Skin and Sweating Problems in Parkinson's Eople with Parkinson’S Sometimes Have Problems with Their Skin, Pand How Much Or How Little They Sweat
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Where Does Psoriasis Fit
Dr Shan Edwards Dermatologist Dermatology Clinic, Christchurch 11:00 - 11:55 WS #86: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? 12:05 - 13:00 WS #97: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? (Repeated) Differential diagnosis based on classic location Where does psoriasis fit in? Dr Shan Edwards , dermatologist Christchurch 2016 2 Conflict statement . This talk sponsored by LEO Pharma Pty Ltd . I have no other association financial or otherwise with LEO Pharma Pty Ltd 3 Acknowedgement I wish to thank and acknowledge and thank A/Prof Amanda Oakley for providing a lot of the material and allowing me to use it in this talk I would also like to acknowledge Dermnet NZ as a source for most of my clinical slides 4 How do you diagnose red scaly skin ? Take a history (90% diagnosis made on history) . When did scaly rash first appear? . What do you think caused it? . What treatments used and their effects? . Personal history of skin problems ? . Family history of similar disorders? . Occupation, hobbies, other life events? . Symptoms: itch? Other eg fever, weightloss unwell Other medical problems?(co-morbidities) . Current medicines : how long, any new ? 7 When did scaly rash first appear? . Infancy: seborrhoeic dermatitis/eczema . Toddler: atopic dermatitis/eczema . Pre-schooler/primary school: tinea capitis/corporis . Primary school: head lice . Teenage/adult: seborrhoeic dermatitis/eczema, psoriasis . Adult/elderly: drug rash, lymphoma, other less common skin conditions(PRP,Lupus) . All age groups:scabies 8 Dear Shan Re: Miss EM age 7yrs I am completely puzzled by EM’s rash and particularly so since there now appear to be other areas of her body being affected by it. -
Lupus and the Skin a Patient’S Guide to Skin Involvement in Lupus
Lupus and the Skin A Patient’s Guide to Skin Involvement in Lupus © LUPUSUK 2015 LUPUS and the Skin LUPUS UK acknowledges with gratitude the assistance of Sue Brown, Consultant Nurse in Rheumatology (Connective Tissue Diseases), Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath and Dr Chris Lovell, Consultant Dermatologist, Royal United Hospital and Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath in the provision of clinical information towards the production of this booklet. ACKNOWLEDGEMENT The authors would like to thank Professor Peter Maddison, Consultant Rheumatologist and Dr Andrew Macfarlane, Consultant Dermatologist at Ysbyty Gwynedd, Bangor, Wales, who wrote the first edition of this booklet and have kindly agreed to its revision. LUPUS UK is the national charity caring for those with systemic lupus erythematosus (SLE) and discoid lupus erythematosus (DLE), supporting people as they develop the symptoms prior to diagnosis and those already diagnosed. You can help by taking up membership For more information contact: LUPUS UK, St James House, Eastern Road, Romford, Essex RM1 3NH Tel: 01708 731251 www.lupusuk.org.uk Reg. charity nos 1051610, SC039682 © LUPUS UK 2012 All rights reserved. No part of this book may be reproduced in any form without written permission from LUPUS UK. Index Section Page No 1 Introduction 1 2 Types of rashes 2 3 Mechanism of photosensitivity 5 4 Treatment of the skin in lupus 7 5 Sun protection 10 6 Quality of life 11 7 Fatigue 12 8 Self help 12 9 Research 14 10 Further reading 14 1. Introduction Many people with lupus may have skin problems, and a rash may be the first sign of the condition. -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

The Management of Common Skin Conditions in General Practice
Management of Common Skin Conditions In General Practice including the “red rash made easy” © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care University of Auckland, Tamaki Campus Reviewed by Hon A/Prof Amanda Oakley - 2019 http://www.dermnetnz.org Management of Common Skin Conditions In General Practice Contents Page Derm Map 3 Classic location: infants & children 4 Classic location: adults 5 Dermatology terminology 6 Common red rashes 7 Other common skin conditions 12 Common viral infections 14 Common bacterial infections 16 Common fungal infections 17 Arthropods 19 Eczema/dermatitis 20 Benign skin lesions 23 Skin cancers 26 Emergency dermatology 28 Clinical diagnosis of melanoma 31 Principles of diagnosis and treatment 32 Principles of treatment of eczema 33 Treatment sequence for psoriasis 34 Topical corticosteroids 35 Combination topical steroid + antimicrobial 36 Safety with topical corticosteroids 36 Emollients 37 Antipruritics 38 For further information, refer to: http://www.dermnetnz.org And http://www.derm-master.com 2 © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care, University of Auckland, Tamaki Campus. Management of Common Skin Conditions In General Practice DERM MAP Start Is the patient sick ? Yes Rash could be an infection or a drug eruption? No Insect Bites – Crop of grouped papules with a central blister or scab. Is the patient in pain or the rash Yes Infection: cellulitis / erysipelas, impetigo, boil is swelling, oozing or crusting? / folliculitis, herpes simplex / zoster. Urticaria – Smooth skin surface with weals that evolve in minutes to hours. No Is the rash in a classic location? Yes See our classic location chart . -

