Evaluation of Two Vaginal, Uterus Sparing Operations for Pelvic Organ Prolapse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sl.No CGHS Treatment Procedure/Investigation List Rates for Non NABH Rates for NABH CGHS Bengaluru Rate List
CGHS Bengaluru Rate List Sl.No CGHS Treatment Procedure/Investigation Rates for Non Rates for List NABH NABH 1 Consultation OPD 135 135 2 Consultation- for Inpatients 270 270 3 Dressings of wounds 45 52 4 Suturing of wounds with local anesthesia 108 124 5 Aspiration Plural Effusion - Diagnostic 120 138 6 Aspiration Plural Effusion - Therapeutic 174 200 7 Abdominal Aspiration - Diagnostic 330 380 8 Abdominal Aspiration - Therapeutic 414 476 9 Pericardial Aspiration 342 393 10 Joints Aspiration 285 329 11 Biopsy Skin 207 239 12 Removal of Stitches 36 41 13 Venesection 124 143 14 Phimosis Under LA 1180 1357 15 Sternal puncture 173 199 16 Injection for Haemorrhoids 373 428 17 Injection for Varicose Veins 315 363 18 Catheterisation 425 500 19 Dilatation of Urethra 450 518 20 Incision & Drainage 378 435 21 Intercostal Drainage 125 144 22 Peritoneal Dialysis 1319 1517 TREATMENT PROCEDURE SKIN 23 Excision of Moles 311 357 24 Excision of Warts 279 321 25 Excision of Molluscum contagiosum 117 135 26 Excision of Veneral Warts 144 166 27 Excision of Corns 126 145 28 I/D Injection Keloid 97 112 29 Chemical Cautery (s) 99 114 TREATMENT PROCEDURE OPTHALMOLOGY 30 66 76 eyes Subconjunctival/subtenon’s injections in one 31 132 152 eyes 32 PterygiumSubconjunctival/subtenon’s Surgery injections in both 5550 6325 33 Conjunctival Peritomy 58 67 34 Conjunctival wound repair or exploration 3300 3795 following blunt trauma 35 Removal of corneal foreign body 115 132 36 Cauterization of ulcer/subconjunctival injection 69 79 in one eye 37 Cauterization of ulcer/subconjunctival -
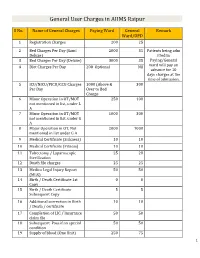
General User Charges in AIIMS Raipur
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

Shirodkar's Extended Manchester Repair
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 2, 2014 pp 263-266 Shirodkar’s Extended Manchester Repair: A Conservative Vaginal Surgery for Genital Prolapse in Young Women and Reinforcement of Weak Uterosacral Ligaments with Merselene Tape: Retrospective and Prospective Study Roohi Shaikh 1, Suman Sardesai 2* 1Assistant Professor, Department of OBGY, Indian Institute of Medical Science and Research, Warudi, Badnapur, Jalna Maharashtra INDIA. 2Professor and HOD, Department of OBGY, Dr. V. M. Medical College, Solapur, INDIA. *Corresponding Address: *[email protected], #[email protected] Research Article Abstract: The aim of this study was to evaluate the results of ligaments to the anterior aspect of what remains of the Shirodkar Extended Manchester Repair operation for uterine cervix, an anterior colporrphaphy and perineorhhapy is prolapse in young women interested in retaining future done. This time honoured technique has various childbearing and menstrual function. Materials and Methods: 30 patients with II or III degree utero-vaginal prolapse with or without shortcomings i.e. cervical stenosis, infertility, cervical cystoenterorectocoele and with normal uterocervical length (i.e. no incompetence, cervical dystocia during labour, cervical elongation) in child-bearing age group (i.e. less than 35 dyspareunia and recurrence of prolapse after pregnancy or years) interested in preserving future fertility or menstrual function otherwise was also reported to the extent of 20-25% were operated and followed-up. In patients with weak uterosacral (Shaw 1933).An ideal conservative method should ligament, reinforcement with merselene tape was done. Results: In preserve menstruation, restore the fertility and should not this study, 79% of the patients were below the age of 30 years. -

