Spatial Differences and Socio-Economic Determinants of Health Poverty
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Authoritarianism and Political Party Reforms in Pakistan
AUTHORITARIANISM AND POLITICAL PARTY REFORM IN PAKISTAN Asia Report N°102 – 28 September 2005 TABLE OF CONTENTS EXECUTIVE SUMMARY AND RECOMMENDATIONS................................................. i I. INTRODUCTION .......................................................................................................... 1 II. PARTIES BEFORE MUSHARRAF............................................................................. 2 A. AFTER INDEPENDENCE..........................................................................................................2 B. THE FIRST MILITARY GOVERNMENT.....................................................................................3 C. CIVILIAN RULE AND MILITARY INTERVENTION.....................................................................4 D. DISTORTED DEMOCRACY......................................................................................................5 III. POLITICAL PARTIES UNDER MUSHARRAF ...................................................... 6 A. CIVILIAN ALLIES...................................................................................................................6 B. MANIPULATING SEATS..........................................................................................................7 C. SETTING THE STAGE .............................................................................................................8 IV. A PARTY OVERVIEW ............................................................................................... 11 A. THE MAINSTREAM:.............................................................................................................11 -

A Comparative Study of Directly Selected, In-Service Promoted and Online Selected Subject Specialists Regarding Teaching Effectiveness in Kohat Division, Pakistan
Journal of Education and Practice www.iiste.org ISSN 2222-1735 (Paper) ISSN 2222-288X (Online) Vol.6, No.10, 2015 A Comparative Study of Directly Selected, In-Service Promoted and Online Selected Subject Specialists Regarding Teaching Effectiveness in Kohat Division, Pakistan Qaiser Suleman PhD (Education) Scholar, Institute of Education & Research, Kohat University of Science & Technology Kohat, Khyber Pakhtunkhwa, (Pakistan) Email: [email protected] Rizwana Gul M.Phil (Education) Scholar, Institute of Education & Research, Kohat University of Science & Technology Kohat, Khyber Pakhtunkhwa, (Pakistan) Abstract The main objective of the study was to compare the teaching effectiveness of directly selected, in-service promoted and online selected subject specialists teaching at higher secondary school level in Kohat Division, Pakistan. The target population of the study was the higher secondary school students in Kohat Division, Pakistan. A sample of 600 students randomly selected from 10 out of 20 higher secondary schools in Kohat Division was used in this study. The design of this research study was survey. A self-developed structured questionnaire was used a research instrument for data collection. Statistical tools i.e., mean, standard deviation, ANOVA and Post-hoc t-tests were used. After statistical analysis, it was concluded that the teaching performance of the directly selected subject specialists was highly appreciable and excellent. On the other hand, teaching performance of in-service promoted subject specialists was found satisfactory while teaching performance of online selected subject specialists was poor and unsatisfactory. Based on findings, it was recommended that at least 75% of the total subject specialists should be recruited through Khyber Pakhtunkhwa Public Service Commission only. -