Eczema of Infancy and Childhood
International Journal of Medicine Research International Journal of Medicine Research ISSN: 2455-7404; Impact Factor: RJIF 5.42 Received: 23-02-2020; Accepted: 21-03-2020; Published: 11-04-2020 www.medicinesjournal.com Volume 5; Issue 2; 2020; Page No. 21-23 Eczema of infancy and childhood Dr. Magida Kathm1, Dr. Baraa W Taha2, Dr. Nassema Lazim3 1, 2, 3 Centeral Teaching Hospital of Peadiatrics, Baghdad, Iraq Abstract Background: Eczema of infancy and childhood is one of the commom dermatological diseases in Iraqi patients for this reason this study was arranged. Objective: To assessment of an epidemiological study aimed at characterization of different clinical aspects of eczema in children and in infants in Iraqi population. Patient and Methods: A total number of tow hundred and fifty patients was seen and studied in the department of dermatology / Medical City Baghdad, FROM December 2013 to April 2014. They were 131 males and 119 female. Their ages ranged from 2 weeks to 12 years, mean age 4.43 years with mean age of onset was 3.65 years. A detailed history was taken from each patient with emphasis on the following relivant points: age, age of onset, sex, family history of atopy, personal history of atopy, history of food allergy, any associated diseases and any seasonal variations. All patients were fully examined regarding the type, morphology and distribution of the lesions in each type of eczema including: Atopic dermatitis, discoid eczema, pityriasis Alba and seborrhoeic dermatitis. The type of feeding whether breast, bottle or mixed feeding was assessed in all types of eczema. -

Health Economics and Dermatology
Extracts from the Lectures of the 32nd Nordic Congress of Dermato-Venereology, Tampere, Finland Hyperpigmentation is a common symptom but will not pro- vide much valuable information to help diagnosing the skin condition. Almost all skin diseases in dark skin can give hyper- pigmentation at some point, especially if they have a chronic or protracted course. A non-specific hyperchromia can darken the elementary lesions of the underlying dermatosis, which could mislead the physician when examining the patient. Hyperpigmentation is the main cause of consultation of dark- skinned patients but the list of causes of hyperpigmentation is countless, thus topography and additional signs should help the physician. Three conditions are of particular exception, namely acne, lichen planus and prurigo lesions in HIV patients. Hypopigmentation on the other hand is an important sign for diagnosis and hypopigmentation also severely impairs the quality of life of the patients. Causes of permanent achromia Fig. 2. Prurigo nodularis in include mainly vitiligo, post-traumatic achromia, idiopathic an HIV patients. Typical Fig. 3. Heterogenous depigmentation hypomelanosis, chronic lupus of the discoid type, and burns. annular pigmented itchy induced by skin bleaching agents. lesions with central depig- Causes of mottled hypopigmentation include vitiligo, systemic mentation. scleroderma and lichenification. Lastly, frequent causes of hypopigmentation include eczema, seborrhoeic dermatitis, pityriasis versicolor, vitiligo minor, injection or local treat- systemic complications. As users tend to hide the use of such ment of corticosteroids, achromic hamartoma, lichen striatus agents to the physician it is important to treat any underlying or verruca plana. Rare causes of hypopigmentation include skin dermatoses, disrupt bleaching agents, avoid any judge- mycosis fungoides, sarcoidosis and leprosy. -

