Report on Epidemiological Mapping of Schistosomiasis and Soil Transmitted Helminthiasis in 19 States and the FCT, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
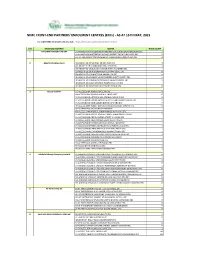
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (Ercs) - AS at 15TH MAY, 2021
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (ERCs) - AS AT 15TH MAY, 2021 For other NIMC enrolment centres, visit: https://nimc.gov.ng/nimc-enrolment-centres/ S/N FRONTEND PARTNER CENTER NODE COUNT 1 AA & MM MASTER FLAG ENT LA-AA AND MM MATSERFLAG AGBABIAKA STR ILOGBO EREMI BADAGRY ERC 1 LA-AA AND MM MATSERFLAG AGUMO MARKET OKOAFO BADAGRY ERC 0 OG-AA AND MM MATSERFLAG BAALE COMPOUND KOFEDOTI LGA ERC 0 2 Abuchi Ed.Ogbuju & Co AB-ABUCHI-ED ST MICHAEL RD ABA ABIA ERC 2 AN-ABUCHI-ED BUILDING MATERIAL OGIDI ERC 2 AN-ABUCHI-ED OGBUJU ZIK AVENUE AWKA ANAMBRA ERC 1 EB-ABUCHI-ED ENUGU BABAKALIKI EXP WAY ISIEKE ERC 0 EN-ABUCHI-ED UDUMA TOWN ANINRI LGA ERC 0 IM-ABUCHI-ED MBAKWE SQUARE ISIOKPO IDEATO NORTH ERC 1 IM-ABUCHI-ED UGBA AFOR OBOHIA RD AHIAZU MBAISE ERC 1 IM-ABUCHI-ED UGBA AMAIFEKE TOWN ORLU LGA ERC 1 IM-ABUCHI-ED UMUNEKE NGOR NGOR OKPALA ERC 0 3 Access Bank Plc DT-ACCESS BANK WARRI SAPELE RD ERC 0 EN-ACCESS BANK GARDEN AVENUE ENUGU ERC 0 FC-ACCESS BANK ADETOKUNBO ADEMOLA WUSE II ERC 0 FC-ACCESS BANK LADOKE AKINTOLA BOULEVARD GARKI II ABUJA ERC 1 FC-ACCESS BANK MOHAMMED BUHARI WAY CBD ERC 0 IM-ACCESS BANK WAAST AVENUE IKENEGBU LAYOUT OWERRI ERC 0 KD-ACCESS BANK KACHIA RD KADUNA ERC 1 KN-ACCESS BANK MURTALA MOHAMMED WAY KANO ERC 1 LA-ACCESS BANK ACCESS TOWERS PRINCE ALABA ONIRU STR ERC 1 LA-ACCESS BANK ADEOLA ODEKU STREET VI LAGOS ERC 1 LA-ACCESS BANK ADETOKUNBO ADEMOLA STR VI ERC 1 LA-ACCESS BANK IKOTUN JUNCTION IKOTUN LAGOS ERC 1 LA-ACCESS BANK ITIRE LAWANSON RD SURULERE LAGOS ERC 1 LA-ACCESS BANK LAGOS ABEOKUTA EXP WAY AGEGE ERC 1 LA-ACCESS -

Report of the Technical Committee Om
REPORT OF THE TECHNICAL COMMITTEE ON CONSTITUTIONAL PROVISIONS FOR THE APPLICATION OF SHARIA IN KATSINA STATE January 2000 Contents: Volume I: Main Report Chapter One: Preliminary Matters Preamble Terms of Reference Modus Operandi Chapter Two: Consideration of Various Sections of the Constitution in Relation to Application of Sharia A. Section 4(6) B. Section 5(2) C. Section 6(2) D. Section 10 E. Section 38 F. Section 275(1) G. Section 277 Chapter Three: Observations and Recommendations 1. General Observations 2. Specific Recommendations 3. General Recommendations Conclusion Appendix A: List of all the Groups, Associations, Institutions and Individuals Contacted by the Committee Volume II: Verbatim Proceedings Zone 1: Funtua: Funtua, Bakori, Danja, Faskari, Dandume and Sabuwa Zone 2: Malumfashi: Malumfashi, Kafur, Kankara and Musawa Zone 3: Dutsin-Ma: Dutsin-Ma, Danmusa, Batsari, Kurfi and Safana Zone 4: Kankia: Kankia, Ingawa, Kusada and Matazu Zone 5: Daura: Daura, Baure, Zango, Mai’adua and Sandamu Zone 6: Mani: Mani, Mashi, Dutsi and Bindawa Zone 7: Katsina: Katsina, Kaita, Rimi, Jibia, Charanchi and Batagarawa 1 Ostien: Sharia Implementation in Northern Nigeria 1999-2006: A Sourcebook: Supplement to Chapter 2 REPORT OF THE TECHNICAL COMMITTEE ON APPLICATION OF SHARIA IN KATSINA STATE VOLUME I: MAIN REPORT CHAPTER ONE Preamble The Committee was inaugurated on the 20th October, 1999 by His Excellency, the Governor of Katsina State, Alhaji Umaru Musa Yar’adua, at the Council Chambers, Government House. In his inaugural address, the Governor gave four point terms of reference to the Committee. He urged members of the Committee to work towards realising the objectives for which the Committee was set up. -