UNMH Obstetrics and Gynecology Clinical Privileges Name
UNMH Obstetrics and Gynecology Clinical Privileges Name:____________________________ Effective Dates: From __________ To ___________ All new applicants must meet the following requirements as approved by the UNMH Board of Trustees, effective April 28, 2017: Initial Privileges (initial appointment) Renewal of Privileges (reappointment) Expansion of Privileges (modification) INSTRUCTIONS: Applicant: Check off the “requested” box for each privilege requested. Applicants have the burden of producing information deemed adequate by the Hospital for a proper evaluation of current competence, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Department Chair: Check the appropriate box for recommendation on the last page of this form. If recommended with conditions or not recommended, provide condition or explanation. OTHER REQUIREMENTS: 1. Note that privileges granted may only be exercised at UNM Hospitals and clinics that have the appropriate equipment, license, beds, staff, and other support required to provide the services defined in this document. Site-specific services may be defined in hospital or department policy. 2. This document defines qualifications to exercise clinical privileges. The applicant must also adhere to any additional organizational, regulatory, or accreditation requirements that the organization is obligated to meet. --------------------------------------------------------------------------------------------------------------------------------------- -

SCHEDULE of CHARGES -2018 (Eff Ective from 01.04.2018 to 31.03.2020)
HOLY FAMILY HOSPITAL, NEW DELHI. SCHEDULE OF CHARGES -2018 (Eff ective from 01.04.2018 to 31.03.2020) HOLY FAMILY HOSPITAL HOLOKHLAY ROFAMILAD, NEWY DELHIHOSPIT - 110025AL HOLOKHLAY ROFAMILAD, NEWY DELHIHOSPIT - 110025AL OKHLA ROAD, NEW DELHI - 110025 HOLY FAMILY HOSPITAL OKHLASchedule ROAD, NEW of DELHICharges - 110025 ScheduleEffective 1of April, Charges 2018 ScheduleEffective 1of April, Charges 2018 Effective 1 April, 2018 Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 +91 11 2684 5900 to 2684 5909 Email : [email protected] Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 P hone Nos: Schedule +91+91 1111 Schedule 26842633 59002800 toto 26842633 of 59092809 ChargesofEmailF axCharges No : adimini: +91 11 [email protected] - 32252018 +91 11 Schedule2684 5900 to 2684 5909 ofEmail Charges : [email protected] Effective 1 April,st 2018 Eff Effectiveecti ve from 1 April, 1 April, 2018 2018 (Valid upto 31st March, 2020) Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 Phone Nos: +91 11 2633 2800 to 2633 2809 Fax No : +91 11 2691 3225 +91 11 2684 5900 to 2684 5909 Email : [email protected] +91 11 2684 5900 to 2684 5909 1 Email : [email protected] HOLY FAMILY HOSPITAL, NEW DELHI. SCHEDULE OF CHARGES -2018 (Effective from 01.04.2018 to 31.03.2020) INDEX S.No. CHARGING HEAD Page No. 1 General Information 3 In-Patient Schedule of Charges 2 Room / Bed and Board 5 3 CCU/ICU / Ped. ICU / Post Op. ICU and Board 5 4 Oxygen 5 5 Ventilator 5 6 NNU – Nursery, Photo Therapy, Incubator, Nursing Care 5 7 Hospital Doctor’s Fee :- Visits 6 8 :- Consultation 6 9 Surgery Fee : General Surgery 6 10 Surgery Fee : Laparoscopic General Surgery 9 11 Surgery Fee : Hernia Surgery 12 12 Surgery Fee : Breast Surgery 12 13 Surgery Fee : Rectal Surgery 13 14 Surgery Fee : O.B. -