Government of Khyber Pakhtunkhwa
GOVERNMENT OF KHYBER PAKHTUNKHWA Public Disclosure Authorized Public Disclosure Authorized Qabail Led Community Support Project (QLCSP) Environmental and Social Management Framework (ESMF) Public Disclosure Authorized December 21, 2019 To be executed By Planning & Development Department (GoKP) Through Public Disclosure Authorized Directorate of Projects under the Merged Areas Secretariat (MAS) EXECUTIVE SUMMARY Introduction The Government of Khyber Pakhtunkhwa (GoKP), through Directorate of Projects Planning & Development Department (DP&DD), intends to implement “Qabail Led Community Support Program (QLCSP”) in Khyber district of merged areas (MA) – the erstwhile Federally Administered Tribal Areas (FATA)1 – and Peshawar and Nowshera districts of KP with the proposed assistance of the World Bank (WB).2 This Environmental and Social Management Framework (ESMF) has been prepared to meet requirements of national legislation of Pakistan and World Bank environmental and social policy requirements to address potential negative impacts from the proposed project. Project Overview Background The Central Asia-South Asia Electricity Transmission and Trade Project (CASA1000) aims to facilitate electricity trade between Central Asia and countries in South Asia by putting in place transmission infrastructure. As part of CASA1000 project, each participating country3 is implementing Community Support Programs (CSPs) to share the benefits associated with the project and to generate support among local communities. Project Area In Pakistan, the CASA1000 transmission line (TL) will pass through approximately 100 kilometer long territory passing through various parts of KP province. The project area accordingly lies in/includes Peshawar and Nowshera districts and Khyber district4 of merged areas (MA). Project Components The Project has four components as briefly described below; and its Project Development Objective (PDO) is “improve access to local infrastructure and strengthen community engagement in the project areas”. -
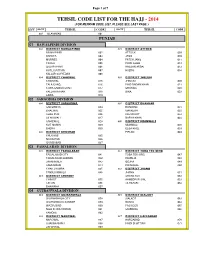
Tehsil Code List for the Hajj
Page 1 of 7 TEHSIL CODE LIST FOR THE HAJJ - 2014 (FOR MEHRAM CODE LIST, PLEASE SEE LAST PAGE ) DIV DISTT TEHSIL CODE DISTT TEHSIL CODE 001 ISLAMABAD 001 PUNJAB 01 RAWALPINDI DIVISION 002 DISTRICT RAWALPINDI 003 DISTRICT ATTOCK RAWALPINDI 002 ATTOCK 009 KAHUTA 003 JAND 010 MURREE 004 FATEH JANG 011 TAXILA 005 PINDI GHEB 012 GUJAR KHAN 006 HASSAN ABDAL 013 KOTLI SATTIAN 007 HAZRO 014 KALLAR SAYYEDAN 008 004 DISTRICT CHAKWAL 005 DISTRICT JHELUM CHAKWAL 015 JHELUM 020 TALA GANG 016 PIND DADAN KHAN 021 CHOA SAIDAN SHAH 017 SOHAWA 022 KALLAR KAHAR 018 DINA 023 LAWA 019 02 SARGODHA DIVISION 006 DISTRICT SARGODHA 007 DISTRICT BHAKKAR SARGODHA 024 BHAKKAR 031 BHALWAL 025 MANKERA 032 SHAH PUR 026 KALUR KOT 033 SILAN WALI 027 DARYA KHAN 034 SAHIEWAL 028 009 DISTRICT MIANWALI KOT MOMIN 029 MIANWALI 038 BHERA 030 ESSA KHEL 039 008 DISTRICT KHUSHAB PIPLAN 040 KHUSHAB 035 NOOR PUR 036 QUAIDABAD 037 03 FAISALABAD DIVISION 010 DISTRICT FAISALABAD 011 DISTRICT TOBA TEK SING FAISALABAD CITY 041 TOBA TEK SING 047 FAISALABAD SADDAR 042 KAMALIA 048 JARANWALA 043 GOJRA 049 SAMUNDARI 044 PIR MAHAL 050 CHAK JHUMRA 045 012 DISTRICT JHANG TANDLIANWALA 046 JHANG 051 013 DISTRICT CHINIOT SHORE KOT 052 CHINIOT 055 AHMEDPUR SIAL 053 LALIAN 056 18-HAZARI 054 BHAWANA 057 04 GUJRANWALA DIVISION 014 DISTRICT GUJRANWALA 015 DISTRICT SIALKOT GUJRANWALA CITY 058 SIALKOT 063 GUJRANWALA SADDAR 059 DASKA 064 WAZIRABAD 060 PASROOR 065 NOSHEHRA VIRKAN 061 SAMBRIAL 066 KAMOKE 062 016 DISTRICT NAROWAL 017 DISTRICT HAFIZABAD NAROWAL 067 HAFIZABAD 070 SHAKAR GARH 068 PINDI BHATTIAN -
