Unlikely Case of Submasseteric Abscess Originating from a Maxillary Molar: the Skipping Lesion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Deep Neck Infections 55
Deep Neck Infections 55 Behrad B. Aynehchi Gady Har-El Deep neck space infections (DNSIs) are a relatively penetrating trauma, surgical instrument trauma, spread infrequent entity in the postpenicillin era. Their occur- from superfi cial infections, necrotic malignant nodes, rence, however, poses considerable challenges in diagnosis mastoiditis with resultant Bezold abscess, and unknown and treatment and they may result in potentially serious causes (3–5). In inner cities, where intravenous drug or even fatal complications in the absence of timely rec- abuse (IVDA) is more common, there is a higher preva- ognition. The advent of antibiotics has led to a continu- lence of infections of the jugular vein and carotid sheath ing evolution in etiology, presentation, clinical course, and from contaminated needles (6–8). The emerging practice antimicrobial resistance patterns. These trends combined of “shotgunning” crack cocaine has been associated with with the complex anatomy of the head and neck under- retropharyngeal abscesses as well (9). These purulent col- score the importance of clinical suspicion and thorough lections from direct inoculation, however, seem to have a diagnostic evaluation. Proper management of a recog- more benign clinical course compared to those spreading nized DNSI begins with securing the airway. Despite recent from infl amed tissue (10). Congenital anomalies includ- advances in imaging and conservative medical manage- ing thyroglossal duct cysts and branchial cleft anomalies ment, surgical drainage remains a mainstay in the treat- must also be considered, particularly in cases where no ment in many cases. apparent source can be readily identifi ed. Regardless of the etiology, infection and infl ammation can spread through- Q1 ETIOLOGY out the various regions via arteries, veins, lymphatics, or direct extension along fascial planes. -
Methodical Complex on Gross Anatomy for Ii Course
MINISTRY OF HIGHER AND SECONDARY SPECIAL EDUCATION OF UZBEKISTAN BUKHARA STATE MEDICAL INSTITUTE NAMED AFTER ABU ALI IBN SINO DEPARTMENT OF ANATOMY "APPROVED" by Vice-Rector for Academic and educational work, Associate prof. G.J.Jarilkasinova ________________________________ "_____" ________________ 2020 Area of knowledge: 500000 - Health and social care Education field: 510000 - Healthcare Educational direction: 5510100 - Medical business 5111000 - Professional education (5510100 - Medicine business) 5510200 - Pediatric Medicine 5510300 - Medico-prophylactic business 5510400 – Dentistry (by directions) 5510900 – Medico-biological business EDUCATIONAL - METHODICAL COMPLEX ON GROSS ANATOMY FOR II COURSE Bukhara 2020 The scientific program was approved by the Resolution of the Coordination Council No. ___ of August ___, 2020 on the activities of educational and methodological associations in the areas of higher and secondary special and vocational education. The teaching and methodical complex was developed by order of the Ministry of Higher and Secondary Special Education of the Republic of Uzbekistan dated March 1, 2017 No. 107. Compilers: Radjabov A.B. - Head of the Department of Anatomy, Associate Professor Khasanova D.A. - Assistant of the Department of Anatomy, PhD Bobomurodov N.L. - Associate Professor of the Department of Anatomy Reviewers: Davronov R.D. - Head of the Department Histology and Medical biology, Associate Professor Djuraeva G.B. - Head of the Department of the Department of Pathological Anatomy and Judicial Medicine, Associate Professor The working educational program for anatomy is compiled on the basis of working educational curriculum and educational program for the areas of 5510100 - Medical business. This is discussed and approved at the department Protocol № ______ of "____" _______________2020 Head of the chair, associate professor: Radjabov A.B. -
