220 448 76 082050221 839 79 082050222 571 80 KHORWANDE 1,907 184 082050229 1,714 159 082050230 193 25 MAIN GAN 11,832 1182 082050201 1,209 114 082050202 1,105 124 082050203 1,322 128 082050204 1,387 138 082050205 1,043 75 082050206 774 71 082050207 763 75 082050208 -

The Kingdom of Afghanistan: a Historical Sketch George Passman Tate
University of Nebraska Omaha DigitalCommons@UNO Books in English Digitized Books 1-1-1911 The kingdom of Afghanistan: a historical sketch George Passman Tate Follow this and additional works at: http://digitalcommons.unomaha.edu/afghanuno Part of the History Commons, and the International and Area Studies Commons Recommended Citation Tate, George Passman The kingdom of Afghanistan: a historical sketch, with an introductory note by Sir Henry Mortimer Durand. Bombay: "Times of India" Offices, 1911. 224 p., maps This Monograph is brought to you for free and open access by the Digitized Books at DigitalCommons@UNO. It has been accepted for inclusion in Books in English by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. Tate, G,P. The kfn&ean sf Af&mistan, DATE DUE I Mil 7 (7'8 DEDICATED, BY PERMISSION, HIS EXCELLENCY BARON HARDINGE OF PENSHURST. VICEROY AND GOVERNOR-GENERAL OF INDIA, .a- . (/. BY m HIS OBEDIENT, SERVANT THE AUTHOR. il.IEmtev 01 the Asiniic Society, Be?zg-nl, S?~rueyof I~din. dafhor of 'I Seisinqz : A Menzoir on the FJisio~y,Topo~rcrphj~, A7zliquiiies, (112d Peo$Ie of the Cozi?zt~y''; The F/.o?zlic7,.~ of Baluchisia'nn : Travels on ihe Border.? of Pe~szk n?zd Akhnnistnn " ; " ICalnf : A lMe??zoir on t7ze Cozl7~try and Fnrrzily of the Ahntadsai Khn7zs of Iinlnt" ; 4 ec. \ViTkI AN INrPR<dl>kJCTOl2Y NO'FE PRINTED BY BENNETT COLEMAN & Co., Xc. PUBLISHED AT THE " TIMES OF INDIA" OFFTCES, BOMBAY & C.1LCUTT-4, LONDON AGENCY : gg, SI-IOE LANE, E.C. -

AFGHANISTAN and PAKISTAN the New Parliament: an Afghan Way to Democracy Fausto Biloslavo 37 Military Center for Strategic Studies
Q UARTERLY NORTH AFRICA – MIDDLE EAST –PERSIAN GULF YEAR IV SPRING 2006 Four Scenarios After Hamas' Victory Hillel Frisch 5 SOUTH EASTERN EUROPE First Quarter Balkan review: trends and evolutions in the region Centro Militare Paolo Quercia 13 di Studi Strategici COMMONWEALTH OF INDEPENDENT STATES EASTERN EUROPE CeMiSS Quarterly is a review The rising confrontation between Russia and the West supervised by CeMiSS director, Rear Andrea Grazioso 17 Admiral Luciano Callini. It provides a forum to promote the THE TRANSATLANTIC RELATIONS knowledge and understanding of Towards an October Surprise, via Teheran? international security affairs, military Lucio Martino 23 strategy and other topics of significant interest. THE ASIAN PLAYERS: INDIA AND CHINA The opinions and conclusions Find the enemy: China naval strategy and the EU Galileo Project expressed in the articles are those of Nunziante Mastrolia 29 the contributors and do not necessarily reflect the position of the Italian Ministry of Defence. AFGHANISTAN AND PAKISTAN The new parliament: an Afghan way to democracy Fausto Biloslavo 37 Military Center for Strategic Studies External Relations Office Palazzo Salviati LATIN AMERICA Piazza della Rovere, 83 00165 – Free Trade Agreements vs. Nationalizations ROME - ITALY United States’ and Venezuela’s confronting influence in Latin tel. 00 39 06 4691 3207 America fax 00 39 06 6879779 Riccardo Gefter Wondrich 59 e-mail [email protected] Quarterly Year IV N°2 - April 2006 North Africa Middle East Persian Gulf FOUR SCENARIOS AFTER HAMAS' VICTORY Hillel Frisch Elections to the Palestinian Legislative Council raised hopes of bringing the classic spoiler Hamas into negotiations, restart a peace process moribund since September 2000 and to set the Palestinians on a peaceful democratic trajectory. -