Gypsum Mining & Processing District Kohat, Khyber
Cluster Study –Gypsum Mining & Processing- Kohat, Khyber Pakhtunkhwa Final Report GYPSUM MINING & PROCESSING DISTRICT KOHAT, KHYBER PAKHTUNKHWA Cluster Study Mineral Transformation Plan Vision 2025 Ministry of Planning, Development & Reforms, Government of Pakistan. Cluster Based Mineral Transformation Plan V2025- Feasibility Study Page | 1 Cluster Study –Gypsum Mining & Processing- Kohat, Khyber Pakhtunkhwa Contents 1. ABOUT THE STUDY.................................................................................................................................. 7 2. DESCRIPTION OF THE CLUSTER ......................................................................................................... 8 2.1. Introduction ....................................................................................................................................... 8 2.1.1. Strategic Location of the Cluster ........................................................................................ 8 2.2. Situational Analysis ....................................................................................................................... 10 2.2.1. Enterprise Base...................................................................................................................... 10 2.2.2. Products ................................................................................................................................... 16 2.2.3. Production Statistics ........................................................................................................... -

Public Information Officers Contact List
Public Information Officers Contact List S.NO NAME DESIGNATION DEPARTMENT Sub-Department DISTRICT TELEPHONE CELL NUMBER EMAIL 1 Mr. Muhammad Riaz DEO (M) Education ELEMENTARY EDUCATION DEPARTMENT Abbottabad 0992-9310102 3335060225 [email protected] 2 Miss. Samina Altaf DEO (F) Education ELEMENTARY EDUCATION DEPARTMENT Abbottabad 0992-342314 3 Dr. Fazle Rehman Director Livestock, Abbottabad Agriculture DIRECTORATE OF AGRICULTURE (EXTENSION) Abbottabad 0992-382628 4 Dr. Pervez Principal Research Officer/Regional Director Agriculture DIRECTOR GENERAL (RESEARCH) LIVESTOCK & DAIRY DEVELOPMENT Abbottabad 0992-383763 0345-8566012 5 Mr. Waqas Ashraf Assistant Public Prosecutor Law DISTRICT ABBOTTABAD Abbottabad 0992-9310383 0300-9110884 [email protected] 6 Mr. Mussamer Shah Assistant Manager (Legal) Forest Development Corporation Forest & Environment DISTRICT ABBOTTABAD Abbottabad 0992-380897 7 Mr. Naeem Khan Additional Deputy Commissioner Revenue Deputy Commissioner Abbottabad 0992-9310207 [email protected] 8 Mr. Jahanzeb Khan Deputy Director Small Industrial Estate Small Industrial Estate Abbottabad 0992-383770 9 Mr. Zaffar Ali Khan DFO, Gallis, Abbottabad Forest & Environment Environment Abbottabad 0992-9310306 [email protected] 10 Mr. Faiq Khan DFO, Wildlife, Abbottabad Forest & Environment Environment Abbottabad 0992-9310323 