Therapies for Common Cutaneous Fungal Infections
MedicineToday 2014; 15(6): 35-47 PEER REVIEWED FEATURE 2 CPD POINTS Therapies for common cutaneous fungal infections KENG-EE THAI MB BS(Hons), BMedSci(Hons), FACD Key points A practical approach to the diagnosis and treatment of common fungal • Fungal infection should infections of the skin and hair is provided. Topical antifungal therapies always be in the differential are effective and usually used as first-line therapy, with oral antifungals diagnosis of any scaly rash. being saved for recalcitrant infections. Treatment should be for several • Topical antifungal agents are typically adequate treatment weeks at least. for simple tinea. • Oral antifungal therapy may inea and yeast infections are among the dermatophytoses (tinea) and yeast infections be required for extensive most common diagnoses found in general and their differential diagnoses and treatments disease, fungal folliculitis and practice and dermatology. Although are then discussed (Table). tinea involving the face, hair- antifungal therapies are effective in these bearing areas, palms and T infections, an accurate diagnosis is required to ANTIFUNGAL THERAPIES soles. avoid misuse of these or other topical agents. Topical antifungal preparations are the most • Tinea should be suspected if Furthermore, subsequent active prevention is commonly prescribed agents for dermatomy- there is unilateral hand just as important as the initial treatment of the coses, with systemic agents being used for dermatitis and rash on both fungal infection. complex, widespread tinea or when topical agents feet – ‘one hand and two feet’ This article provides a practical approach fail for tinea or yeast infections. The pharmacol- involvement. to antifungal therapy for common fungal infec- ogy of the systemic agents is discussed first here. -
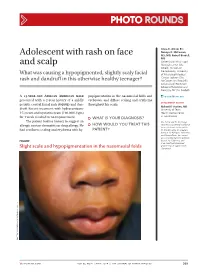
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Young Adults Young Adults (20 - 35 Years)
YOUNG ADULTS YOUNG ADULTS (20 - 35 YEARS) A large number of skin diseases reach their peak of expression during the young adult years, and these individuals also represent a large and growing proportion of the South African population, in common with other developing countries. Young adults are especially distressed by skin conditions that are uncomfortable, disfiguring or contagious. This group has also been severely affected by HIV/AIDS, with a consequent increase in the frequency and severity of the HIV- associated dermatoses. Some of these conditions have been discussed in other sections of this review. ACNE KELOIDALIS Inflammatory papules and pustules located mainly on the nape of the neck and occiput characterise this acne-like condition. It primarily affects black males. The lesions heal with scarring, creating huge keloids if this tendency exists. The cause is unknown, and unlikely to result from repeated shaving or short hair cutting. It DENGA A MAKHADO may be caused by unusually thick collagen, which traps and disrupts terminal MB ChB, FCDerm (SA) hair follicles. Treatment is not very successful, and large keloids are best excised Consultant Dermatologist by a surgeon. Mild cases can be helped by intralesional injection of steroids like Division of Dermatology Celestone Soluspan into individual papules and scars. Long-term oral tetracy- clines, as for acne, can also be beneficial, as can topical antibiotics like erythro- University of the Witwatersrand and mycin and clindamycin. Chris Hani Baragwanath Hospital Johannesburg ACNE VULGARIS Denga Anna Makhado is a consultant der- There has been a recent tendency for acne to persist beyond the teens, or even matologist at Chris Hani Baragwanath occur for the first time in adulthood, called persistent adult acne. -

Evidence-Based Danish Guidelines for the Treatment of Malassezia- Related Skin Diseases
Acta Derm Venereol 2015; 95: 12–19 SPECIAL REPORT Evidence-based Danish Guidelines for the Treatment of Malassezia- related Skin Diseases Marianne HALD1, Maiken C. ARENDRUP2, Else L. SVEJGAARD1, Rune LINDSKOV3, Erik K. FOGED4 and Ditte Marie L. SAUNTE5; On behalf of the Danish Society of Dermatology 1Department of Dermatology, Bispebjerg Hospital, University of Copenhagen, 2 Unit for Mycology, Statens Serum Institut, 3The Dermatology Clinic, Copen- hagen, 4The Dermatology Clinic, Holstebro, and 5Department of Dermatology, Roskilde Hospital, University of Copenhagen, Denmark Internationally approved guidelines for the diagnosis including those involving Malassezia (2), guidelines and management of Malassezia-related skin diseases concerning the far more common skin diseases are are lacking. Therefore, a panel of experts consisting of lacking. Therefore, a panel of experts consisting of dermatologists and a microbiologist under the auspi- dermatologists and a microbiologist appointed by the ces of the Danish Society of Dermatology undertook a Danish Society of Dermatology undertook a data review data review and compiled guidelines for the diagnostic and compiled guidelines on the diagnostic procedures procedures and management of pityriasis versicolor, se- and management of Malassezia-related skin diseases. borrhoeic dermatitis and Malassezia folliculitis. Main The ’head and neck dermatitis’, in which hypersensi- recommendations in most cases of pityriasis versicolor tivity to Malassezia is considered to be of pathogenic and seborrhoeic dermatitis include topical treatment importance, is not included in this review as it is restric- which has been shown to be sufficient. As first choice, ted to a small group of patients with atopic dermatitis. treatment should be based on topical antifungal medica- tion. -