The Cholera Risk Assessment in Kano State, Nigeria: a Historical Review, Mapping of Hotspots and Evaluation of Contextual Factors
PLOS NEGLECTED TROPICAL DISEASES RESEARCH ARTICLE The cholera risk assessment in Kano State, Nigeria: A historical review, mapping of hotspots and evaluation of contextual factors 1 2 2 2 Moise Chi NgwaID *, Chikwe Ihekweazu , Tochi OkworID , Sebastian Yennan , 2 3 4 5 Nanpring Williams , Kelly ElimianID , Nura Yahaya Karaye , Imam Wada BelloID , David A. Sack1 1 Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States of America, 2 Nigeria Centre for Disease Control, Abuja, Nigeria, 3 Department of a1111111111 Microbiology, University of Benin, Nigeria, 4 Department of Public Health and Disease Control, Kano State a1111111111 Ministry of Health, Kano, Nigeria, 5 Department of Public Health and Disease Control, Ministry of Health a1111111111 Kano, Kano, Nigeria a1111111111 a1111111111 * [email protected] Abstract OPEN ACCESS Nigeria is endemic for cholera since 1970, and Kano State report outbreaks annually with Citation: Ngwa MC, Ihekweazu C, Okwor T, Yennan high case fatality ratios ranging from 4.98%/2010 to 5.10%/2018 over the last decade. How- S, Williams N, Elimian K, et al. (2021) The cholera ever, interventions focused on cholera prevention and control have been hampered by a risk assessment in Kano State, Nigeria: A historical lack of understanding of hotspot Local Government Areas (LGAs) that trigger and sustain review, mapping of hotspots and evaluation of contextual factors. PLoS Negl Trop Dis 15(1): yearly outbreaks. The goal of this study was to identify and categorize cholera hotspots in e0009046. https://doi.org/10.1371/journal. Kano State to inform a national plan for disease control and elimination in the State. -

Nigeria Centre for Disease Control Protecting the Health of Nigerians
Nigeria Centre for Disease Control Protecting the health of Nigerians Cholera hotspots mapping in Nigeria Iliya Cheshi - NCDC [email protected] Profile: Nigeria • Nigeria is a federal republic comprising 36 states and the Federal Capital Territory, Abuja • Inhabited by more than 250 ethnic groups with over 500 distinct languages • Nigeria is divided roughly in half between Christians and Muslims 195.9 million (2018) Census 2 NIGERIA CENTRE FOR DISEASE CONTROL Introduction • Cholera remains a global public health problem, disproportionately affecting the tropical and sub-tropical areas of the world, where focal areas or hotspots play a key role in perpetuating the disease transmission • Targeting these hotspots with proven interventions e.g. Water, Sanitation and Hygiene (WaSH), as well as Oral Cholera Vaccines (OCV) could reduce the mean annual incidence of the entire sub-Saharan African region by half (Lessler et al) • The Global Task Force on Cholera Control (GTFCC) has thus advocated for a comprehensive cholera control strategy where the use of OCV plays a complementary role to other preventive interventions, chiefly, ensuring access to WaSH 3 NIGERIA CENTRE FOR DISEASE CONTROL • To align its cholera control strategies with the global road map of the GTFCC, the team at the Nigeria Centre for Disease Control (NCDC) released a document detailing their preparedness and response plans • Assessing cholera transmission dynamics in Nigeria and identifying cholera hotspots were outlined as immediate-term goals. This help to design and implement relevant long term and cost effective solutions to achieve the ultimate goal of cholera elimination 4 NIGERIA CENTRE FOR DISEASE CONTROL Cholera hotspot mapping in Nigeria “Cholera hotspot” is defined as a geographically limited area (e.g. -