0302-193344 [email protected] 11 Mr. Khabir Muhammad Police Hazara Division, Hazara Abbottabad 0992-9310516 12 Mr. Jawad Khan Sub Divisional Officer Irrigation Irrigation Sub Divisional Abbotabad Abbottabad 0992-9310246 0346-9577518 13 Mr. Baber Shamrez Research Officer Agriculture Agriculture Research System Abbottabad 0992-380873 0345-5300126 14 Muhammad Saleem Raza District Sports Officer Abbottabad and Torghar Sports Sports Department Abbottabad 0992-9310224 0334-9067114 15 Abdul Malik Khan DSP/FRP Police Police department Abbottabad 0992-9310020 0300-5796002 16 Waheed Gul District Zakat Officer Zakat and Ushar Zakat & Usher Dept . -

Molecular Prevalence of Hepatitis B Virus Infection in Khyber Pakhtunkhwa, Pakistan
International Journal of Medicine and Medical Sciences Vol. 4(5), pp. 123-127, July 2012 Available online at http://www.academicjournals.org/IJMMS DOI: 10.5897/IJMMS12.095 ISSN 2006-9723 ©2012 Academic Journals Full Length Research Paper Molecular prevalence of Hepatitis B virus infection in Khyber Pakhtunkhwa, Pakistan Zia Ur Rahman Awan1*, Abdul Haleem Shah1, Sanaullah Khan2, Saeed Ur Rahman1 and Hafiz Munib Ur Rahman1 1Department of Biological Sciences, Gomal University Dera Ismail Khan, Pakistan. 2Department of Zoology, Kohat University of Sciences and Technology Kohat, Pakistan. Accepted 1 June, 2012 Hepatitis B virus (HBV) infection is a major health problem in the developing countries including Pakistan. This study aimed to investigate various risk factors and prevalence of HBV in different areas of Khyber Pakhtunkhwa province, Pakistan. A total of 1439 individuals (1021 males and 418 females) suspected for hepatitis B infection were screened for HBsAg. All the samples were blindly analyzed for HBV DNA by nested polymerase chain reaction (PCR). Of the total, 49.5% were found positive for HBsAg. Of these HBsAg positive patients, 83.03% were confirmed for HBV DNA. Of the 726 HBsAg negative individuals, 37 (24 males and 13 females) were found positive for HBV DNA. 629 HBV DNA positive individuals include 70.43% male and 29.57% female. Higher prevalence rate (16.53%) was observed in Malakand and lowest (13.35%) in Mardan. Mostly young people with age 16 to 30 years were infected as compared to other age group. Risk factors observed in HBV positive individuals were unhygienic barber practice, blood transfusion, general and dental surgery, unsafe injection and sharing personal items. -

Abbreviations and Acronyms
P ART III] THE GAZETTE OF PAKISTAN, EXTRA., NOV. 21, 2019 1945 ISLAMABAD, FRIDAY, NOVEMBER 29, 2019 PART III Other Notifications, Orders, etc. ELECTION COMMISSION OF PAKISTAN NOTIFICATION Islamabad, the 26th November, 2019 No. F. 12(3)/2019-E/Rolls(3).—In exercise of the powers conferred by section 29 of the Election Act, 2017, the Election Commission of Pakistan is pleased to appoint for the purpose of receiving and deciding claims, objections and applications of correction of votes, the officers specified in column 2 of the schedule below, to be the Revising Authorities in the Province of Khyber Pakhtunkhwa, for the electoral areas falling within the jurisdiction mentioned against each in the corresponding entry in the column 3 of the said schedule. (1945) Price: Rs. 5.00 [1856(2019)/Ex.Gaz.] 1946 THE GAZETTE OF PAKISTAN, EXTRA., NOV. 29, 2019 [PART III SCHEDULE Sl. Revising Authority Jurisdiction No. 1 2 3 Regional Election Commissioner, 1. District Peshawar (including Sub-Division Hassan Khel) 1. Peshawar Division 2 District Charsadda 3. District Nowshera Regional Election Commissioner, 1. District Mardan 2. District Swabi 2. Mardan Division 1. District Kohat (including Sub-Division Dara Adam Khel) Regional Election Commissioner, 3. Kohat Division 2. District Karak 3. District Hangu 4. District Okrakzai 5. District Kurrum 1. Bannu (including Sub-Division Wazir) Regional Election Commissioner, 4. 