Forum for Nordic Dermato-Venereology
Suppl. 15, Vol. 13, 2008 ISSN 1402-2915 Forum for Nordic Dermato-Venereology Official journal of the Nordic Dermatological Association 31st Nordic Congress of Dermato-Venereology May 31 – June 3, 2008 in Reykjavik, Iceland RK·FINL MA AN N D E · I D C · E N L A E N D Forum E D NDV· N W S O · R Y A Published by Society for Publication of Acta Dermato-Venereologica W http://forum.medicaljournals.se CoverAbstractboken.indd 1 2008-05-12 17:05:08 31st Nordic Congress of Dermato-Venereology May 31–June 3, 2008 in Reykjavik, Iceland Programme and Abstracts ProtopicProtopic® providespro effect effectiveive controlcon of atopic eczemaecz • FastFast rreliefelief of iitchtch1 • EffectiveEffective control ooff atopicatopic eczema2 • For short-term and intermittentin long-termlong-term treatment in adults andand cchildrenhildren (>2 yyears)ear 3 REFERENCES: 1. Reitamo S., et al. J Allergy Clin Immunol 2002;109: 539-546. 2. Reitamo S. Br. J. dermatol 2005:152:1282-89. 3. Summary of product characteristics Nov. 2006. unplugged.dk/20241/0234/04.2008 20241_Protopic_ann_man_IS_UK_210x280.indd 1 4/11/08 11:18:28 AM Table of Contents Welcome to Reykjavik 5 Congress Information 6 Floor Maps 8 Overview: Abstract Titles and Chairmen 10 Sponsors 13 Programme at a Glance 14 Abstracts in the 31st Nordic Congress of Dermato-Venereology Plenary Sessions 16 Parallel Sessions 17 Courses and Workshop 39 Posters 43 Abstract Author Index 48 Information from Nordic Dermatology Association Regulations of Nordic Dermatology Association 50 Meetings in Nordic Dermatology Association 51 Minutes from Nordic Dermatology Association 52 Economical report for 2004, 2005, 2006 och 2007 54 Necrologies 55 Members in the National Societies 57 Protopic 0.03% and 0.1% ointment (tacrolimus) *Interactions: Formal topical drug interaction studies with tacrolimus ointment have not been conducted. -

Trichoscopy Simplified Ebtisam Elghblawi*
Send Orders for Reprints to [email protected] 12 The Open Dermatology Journal, 2015, 9, 12-20 Open Access Trichoscopy Simplified Ebtisam Elghblawi* Dermatology OPD, STJTL, Tripoli, Libya Abstract: It has been a long while since skin surfaces and skin lesions have been examined by dermoscopy. However examining the hair and the scalp was done again recently and gained attention and slight popularity by the practical tool, namely trichoscopy, which can be called in a simplified way as a dermoscopy of the hair and the scalp. Trichoscopy is a great tool to examine and asses an active scalp disease and hair and other signs can be specific for some scalp and hair diseases. These signs include yellow dots, dystrophic hairs, cadaverized (black dots), white dots and exclamation mark hairs. Trichoscopy magnifies hair shafts at higher resolution to enable detailed examinations with measurements that a naked eye cannot distinguish nor see. Trichoscope is considered recently the newest frontier for the diagnosis of hair and scalp disease. Aim of this paper. The aim of this paper is to simplify and sum up the main trichoscopic readings and findings of hair and scalp disorders that are commonly encountered at clinic dermatology settings. Keywords: Dermoscopy, diagnosis, hair, hair loss, scalp dermoscopy, trichoscopy. INTRODUCTION Any dermatology clinic will be quite busy and in many instances faced with many patients mostly women complaining of hair loss, which can have significant effects on their self-esteem and quality of life. A normal terminal hair is identical in thickness and colour right through its length (Fig. 1). The width of normal hairs is usually more than 55 mm.