Tehrik-E-Taliban Pakistan
DIIS REPORT 2010:12 DIIS REPORT TEHRIK-E-TALIBAN PAKISTAN AN ATTEMPT TO DECONSTRUCT THE UMBRELLA ORGANIZATION AND THE REASONS FOR ITS GROWTH IN PAKISTAN’S NORTH-WEST Qandeel Siddique DIIS REPORT 2010:12 DIIS REPORT DIIS . DANISH INSTITUTE FOR INTERNATIONAL STUDIES 1 DIIS REPORT 2010:12 © Copenhagen 2010, Qandeel Siddique and DIIS Danish Institute for International Studies, DIIS Strandgade 56, DK-1401 Copenhagen, Denmark Ph: +45 32 69 87 87 Fax: +45 32 69 87 00 E-mail: [email protected] Web: www.diis.dk Cover photo: Pakistani Taliban chief Hakimullah Mehsud promising future attacks on major U.S. cities and claiming responsibility for the attempted car bombing on Times Square, New York (AP Photo/IntelCenter) Cover: Anine Kristensen Layout: Allan Lind Jørgensen Printed in Denmark by Vesterkopi AS ISBN 978-87-7605-419-9 Price: DKK 50.00 (VAT included) DIIS publications can be downloaded free of charge from www.diis.dk Hardcopies can be ordered at www.diis.dk Qandeel Siddique, MSc, Research Assistant, DIIS www.diis.dk/qsi 2 DIIS REPORT 2010:12 Contents Executive Summary 4 Acronyms 6 1. TTP Organization 7 2. TTP Background 14 3. TTP Ideology 20 4. Militant Map 29 4.1 The Waziristans 30 4.2 Bajaur 35 4.3 Mohmand Agency 36 4.4 Middle Agencies: Kurram, Khyber and Orakzai 36 4.5 Swat valley and Darra Adamkhel 39 4.6 Punjab and Sind 43 5. Child Recruitment, Media Propaganda 45 6. Financial Sources 52 7. Reasons for TTP Support and FATA and Swat 57 8. Conclusion 69 Appendix A. -
47281-001: National Highway Network Development in Balochistan Project
National Highway Network Development in Balochistan Project (RRP PAK 47281) Resettlement Plan May 2014 PAK: National Highway Network Development in Balochistan Project Widening and Improvement Project of N-50 Road Zhob-Mughalkot Section (81 km) Prepared by Environment, Afforestation, Land and Social Wing (EALS), National Highway Authority and Ministry of Communications, Government of Pakistan; for the Asian Development Bank. This resettlement plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Contents DEFINITIONS OF TERMS ........................................................................................................... i EXECUTIVE SUMMARY ........................................................................................................... iv Chapter 1 INTRODUCTION ............................................................................................ 1 1.1. Project Background ....................................................................................................... 1 1.2. Project Description ....................................................................................................... -

The Musalman Races Found in Sindh
A SHORT SKETCH, HISTORICAL AND TRADITIONAL, OF THE MUSALMAN RACES FOUND IN SINDH, BALUCHISTAN AND AFGHANISTAN, THEIR GENEALOGICAL SUB-DIVISIONS AND SEPTS, TOGETHER WITH AN ETHNOLOGICAL AND ETHNOGRAPHICAL ACCOUNT, BY SHEIKH SADIK ALÍ SHER ALÍ, ANSÀRI, DEPUTY COLLECTOR IN SINDH. PRINTED AT THE COMMISSIONER’S PRESS. 1901. Reproduced By SANI HUSSAIN PANHWAR September 2010; The Musalman Races; Copyright © www.panhwar.com 1 DEDICATION. To ROBERT GILES, Esquire, MA., OLE., Commissioner in Sindh, This Volume is dedicated, As a humble token of the most sincere feelings of esteem for his private worth and public services, And his most kind and liberal treatment OF THE MUSALMAN LANDHOLDERS IN THE PROVINCE OF SINDH, ВY HIS OLD SUBORDINATE, THE COMPILER. The Musalman Races; Copyright © www.panhwar.com 2 PREFACE. In 1889, while I was Deputy Collector in the Frontier District of Upper Sindh, I was desired by B. Giles, Esquire, then Deputy Commissioner of that district, to prepare a Note on the Baloch and Birahoi tribes, showing their tribal connections and the feuds existing between their various branches, and other details. Accordingly, I prepared a Note on these two tribes and submitted it to him in May 1890. The Note was revised by me at the direction of C. E. S. Steele, Esquire, when he became Deputy Commissioner of the above district, and a copy of it was furnished to him. It was revised a third time in August 1895, and a copy was submitted to H. C. Mules, Esquire, after he took charge of the district, and at my request the revised Note was printed at the Commissioner-in-Sindh’s Press in 1896, and copies of it were supplied to all the District and Divisional officers. -