2. District Lakki Marwat (including Sub-Division Bhettani) Bannu Division 3. District North Wazirstan 1. District D. I. Khan (including Sub-Division Darazanda) Regional Election Commissioner, 5. D.I. Khan Division 2. District Tank (including Sub-Division Jandola) 3. -

4582 Opt.Pdf, PDF, 5.95MB
4'5 2J fL),1u ') jry 2 -LLL) jj )1 -i )11P J 7Yt1L)' cJb'L&J) ) 2019 _2O13 7 uestion No. 2355 Form Mst. Shagufta Malik, MPA Details of Purchased vehicles for Secretaries, Additional Secretaries, Deputy Secretaries, Commissioners, Deputy Commissioners, Additional Commissioners, Assistant Commissioners etc. during financial year 2013-2019. The Govt. of Khyber Pakhtunkhwa Administration Department had purchased nineteen (19) no. of vehicles by approval of the Competent Authority (Annex-I, II, III) during the year 2013-2019. Furthermore, allotment (handing/taking) of these vehicles are placed at Annex-IV. The Details of each vehicle is tabulated as below: S.NO VEHICLE NO MAKE/TYPE/ENGINE CAPACITY MODEL ALLOTED TO Amount Purchased from: Mr. Bakhtiar (BPS-20) 1 AB-1606 Toyota Corolla GLI 1300 CC 2018 Toyota khyber Motors -Ring Road Special Secretry Esatblishment Peshawar - Mr. Shahid Sohail Khan (BPS-19) 2 AB-2210 Toyota khyber Motors Ring Road Toyota Corolla GLI 1300 cc 2018 Additional Secretary Administration 1,989,500/- Peshawar Department AB-2214 Mr. NasirAman(BPS-19) Toyota khyber Motors Ring Road Toyota Corolla GLI 1300 cc 2018 1,989,500/- Additional Secretary (Regulation) Peshawar 4 AB-1879 Capt.(R) Abdur Rehman BS-18) Toyota khyber Motors Ring Road Toyota Corolla GLI 1300 cc 2018 1,989,500/- P50 to chief Secretary Peshawar 5 AB-2212 Syed Jamal uddin Shah (BS-20) Toyota khyber Motors Ring Road Toyota Corolla GLI 1300 cc 2018 1,989,500/- Secretary Establishment Peshawar 6 Toyota khyber Motors Ring Road AB-2213 Toyota Corolla GLI 1300 -

Final Research Paper Industrial Policy (Khyber
FINAL RESEARCH PAPER INDUSTRIAL POLICY (KHYBER PAKHTUNKHWA) PAKISTAN SUBMITTED BY: Syed Zaigham Kazmi SUBMITTED TO: Dr. Velma Grover This document is purely an academic exercise submitted in partial fulfillment for the Masters program of Engineering & Public Policy 1 CONTENT ABSTRACT………………………………………….. 3 INTRODUCTION…………………………………… 3 ABOUT KHYBER PAKHTUNKHWA…………….. 4 INDUSTRIAL BACKGROUND……………………. 8 PRESENT STATUS…………………………………. 12 OBJECTIVE…………………………………………. 14 CONSIDERATION…………………………………. 15 RECENT POLICIES………………………………… 16 INDUSTRIAL SURVEY…………………………….. 25 CHALLENGES & STRATEGY……………………. 27 OTHER POLICY OPTIONS………………………... 31 CONCLUSSION……………………………………… 33 APPENDIX……………………………………………. 35 ACRONYMS KP: Khyber Pakhtunkhwa NMC: National Management Consultant SDA: Sarhad Development Authority BSS: Business Support Services SEZ: Special Economic Zones IGC: International Growth Center FATA: Federally Administrated Tribal Area KPCCI: Khyber Pakhtunkhwa Chamber of Commerce and Industry SMEDA: Small & Medium Enterprises Development Authority 2 ABSTRACT: To development more sustainable society as industry in Khyber Pakhtunkhwa and needs to better understand how to respond to environmental, social and economic challenges and transform industrial behavior. At the center of the industrial sustainability, the purpose is to develop knowledge and tools that help accelerate the transition towards a sustainable industrial system. Industrial sustainability now appears to be moving up the management agenda in many organizations. [1] Industry is a key player in the -