ICD-9-CM Procedures (FY10)
2 PREFACE This sixth edition of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) is being published by the United States Government in recognition of its responsibility to promulgate this classification throughout the United States for morbidity coding. The International Classification of Diseases, 9th Revision, published by the World Health Organization (WHO) is the foundation of the ICD-9-CM and continues to be the classification employed in cause-of-death coding in the United States. The ICD-9-CM is completely comparable with the ICD-9. The WHO Collaborating Center for Classification of Diseases in North America serves as liaison between the international obligations for comparable classifications and the national health data needs of the United States. The ICD-9-CM is recommended for use in all clinical settings but is required for reporting diagnoses and diseases to all U.S. Public Health Service and the Centers for Medicare & Medicaid Services (formerly the Health Care Financing Administration) programs. Guidance in the use of this classification can be found in the section "Guidance in the Use of ICD-9-CM." ICD-9-CM extensions, interpretations, modifications, addenda, or errata other than those approved by the U.S. Public Health Service and the Centers for Medicare & Medicaid Services are not to be considered official and should not be utilized. Continuous maintenance of the ICD-9- CM is the responsibility of the Federal Government. However, because the ICD-9-CM represents the best in contemporary thinking of clinicians, nosologists, epidemiologists, and statisticians from both public and private sectors, no future modifications will be considered without extensive advice from the appropriate representatives of all major users. -

Nomenclatures of Procedures and Operations Promulgated by Colleges of the Hong Kong Academy of Medicine (August 2021)
Nomenclatures of procedures and operations promulgated by Colleges of the Hong Kong Academy of Medicine (August 2021) College English Chinese 1 AN Nomenclature of Procedures in Anaesthesia and Intensive Care 2 AN Group A: Mode of anaesthesia or sedation A組:麻醉或鎮靜模式 3 AN General anaesthesia 全身麻醉 4 AN Monitored anaesthetic care (MAC) 專業麻醉照護 5 AN Regional technique: neural blockade-anaesthesia/analgesia 區域麻醉:神經阻滯麻醉/鎮痛 6 AN Regional technique: Epidural anaesthesia/analgesia 區域麻醉:硬膜外麻醉/鎮痛 7 AN Regional technique: Spinal anaesthesia/analgesia 區域麻醉:脊椎麻醉/鎮痛 8 AN Regional technique: Intravenous regional anaesthesia 區域麻醉: 經靜脈注射區域麻醉 9 AN Group B: airway B組:氣道 10 AN Endotracheal Intubation 氣管插管術 11 AN Laryngeal mask airway 喉罩通氣道 12 AN Face mask airway 面罩通氣道 13 AN Awake fiberoptic intubation 清醒支氣管鏡插管 14 AN Percutaneous Tracheotomy 經皮氣管切開術 15 AN Intermittent positive airway pressure ventilation 間歇正壓通氣 16 AN Non-invasive pressure ventilation CPAP (mask) 非侵入性連續呼吸道正壓通氣(面罩) 17 AN Non-invasive pressure ventilation BiPAP (mask) 非侵入性雙水平式呼吸道正壓通氣(面罩) 18 AN Hyperbaric oxygen therapy 高壓氧治療 19 AN Extracorporeal Membrane Oxygenation (ECMO) 體外膜式人工氧合法 20 AN Bronchoscopy 支氣管鏡檢查 21 AN Pleural drainage 胸腔引流 22 AN Group C: circulation C組:循環 23 AN Intravenous cannulation 靜脈插管 24 AN Arterial catheterization 動脈導管 25 AN Cardiopulmonary resuscitation (CPR) 心肺復蘇術(CPR) 26 AN Defibrillation 除顫術 27 AN Cardioversion 心律轉變 28 AN Temporary Pacemaker 臨時起搏器 29 AN Central venous catheter 中央靜脈導管 30 AN Pulmonary artery catheter 肺動脈導管 31 AN Echocardiography (Transthoracic) 超聲心動圖(經胸腔) 32 -

Phaneuf-Manchester Operation for Uterine Prolapse ‘57
Am J Surgery 1951 V-82 MANCHESTER OPERATION OF COLPORRHAPHY IN THE TREATMENT OF UTERINE PROLAPSE* LOUIS E. PHANEUP, M.D. Boston, Massachusetts TERINE prolapse is an old Iesion about suture material, catgut, was being tried in which much has been written. Among genera1 surgery in Germany, Donald obtained U the writings of Hippocrates reference some of this catgut, sterilized in carbolic oil, is made to the fact that dispIacements of the and used it in the performance of his third uterus were recognized but it was not until the operation on August 3, I 888. He did an anterior time of GaIen, 130 to 210 A.D., that this condi- coIporrhaphy and approximated the deep tion excited much interest. GaIen also we11 tissues with a buried continuous suture of described the condition of proIapsus uteri. catgut. Two weeks Iater he did a posterior According to William FIetcher Shaw,’ Mar- coIporrhaphy using the same technic. The shaI1 Ha11 of London seems to have been the patient was discharged on August 30th and the first to suggest narrowing the vagina in the folIowing discharge note was made: “The treatment of uterine proIapse but there is no wound was heaIed and the outIet of the vagina record that he performed the operation himself. onIy admitted two fingers with difficulty, no In 1831 Heming operated upon the anterior pessary was inserted.” Originally Donald made vagina1 waI1 and was foIIowed by numerous the denudation of the anterior vaginal wall with other surgeons, including Marion Sims, Emmet, a wide diamond-shaped incision; later, W. E. -