Clans, Tribes and Their Locality in Chechnya, Albania, Afghanistan and Iraq
Appendix Clans, Tribes and Their Locality in Chechnya, Albania, Afghanistan and Iraq While compiling the lists with clans the author found that in some cases lists do not (completely) overlap. Since the sources are trustworthy, they are indicated here. This shows the importance of correct knowledge of clans and their influence in the areas they are inhabiting. 1 Clans in Chechnya1 Confederation Clans Localisation A’kkhiï Bartchakhoï, J’evoï, Ziogoï, In the east of Chechnya, Pkhiartchoï, Pkhiartchakhoï, near Daghestan; North of Nokkhoï, Va’ppiï Daghestan Malkhiï Amkhoï, Bia’stiï, Bienastkhoï, In the south west of Italtchkhoï, Kamalkhoï, Chechnya, along the frontier Kkhoratkhoï, Kiegankhoï, with Ingushetia and Georgia Mechiï, Sakankhoï, Teratkhoï, Tchiarkhoï, Erkhoï, Yamkhoï Nokhtchmakhkoï Aïtkhaloï, Belguiatoï, Benoï, East, Southeast and part of Biltoï, Guandarguenoï, central Chechnya Guiordaloï, Gouonoï, Zandak’oï, Ikhiiroï, Ichkhoï, Kourchaloï, Sessankhoï, Tchermoï, Tsientaroï, Tchartoï, Eguiachbatoï, Enakkhaloï, Enganoï, Chouonoï, Yalkhoï, Yaliroï Terloï Nik’aroï, O’chniï, Cho’ndiï, Along the Tchanty-Argun Eltpkh’arkhoï 1 M.A. Mamakaev. Le taipe (lignee) tchétchène dans la période de sa désintégration (Grozny: Maison d’édition tchétchéno-ingouche, 1973), 18–19 in Viacheslav Avioutskii, 54. © koninklijke brill nv, leiden, ���� | doi:10.1163/9789004415485_013 Charlotte Hille - 9789004415485 Downloaded from Brill.com09/30/2021 01:32:57AM via free access <UN> �36 APPENDIX: CLANS, TRIBES AND THEIR LOCALITY Confederation Clans Localisation -

Village List of Kurram Agency , Pakistan
M-Int-2 400- I C!llsus 51-No. 30 C (5) I I I I CENSUS OF PAKISTAN, 1951 I I I ' VILLAGE LIST o North West Frontier-Kurram Agency -r-'INCIAL SUPERINTENDENT OF CENSU 5, ~IER PROVINCB-;" , I March 1952 Przce : 2 -,t- PRIN'I'ED E" THE l'vlANAGER, GO".'Fm; ""I .. ";:0:' 0<' I"_'.:,:r:.>TAN PRESS, K<\RACHI PUBLISHFD BY THE MANAGER OF PCBI.IC.-\TIONS, KARACHI: 1953 VILLAGE LIST OF TRIBAL AREAS OF N. W. F. KURRAM AGENCY FOREWORD This Village List is prepared from the Enumeration carried out in the First Census of Pakistan during February 1951. It gives the population of the smaller area!> and thus preserves information which would otherwise be merged in the statistical totals of the Census Report. It is hoped that the preparation of this list will form a basis for the continued collection of Village Statistics. The enumeration in the Tribal Areas was carried out partly on special tribal enu meration slips, and partly by means of estimates prepared by Political Officers. In Kurram Agency, the whole population except members of the Services was enumerated on Tribal Slips. Members of the Services, enumerated on standard All-Pakistan Enumeration forms, are not included in the figures in the Village List but are merged with the figures in the Census Reports of the N.W.F. Province. The Village List is in two parts; first a summary of Kurram Agency and secondly a list of Villages. In both sections the population is analysed according to the tribes as stated by the respond !nts on their Enumeration Slips. -