Pakistan National Election: 1977
Gilanis’ Index of © ELECTORAL RECORD 1970-2013 Volume 2 PAKISTAN NATIONAL ELECTION: 1977 An 10 Volume Study prepared by Gallup Election studies team head by Bilal Gilani, Executive Director, Gallup Pakistan Prepared on April 30, 2013 Disclaimer: Gallup Pakistan is not related to Gallup Inc. headquartered in Washington D.C. USA. We require that our surveys be credited fully as Gallup Pakistan (not Gallup or Gallup Poll). We disclaim any responsibility for surveys pertaining to Pakistani public opinion except those carried out by Gallup Pakistan, the Pakistani affiliate of Gallup International Association. For details on Gallup International Association see website: www.gallup-international.comand www.gallup.com.pk Gilani’s Index of Electoral Record: 1970-2013 (An 10 Volume Study) C o n t e n t s Volume 2 Index of Electoral Record: 1977 Page # Table 1: Code List 24 Table 2: Turn Out 25 Table 3: Party Position: All Pakistan 26 Table 4: Party Position: Province-wise 27 Table 5: Party Position: Division-wise 31 Table 6: Party Position: 11 Electoral Territory 37 Basic Code List 1977 1 Independent 2 Jammaat-e-Aalia Mujahideen 3 Jamiat Ulema-e-Islam (Hazarvi) 4 Pakistan Inqlabi Mahaz 5 Pakistan Muslim League (Qayyum) 6 Pakistan National Allaince 7 Pakistan Pakhtunkhwa National Awami Party 8 Pakistan People's Party 9 Pakistan Socialist Party 10 Pakistan Worker's Party 11 Tahafuz-e-Islam Source: Gilani’s Index of Electoral Record, based on Gallup Exit Poll data and ECP data, compiled by Gallup Election Studies Team, 2013 Turn Out Election 1977 -
Province Wise Provisional Results of Census - 2017
PROVINCE WISE PROVISIONAL RESULTS OF CENSUS - 2017 ADMINISTRATIVE UNITS POPULATION 2017 POPULATION 1998 PAKISTAN 207,774,520 132,352,279 KHYBER PAKHTUNKHWA 30,523,371 17,743,645 FATA 5,001,676 3,176,331 PUNJAB 110,012,442 73,621,290 SINDH 47,886,051 30,439,893 BALOCHISTAN 12,344,408 6,565,885 ISLAMABAD 2,006,572 805,235 Note:- 1. Total Population includes all persons residing in the country including Afghans & other Aliens residing with the local population 2. Population does not include Afghan Refugees living in Refugee villages 1 PROVISIONAL CENSUS RESULTS -2017 KHYBER PAKHTUNKHWA District Tehsil POPULATION POPULATION ADMN. UNITS / AREA Sr.No Sr.No 2017 1998 KHYBER PAKHTUNKHWA 30,523,371 17,743,645 MALAKAND DIVISION 7,514,694 4,262,700 1 CHITRAL DISTRICT 447,362 318,689 1 Chitral Tehsil 278,122 184,874 2 Mastuj Tehsil 169,240 133,815 2 UPPER DIR DISTRICT 946,421 514,451 3 Dir Tehsil 439,577 235,324 4 *Shringal Tehsil 185,037 104,058 5 Wari Tehsil 321,807 175,069 3 LOWER DIR DISTRICT 1,435,917 779,056 6 Temergara Tehsil 520,738 290,849 7 *Adenzai Tehsil 317,504 168,830 8 *Lal Qilla Tehsil 219,067 129,305 9 *Samarbagh (Barwa) Tehsil 378,608 190,072 4 BUNER DISTRICT 897,319 506,048 10 Daggar/Buner Tehsil 355,692 197,120 11 *Gagra Tehsil 270,467 151,877 12 *Khado Khel Tehsil 118,185 69,812 13 *Mandanr Tehsil 152,975 87,239 5 SWAT DISTRICT 2,309,570 1,257,602 14 *Babuzai Tehsil (Swat) 599,040 321,995 15 *Bari Kot Tehsil 184,000 99,975 16 *Kabal Tehsil 420,374 244,142 17 Matta Tehsil 465,996 251,368 18 *Khawaza Khela Tehsil 265,571 141,193