2021-2022 Entrance Examination Result.Xlsx
OSUN STATE COLLEGE OF HEALTH TECHNOLOGY, ILESA. 2021/2022 ENTRANCE EXAMINATION RESULT PROFESSIONAL DIPLOMA IN HEALTH INFORMATION MANAGEMENT S/N Reg Nos Name Sex Age State Local Government Courses Total 1 APP3819 OGUNLUMADE TOMILOLA DEBORAH Female 19 Osun Atakunmosa West Professional Diploma in Health Information Mgt.70 2 APP1585 TAIWO GRACE DEBORAH Female 16 Osun Iwo Professional Diploma in Health Information Mgt.70 3 APP0492 ALADOKUN ABOSEDE MARY Female 25 Osun Ifelodun Professional Diploma in Health Information Mgt.67 4 APP3123 AKINYODE OLUWATIMIL?YIN JANET Female 20 Osun Iwo Professional Diploma in Health Information Mgt.65 5 APP3459 MOHAMMED SHIFAU OLAYINKA Female 22 Osun Osogbo Professional Diploma in Health Information Mgt.65 6 APP3736 OLOWOOKERE FERANMI FAITH Female 18 Osun Atakunmosa West Professional Diploma in Health Information Mgt.65 7 APP3621 ADEBUSOYE OMOLARA MAR Y Female 21 Ondo Others Professional Diploma in Health Information Mgt.64 8 APP1319 OLUWOLE CECILIA OPEYEMI Female 21 Osun Odo Otin Professional Diploma in Health Information Mgt.63 9 APP1165 ADEWUYI ESTHER JESUPEMI Female 19 Osun Ilesa West Professional Diploma in Health Information Mgt.62 10 APP2482 AFOLABI ABISOLA RUKAYAT Female 19 Osun Ede South Professional Diploma in Health Information Mgt.62 11 APP3082 AREGBESOLA MOTUNRAYO SOBURAH Female 19 Ondo Others Professional Diploma in Health Information Mgt.62 12 APP1270 OKUNLOLA BLESSING GRACE Female 20 Osun Boripe Professional Diploma in Health Information Mgt.62 13 APP2527 MAKINDE TITILAYO MARY Female 25 Osun Ilesa -

Violence in Nigeria's North West
Violence in Nigeria’s North West: Rolling Back the Mayhem Africa Report N°288 | 18 May 2020 Headquarters International Crisis Group Avenue Louise 235 • 1050 Brussels, Belgium Tel: +32 2 502 90 38 • Fax: +32 2 502 50 38 [email protected] Preventing War. Shaping Peace. Table of Contents Executive Summary ................................................................................................................... i I. Introduction ..................................................................................................................... 1 II. Community Conflicts, Criminal Gangs and Jihadists ...................................................... 5 A. Farmers and Vigilantes versus Herders and Bandits ................................................ 6 B. Criminal Violence ...................................................................................................... 9 C. Jihadist Violence ........................................................................................................ 11 III. Effects of Violence ............................................................................................................ 15 A. Humanitarian and Social Impact .............................................................................. 15 B. Economic Impact ....................................................................................................... 16 C. Impact on Overall National Security ......................................................................... 17 IV. ISWAP, the North West and -