Kandahar Province
UNHCR BACKGROUND REPORT KANDAHAR PROVINCE Prepared by the Data Collection for Afghan Repatriation Project 1 September 1989 PREFACE 'Ihe following report is one in a series of 14 provincial profiles prepared for the United Nations High Conunissioner for Refugees by the Data Collec tion for Afghan Repatriation Project. 'Ihe object of these reports is to provide detailed inforrration on the conditions affecting the repatriation of Afghan refugees in each pru,rince so that UNHCRand its implementing partners may be better able to plan and target progra:rmnes of relief and rehabilitation assistance. Each of the provinces featured in this series is estimated to have at least 35 percent of its pre-1978 population living as refugees. Together, these 14 provinces -- Baghlan, Farah, Ghazni, Hel.rnand, Herat, Kandahar, Kunar, Iaghman, I.agar, Nangarhar, Nbnroz, Paktia, Paktik.a and Zabul -- account for ninety percent of the Afghan refugee population settled in Iran and Pakistan. 'Ihe Data Collection for Afghan Repatriation Project (DCAR)was funded by UNHCRto develop a databasH of information on Afghanistan that would serve as a resource for repatriation planning. Project staff based in Peshawar and Quetta have conducted .interviews and surveys in refugee camps through out NWFP, Baluchistan and Punjab provinces in Pakistan to compile data on refugee origins, ethnic and tribal affiliation and likely routes of refugee return to Afgha11istan. In addition, the project field staff undertake frequent missions into Afghanistan to gather specific inform ation on road conditions, the availability of storage facilities, trans portation and fuel, the level of destruction of housing, irrigation systems and farmland, the location of landmines and the political and military situation at the district (woleswali)and sub-district (alaqadari) levels in those provinces of priority concern to UNHCR. -

The Quetta Shura: a Tribal Analysis
T HE Q UE tt A S HURA : A T RIBAL A NALY S I S Cultural & Geographic Research TRIBAL ANALYSIS CENTER October 2009 The Quetta Shura: A Tribal Analysis T HE Q UE tt A S HURA : A T RIBAL A NALY S I S Copyright © 2009 Tribal Analysis Center, LTD All Rights Reserved Cultural & Geographic Research TRIBAL ANALYSIS CENTER About Tribal Analysis Center Tribal Analysis Center, 6610-M Mooretown Road, Box 159. Williamsburg, VA, 23188 The Quetta Shura: A Tribal Analysis The Quetta Shura: A Tribal Analysis According to well-established studies, the Taliban’s senior leadership, the Quetta Shura,1 which has significant control over the Taliban’s insurgent operations in southern Afghanistan, seems to have evolved from a Ghilzai Pashtun-led organization during its early years to one that is currently domi- nated by Durrani Pashtuns. The Ghilzai remnants are slim and include Mullah Mohammad Omar,2 a Hotak Ghilzai, and Mullah Muttaqi, reportedly a Taraki Ghilzai, and with the exception of Mullah Mohammad Hassan, probably a Babar, the remaining key Taliban leaders of the insurgency in southern Afghanistan have evolved into a Durrani leadership. This is a very significant change within the early Taliban structure. In a careful review of 20 Taliban political figures who served as either a min- ister or deputy-minister, over half were non-Durrani. More significantly, when the Panjpai Durranis are separated from the group, the Zirak Durranis comprise less than 25 percent of the total. An equally significant number of Taliban military officials were also analyzed to show that approximately 33 percent were Durranis, but this group has only one Zirak Durrani.3 Using this as a baseline study, the tribal composition of the current Taliban leadership is even more significant, if not astonishing. -
Pishin Blockwise
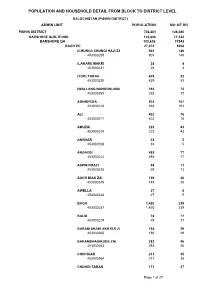
POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL BALOCHISTAN (PISHIN DISTRICT) ADMIN UNIT POPULATION NO OF HH PISHIN DISTRICT 736,481 128,080 BARSHORE SUB-TEHSIL 103,606 17,343 BARSHORE QH 103,606 17343 BAGH PC 27,874 5008 (CHUNGI) CHUNGI HAJI ZAI 901 146 453030235 901 146 (LAKARI) MAKRI 28 4 453030231 28 4 (TOR) TORAH 429 53 453030230 429 53 (WALLANG NANOON) NANOON 353 72 453030250 353 72 AGHBERGA 834 161 453030216 834 161 ALI 402 76 453030217 402 76 AMUZAI 223 43 453030220 223 43 ANGHAR 33 5 453030208 33 5 ANZARGI 485 77 453030224 485 77 ASPIN KHAZI 69 13 453030225 69 13 AUCH BIAN ZAI 149 26 453030245 149 26 AWELLA 27 5 453030248 27 5 BAGH 1,420 239 453030237 1,420 239 BALIK 78 17 453030219 78 17 BARAM SHAHI AKHTER ZAI 186 29 453030265 186 29 BARAMSHAUIKUDE ZAI 283 46 453030263 283 46 CHICHGAR 211 35 453030264 211 35 CHUNGI TARAN 171 37 Page 1 of 27 POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL BALOCHISTAN (PISHIN DISTRICT) ADMIN UNIT POPULATION NO OF HH 453030232 171 37 DARA 73 19 453030257 73 19 DARASOOR 338 50 453030256 338 50 EZAH 503 93 453030253 503 93 GARANGI 62 13 453030269 62 13 GHANZA 802 139 453030241 802 139 GHEZAH 544 106 453030203 544 106 GUT 59 11 453030268 59 11 HOT 796 142 453030218 796 142 HUMAI 17 2 453030226 17 2 ISSA ZAI 314 43 453030206 314 43 KACHH HASSAN ZAI 806 159 453030215 806 159 KAZHA BAIN 20 2 453030221 20 2 KHAR 36 7 453030228 36 7 KHUSHKABA POTIAN 162 25 453030211 162 25 KHUSOI 364 59 453030209 364 59 KOZ HUBU CHINA 290 44 453030229 290 44 KUTT 907 148 453030204 907 148 LAKKER -