Manchester Repair an Alternative to Hysterectomy
Case Reports Manchester repair An alternative to hysterectomy Abdulrahim A. Rouzi, MBChB, FRCSC, Nora N. Sahly, MBChB, Amal S. Shobkshi, MD, Hassan S. Abduljabbar, MBChB, FRCSC. ABSTRACT terine prolapse is defined as the descent of the Uuterus and cervix into the vaginal canal toward the introitus. Some degree of uterine prolapse is common in parous women; however, symptomatic الدراسات املوجودة ًحاليا ﻻ تتوفر أية معلومات فيما يخص عمليات uterine prolapse is not common in women during their )مانشستر(. نستعرض في هذا التقرير وبأثر رجعي سلسلة من reproductive years. Treatment options include both الدراسات لسبع سيدات كن يعانني من هبوط في الرحم، وخضعن non-surgical and surgical modalities, but the failure rate لعملية )مانشستر(، وذلك خﻻل الفترة مابني يناير 1997م وحتى ,is high with non-surgical approaches. Surgical options مايو 2008م، مبستشفى امللك عبد العزيز اجلامعي – جدة – اململكة in particular vaginal hysterectomy, are therefore the العربية السعودية. وقد مرت جميع هؤﻻء السيدات مبراحل احلمل standard treatments in these cases. Hysterectomy may والوﻻدة ولدين ) (3±1 أبناء، ويرغنب في تفادي عملية استئصال not, however, be acceptable to young women with a الرحم وإجناب املزيد. تراوحت مدة العملية مابني 16±119 دقيقة، second degree uterine prolapse who want to preserve ولم يكن هناك أية مضاعفات خﻻل العملية. تراوحت مدة املتابعة -their fertility. In this group of patients, the Manchester ما بعد العملية 5±2 أعوام. كانت جميع السيدات راضيات عن Fothergill procedure (commonly referred to as the نتائج العملية. حملت مريضتني )%28.6( وكانت وﻻداتهن طبيعة Manchester repair) should be considered. This procedure was first performed in 1888 by Dr. Archibald Donald in وناجحة. -

Short and Long-Term Outcomes of the Manchester Procedure for Pelvic Organ Prolapse and the Impact of Major Levator Ani Muscle Defects
Short and long-term outcomes of the Manchester Procedure for Pelvic Organ Prolapse and the impact of major Levator Ani Muscle defects PhD thesis by Sissel Hegdahl Oversand, MD 2018 Department of Gynaecology, Oslo University Hospital, Ullevål and University of Oslo, Faculty of Medicine, Norway © Sissel Hegdahl Oversand, 2018 Series of dissertations submitted to the Faculty of Medicine, University of Oslo ISBN 978-82-8377-335-4 All rights reserved. No part of this publication may be reproduced or transmitted, in any form or by any means, without permission. Cover: Hanne Baadsgaard Utigard. Print production: Reprosentralen, University of Oslo. # " !$ ! ." '&*&0# &)),(*&0#),!(-/**),. &0.),(#'/-&0/&-#)(- *&0#),!(*,)&*- -/,!#&'(!'(.) *&0#),!(*,)&*- ."'("-.,*,)/, *)*-/,!,3#(.,(&+/&#.3)(.,)& )/.)''-/,-#(*)*-/,!,3 )-.^ .#0(-- *.#(.-&.#)( -/,!#&.(#+/- (.)'#&0&/.#)(.))&- *.#(. ,*),.0&/.#)(.))&- )/.)''-/,- (0196,6(8, 3(8420*(1498*42,7 !(80,386,5468,+498*42,7 42510*(80437 -..#-.#&(&3--(*)1,&/&.#)(- &!#-&.#)((,-,"."#- !$! -"),.(&)(! .,' #&/,,.- *,0&() &'0/&-#)(-(#'*.)(*,)*,.#0 -../- #'*.) &'0/&-#)(-)()( 3,*)-.)*,.#0)/.)'- (.)'#&(*.#(. ,*),.)/.)'-)(3, ., (.#0.#--/*)*,*#,-1#."'#( )/-)(."'("-., *,)/, ! '."))&)!#&)(-#,.#)(- B #89+=+,70.3(3+789+=54591(80437 07703.+(8( !,1:0* 6.(3!641(57,"9(380-0*(80437*(1,! !">>>>> $6(375,603,(1%186(7493+ "9,780433(06,7 $,1,5/43,038,6:0,; #86,3./87(3+10208(80437 #8(80780*(1(3(1=7,7 #-/--#)() -