IOM Nigeria DTM Flash Report NCNW 37 (31 January 2021)
FLASH REPORT #37: POPULATION DISPLACEMENT DTM North West/North Central Nigeria Nigeria 25 - 31 JANUARY 2021 Casualties: Movement Trigger: 160 Individuals 9 Individuals Armed attacks OVERVIEW The crisis in Nigeria’s North Central and North West zones, which involves long-standing tensions between NIGER REPUBLIC ethnic and religious groups; attacks by criminal Kaita Mashi Mai'adua Jibia groups; and banditry/hirabah (such as kidnapping and Katsina Daura Zango Dutsi Faskari Batagarawa Mani Rimi Safana grand larceny along major highways) led to a fresh Batsari Baure Bindawa wave of population displacement. 134 Kurfi Charanchi Ingawa Sandamu Kusada Dutsin-Ma Kankia Following these events, a rapid assessment was Katsina Matazu conducted by DTM (Displacement Tracking Matrix) Dan Musa Jigawa Musawa field staff between 25 and 31 January 2021, with the Kankara purpose of informing the humanitarian community Malumfashi Katsina Kano Faskari Kafur and government partners in enabling targeted Bakori response. Flash reports utilise direct observation and Funtua Dandume Danja a broad network of key informants to gather represen- Sabuwa tative data and collect information on the number, profile and immediate needs of affected populations. NIGERIA Latest attacks affected 160 individuals, including 14 injuries and 9 fatalities, in Makurdi LGA of Benue State and Faskari LGA of Katsina State. The attacks caused Kaduna people to flee to neighbouring localities. SEX (FIG. 1) Plateau Federal Capital Territory 39% Nasarawa X Affected Population 61% Male Makurdi International border Female 26 State Guma Agatu Benue Makurdi LGA Apa Gwer West Tarka Oturkpo Gwer East Affected LGAs Gboko Ohimini Konshisha Ushongo The map is for illustration purposes only. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

House of Reps Order Paper Thursday 15 July, 2021
121 FOURTH REPUBLIC 9TH NATIONAL ASSEMBLY (2019–2023) THIRD SESSION NO. 14 HOUSE OF REPRESENTATIVES FEDERAL REPUBLIC OF NIGERIA ORDER PAPER Thursday 15 July 2021 1. Prayers 2. National Pledge 3. Approval of the Votes and Proceedings 4. Oaths 5. Messages from the President of the Federal Republic of Nigeria (if any) 6. Messages from the Senate of the Federal Republic of Nigeria (if any) 7. Messages from Other Parliament(s) (if any) 8. Other Announcements (if any) 9. Petitions (if any) 10. Matters of Urgent Public Importance 11. Personal Explanation PRESENTATION OF BILLS 1. Federal College of Education (Technical) Aghoro, Bayelsa State (Establishment) Bill, 2021 (HB. 1429) (Hon. Agbedi Yeitiemone Frederick) - First Reading. 2. National Eye Care Centre, Kaduna (Establishment, Etc) Act (Amendment) Bill, 2021 (HB. 1439) (Hon. Pascal Chigozie Obi) - First Reading. 3. Electronic Government (e-Government) Bill, 2021 (HB. 1432) (Hon. Sani Umar Bala) - First Reading. 4. Federal Medical Centre Zuru (Establishment) Bill, 2021 (HB. 1443) (Hon. Kabir Ibrahim Tukura) - First Reading. 5. National Centre for Agricultural Mechanization Act (Amendment) Bill, 2021(HB. 1445) (Hon. Sergius Ogun) - First Reading. 122 Thursday 15 July 2021 No. 14 6. Industrial Training Fund Act (Amendment) Bill, 2021 (HB. 1447) (Hon. Patrick Nathan Ifon) - First Reading. 7. Fiscal Responsibility Act (Amendment) Bill, 2021 (HB. 1534) (Hon. Satomi A. Ahmed) - First Reading. 8. Federal Highways Act (Amendment) Bill, 2021 (HB. 1535) (Hon. Satomi A. Ahmed) - First Reading. 9. Border Communities Development Agency (Establishment) Act (Amendment) Bill, 2021 (HB. 1536) (Hon. Satomi A. Ahmed) - First Reading. 10. Borstal Institutions and Remand Centres Act (Amendment) Bill, 2021 (HB. -

AFRREV STECH, Vol. 3(2) May, 2014
AFRREV STECH, Vol. 3(2) May, 2014 AFRREV STECH An International Journal of Science and Technology Bahir Dar, Ethiopia Vol. 3 (2), S/No 7, May, 2014: 51-65 ISSN 2225-8612 (Print) ISSN 2227-5444 (Online) http://dx.doi.org/10.4314/stech.v3i2.4 THE USE OF COMPOSITE WATER POVERTY INDEX IN ASSESSING WATER SCARCITY IN THE RURAL AREAS OF OYO STATE, NIGERIA IFABIYI, IFATOKUN PAUL Department of Geography and Environmental Management, Faculty of Social Sciences University of Ilorin; Ilorin, Kwara State, Nigeria E-mail: 234 8033231626 & OGUNBODE, TIMOTHY OYEBAMIJI Faculty of Law Bowen University, Iwo Osun State, Nigeria Abstract Physical availability of water resources is beneficial to man when it is readily accessible. Oyo State is noted for abundant surface water and appreciable groundwater resources in its pockets of regolith aquifers; as it has about eight months of rainy season and a relatively deep weathered regolith. In spite of this, cases of water associated diseases Copyright© IAARR 2014: www.afrrevjo.net 51 Indexed and Listed in AJOL, ARRONET AFRREV STECH, Vol. 3(2) May, 2014 and deaths have been reported in the rural areas of the state. This study attempts to conduct an investigation into accessibility to potable water in the rural areas of Oyo State, Nigeria via the component approach of water poverty index (WPI). Multistage method of sampling was applied to select 5 rural communities from 25 rural LGAs out of the 33 LGAs in the State. Data were collected through the administration of 1,250 copies of questionnaire across 125 rural communities. Component Index method as developed by Sullivan, et al (2003) was modified and used in this study. -