Shinwari Tribe
Program for Culture & Conflict Studies [email protected] Shinwari Tribe Shinwari Notes: The Shinwari are Eastern Sarbani Pashtuns located in eastern Afghanistan and the Khyber region of Pakistan. Their nomadic brethren are Shinwari Powindah. (Click Blue box to continue to next segment.) (Click Blue box to continue to next segment.) Manduzai / Mandu / Sangu Khel / Sipai / Sehpai / Alisher Khel Mullagori Mandhi Zai Sangukhel Sipai Reference: Courage Services Inc., Tribal Hierarchy & Dictionary of Afghanistan: A Reference Aid for Analysts, 1 (February 2007). Program for Culture & Conflict Studies [email protected] Alisher Khel Descendant of Shinwari Tribe Alisher Khel Adil Khel Ash Khel Kuru Khel Usman Khel Alijan Nmasi Kamal Nmasi Shahmad Nmasi De Saruk Kali Khel Khuga Khel Khwaja Khel Alam Khan Nmasi Ashrapai Nmasi Basai Nmasi Fatima Nmasi Kuhai Lohargai Mirdad Khel Otar Khel Ganjun Nmasi Tirai Khel Badia Nmasi Kadir Nmasi Nur Gholam Nmasi Pa Khel / Paya Khel Past Khel Pekha Piro Khel / Peru Khel Mat Khel Shudan Khel Pirwal Khel Piset Khel Rostam Khel Shamu Khel Shaikhai Khel Shekmal Khel Ghani Nmasi Talib Khel Reference: Courage Services Inc., Tribal Hierarchy & Dictionary of Afghanistan: A Reference Aid for Analysts, 2 (February 2007). Program for Culture & Conflict Studies [email protected] Manduzai / Mandu / Mandhi Zai Descendant of Shinwari Tribe Manduzai Hamza Khel Hasan Khel Ilias Khel Ahmad Khel Maghdud Khel Da Oghaz Khel Musi Khel Umar Khel Daulat Khel Kotwal Kuki Khel Reference: Courage Services Inc., Tribal Hierarchy & Dictionary of