Joint Report on Terminology for Surgical Procedures to Treat Pelvic
AUGS-IUGA JOINT PUBLICATION Joint Report on Terminology for Surgical Procedures to Treat Pelvic Organ Prolapse Developed by the Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. Individual contributors are noted in the acknowledgment section. 03/02/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3JfJeJsayAVVC6IBQr6djgLHr3m8XRMZF6k61FXizrL9aj3Mm1iL7ZA== by https://journals.lww.com/jpelvicsurgery from Downloaded meaningful data about specific procedures, standardized and Downloaded Abstract: Surgeries for pelvic organ prolapse (POP) are common, but widely accepted terminology must be adopted. Each term for a standardization of surgical terms is needed to improve the quality of in- given procedure must indicate to researchers, clinicians, and from vestigation and clinical care around these procedures. The American learners a specific and reliable minimal set of steps. The aim of https://journals.lww.com/jpelvicsurgery Urogynecologic Society and the International Urogynecologic Associ- this document is to propose a standardized terminology to de- ation convened a joint writing group consisting of 5 designees from scribe common surgeries for POP. each society to standardize terminology around common surgical terms in POP repair including the following: sacrocolpopexy (including sacral colpoperineopexy), sacrocervicopexy, uterosacral ligament suspension, sacrospinous ligament fixation, iliococcygeus fixation, uterine preserva- tion prolapse procedures or hysteropexy -

MIDLAND MEMORIAL HOSPITAL Delineation of Privileges FEMALE PELVIC MEDICINE and RECONSTRUCTIVE SURGERY (UROGYNECOLOGY)
MIDLAND MEMORIAL HOSPITAL Delineation of Privileges FEMALE PELVIC MEDICINE AND RECONSTRUCTIVE SURGERY (UROGYNECOLOGY) Your home for healthcare Physician Name: _____________________________________________________ Female Pelvic Medicine and Reconstructive Surgery Core Privileges Qualifications Minimum threshold criteria for requesting core privileges in obstetrics and gynecology: Basic education: MD or DO Successful completion of an ACGME- or AOA-accredited residency in OB/GYN. Successful completion of an ABOG, ACGME or AOA approved fellowship in female pelvic medicine and reconstructive surgery. AND Current subspecialty certification or board eligible (with achievement of certification within 5 years) leading to subspecialty certification in female pelvic medicine and reconstructive surgery by the ABOG. (*Members of the Staff, prior to the adoption of Bylaws 10/2007, are considered grandfathered in for privileges, but cannot achieve board certification as of 2014). Required current experience: Applicants must be able to demonstrate that they have performed at least 50 female pelvic medicine and reconstructive surgical procedures, reflective of the scope of privileges requested, in the past 12-months, or successful completion of an ACGME or AOA accredited FPMRS fellowship within the past 12-months. References for New Applicants If the applicant is recently trained, a letter of reference should come from the director of the applicant’s training program. Alternatively, a letter of reference may come from the applicable department chair and/or clinical service chief at the facility where the applicant most recently practiced. Renewal of privileges Reappointment should be based on unbiased, objective results of care according to the organization’s existing quality improvement measures. Current demonstrated competence and adequate volume of experience in 50 procedures with acceptable results, reflective of the scope of privileges requested, for the past 24 months based on results of ongoing professional practice evaluation and outcomes.