Visceral and Cutaneous Larva Migrans PAUL C
Visceral and Cutaneous Larva Migrans PAUL C. BEAVER, Ph.D. AMONG ANIMALS in general there is a In the development of our concepts of larva II. wide variety of parasitic infections in migrans there have been four major steps. The which larval stages migrate through and some¬ first, of course, was the discovery by Kirby- times later reside in the tissues of the host with¬ Smith and his associates some 30 years ago of out developing into fully mature adults. When nematode larvae in the skin of patients with such parasites are found in human hosts, the creeping eruption in Jacksonville, Fla. (6). infection may be referred to as larva migrans This was followed immediately by experi¬ although definition of this term is becoming mental proof by numerous workers that the increasingly difficult. The organisms impli¬ larvae of A. braziliense readily penetrate the cated in infections of this type include certain human skin and produce severe, typical creep¬ species of arthropods, flatworms, and nema¬ ing eruption. todes, but more especially the nematodes. From a practical point of view these demon¬ As generally used, the term larva migrans strations were perhaps too conclusive in that refers particularly to the migration of dog and they encouraged the impression that A. brazil¬ cat hookworm larvae in the human skin (cu¬ iense was the only cause of creeping eruption, taneous larva migrans or creeping eruption) and detracted from equally conclusive demon¬ and the migration of dog and cat ascarids in strations that other species of nematode larvae the viscera (visceral larva migrans). In a still have the ability to produce similarly the pro¬ more restricted sense, the terms cutaneous larva gressive linear lesions characteristic of creep¬ migrans and visceral larva migrans are some¬ ing eruption. -

IOM Nigeria DTM Flash Report NCNW 26 June 2020
FLASH REPORT: POPULATION DISPLACEMENT DTM North West/North Central Nigeria. Nigeria 22 - 26 JUNE 2020 Aected Population: Casualties: Movement Trigger: 2,349 Individuals 3 Individuals Armed attacks OVERVIEW Maikwama 219 The crisis in Nigeria’s North Central and North West zones, which involves long-standing Dandume tensions between ethnic and linguis�c groups; a�acks by criminal groups; and banditry/hirabah (such as kidnapping and grand larceny along major highways) led to fresh wave of popula�on displacement. Kaita Mashi Mai'adua Jibia Shinkafi Katsina Daura Zango Dutsi Batagarawa Mani Safana Latest a�acks affected 2,349 individuals, includ- Zurmi Rimi Batsari Baure Maradun Bindawa Kurfi ing 18 injuries and 3 fatali�es, in Dandume LGA Bakura Charanchi Ingawa Jigawa Kaura Namoda Sandamu Katsina Birnin Magaji Kusada Dutsin-Ma Kankia (Katsina) and Bukkuyum LGA (Zamfara) between Talata Mafara Bungudu Matazu Dan Musa 22 - 26 June, 2020. The a�acks caused people to Gusau Zamfara Musawa Gummi Kankara flee to neighboring locali�es. Bukkuyum Anka Tsafe Malumfashi Kano Faskari Kafur Gusau Bakori A rapid assessment was conducted by field staff Maru Funtua Dandume Danja to assess the impact on people and immediate Sabuwa needs. ± GENDER (FIG. 1) Kaduna X Affected PopulationPlateau 42% Kyaram 58% Male State Bukkuyum 2,130 Female Federal Capital Territory LGA Nasarawa Affected LGAs The map is for illustration purposes only. The depiction and use of boundaries, geographic names and related data shown are not warranted to be error free nor do they imply judgment on the legal status of any territory, or any endorsement or accpetance of such boundaries by MOST NEEDED ASSISTANCE (FIG.