Post-Operative Computed Tomography Scans in Severe Cervicofacial
Post-operative computed tomography scans in severe cervicofacial infections Yanga Ngcwama 9508272 Supervisor: Prof JA Morkel 1 CONTENTS Title 3 Declaration 4 Acknowledgements 5 Dedication 6 List of abbreviations 7 Key words 7 Abstract 8 List of tables 9 List of figures 10 1. Introduction 11 2. Literature review 12 3. Aims and objectives 24 4. Materials and methods 25 5. Results 28 6. Discussion 34 7. Conclusion 37 8. References 38 9. Annexures Annexure 1: Patient Information Letter 41 Annexure 2: Consent Form 42 Annexure 3: Patient Consent to Clinical Photography 43 Annexure 4: Data Capturing Sheet 44 2 TITLE Post-operative computed tomography scans in severe cervicofacial infections By Yanga Ngcwama Submitted in partial fulfillment (mini-thesis) for the Magister Chirurgiae Dentium (Maxillo-Facial and Oral Surgery) Department of Maxillo-Facial and Oral Surgery at the Faculty of Dentistry University of the Western Cape June 2015 3 DECLARATION I, Yanga Ngcwama, declare that this mini-thesis is my own work, that all sources I have quoted have been indicated and acknowledged by means of references, and that it has not been presented for any other degree at any university: Signed: Date: 08 October 2015. Department of Maxillo-Facial and Oral Surgery Faculty of Dentistry University of the Western Cape South Africa 4 ACKNOWLEDGEMENTS I wish to acknowledge my sincere gratitude to the following individuals for their assistance in this research project. (1) Professor J.A. Morkel, for going more than an extra mile in assisting his registrars with their training and their research projects. Long Live. (2) Professor G. -

Aetio-Pathogenesis and Clinical Pattern of Orofacial Infections
2 Aetio-Pathogenesis and Clinical Pattern of Orofacial Infections Babatunde O. Akinbami Department of Oral and Maxillofacial Surgery, University of Port Harcourt Teaching Hospital, Rivers State, Nigeria 1. Introduction Microbial induced inflammatory disease in the orofacial/head and neck region which commonly arise from odontogenic tissues, should be handled with every sense of urgency, otherwise within a short period of time, they will result in acute emergency situations.1,2 The outcome of the management of the conditions are greatly affected by the duration of the disease and extent of spread before presentation in the hospital, severity(virulence of causative organisms) of these infections as well as the presence and control of local and systemic diseases. Odontogenic tissues include 1. Hard tooth tissue 2. Periodontium 2. Predisposing factors of orofacial infections Local factors and systemic conditions that are associated with orofacial infections are listed below. Local factors Systemic factors 1. Caries, impaction, pericoronitis Human immunodeficiency virus 2. Poor oral hygiene, periodontitis Alcoholism 3. Trauma Measles, chronic malaria, tuberculosis Diabetis mellitus, hypo- and 4. Foreign body, calculi hyperthyroidism 5. Local fungal and viral infections Liver disease, renal failure, heart failure 6. Post extraction/surgery Blood dyscrasias 7. Irradiation Steroid therapy 8. Failed root canal therapy Cytotoxic drugs 9. Needle injections Excessive antibiotics, 10. Secondary infection of tumors, cyst, Malnutrition fractures 11. -
Description Concept ID Synonyms Definition
Description Concept ID Synonyms Definition Category ABNORMALITIES OF TEETH 426390 Subcategory Cementum Defect 399115 Cementum aplasia 346218 Absence or paucity of cellular cementum (seen in hypophosphatasia) Cementum hypoplasia 180000 Hypocementosis Disturbance in structure of cementum, often seen in Juvenile periodontitis Florid cemento-osseous dysplasia 958771 Familial multiple cementoma; Florid osseous dysplasia Diffuse, multifocal cementosseous dysplasia Hypercementosis (Cementation 901056 Cementation hyperplasia; Cementosis; Cementum An idiopathic, non-neoplastic condition characterized by the excessive hyperplasia) hyperplasia buildup of normal cementum (calcified tissue) on the roots of one or more teeth Hypophosphatasia 976620 Hypophosphatasia mild; Phosphoethanol-aminuria Cementum defect; Autosomal recessive hereditary disease characterized by deficiency of alkaline phosphatase Odontohypophosphatasia 976622 Hypophosphatasia in which dental findings are the predominant manifestations of the disease Pulp sclerosis 179199 Dentin sclerosis Dentinal reaction to aging OR mild irritation Subcategory Dentin Defect 515523 Dentinogenesis imperfecta (Shell Teeth) 856459 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield I 977473 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield II 976722 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; -

Severity Score As a Prognostic Factor for Management of Infections of Odontogenic Origin, a Study of 100 Cases
Open Journal of Stomatology, 2017, 7, 25-34 http://www.scirp.org/journal/ojst ISSN Online: 2160-8717 ISSN Print: 2160-8709 Severity Score as a Prognostic Factor for Management of Infections of Odontogenic Origin, a Study of 100 Cases Roman Mirochnik1*, Shareef Araidy1*, Victoria Yaffe1, Imad Abu El-Naaj1,2 1Oral and Maxillofacial Surgery Department, “Baruch Padhe” Medical Center, Poria, Israel 2Bar Ilan University, Israel How to cite this paper: Mirochnik, R., Abstract Araidy, S., Yaffe, V. and El-Naaj, I.A. (2017) Severity Score as a Prognostic Factor for Purpose: The main objective of the current study is to determine whether it is Management of Infections of Odontogenic possible to correlate the longevity of the hospitalization period (LOS) to effi- Origin, a Study of 100 Cases. Open Journal cacy of surgical treatment regime and severity scoring. Materials and Me- of Stomatology, 7, 25-34. http://dx.doi.org/10.4236/ojst.2017.71002 thods: A total of 100 patients met our inclusion criteria. All patient records, including results of hematologic and biochemical parameters, were recorded. Received: September 17, 2016 The patients were later subcategorized further according to a severity score Accepted: January 3, 2017 (“Low, Moderate, Severe”) of their main facial space involvement. The main Published: January 6, 2017 analysis of the study is a regression analysis model; all the variables (sex, age, Copyright © 2017 by authors and CRP, white blood cell count, fever, space, and etiology) were stratified ac- Scientific Research Publishing Inc. cording to the overall hospital stay. A crosstab comparison was performed This work is licensed under the Creative next; the variables were categorized and combined with hospital stay, and Commons Attribution International License (CC BY 4.0). -

A Guide to Deep Neck Space Fascial Infections for the Dental Team
Main, B. , Collin, J., Coyle, M., Hughes, C., & Thomas, S. (2017). A guide to deep neck space fascial infections for the dental team. Dental Update, 43(8), 745-752. https://doi.org/10.12968/denu.2016.43.8.745 Peer reviewed version Link to published version (if available): 10.12968/denu.2016.43.8.745 Link to publication record in Explore Bristol Research PDF-document This is the accepted author manuscript (AAM). The final published version (version of record) is available online via George Warman Publications at http://www.dental-update.co.uk/articleMatchListArticle.asp?aKey=1577. Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ Oral Surgery A guide to deep neck space fascial infections for the dental team Authors: Mr Barry Main MRCS (Ed), MFDS (Ed), MB ChB (Hons), BDS (Hons), BMSc (Hons) Doctoral Research Fellow and Honorary Specialty Registrar in Oral and Maxillofacial Surgery, School of Oral and Dental Science, University of Bristol, Lower Maudlin Street, Bristol BS1 2LY Mr John Collin BSc, MB ChB, MRCS, BDS Specialty Registrar in Oral and Maxillofacial Surgery, Division of Oral and Maxillofacial Surgery, School of Oral and Dental Science, University of Bristol, Lower Maudline Street, Bristol BS1 2LY Ms Margaret Coyle BA, -

Infection of Oral Nd Maxillofacial Surgery • Inflammation: It's Tissue Reaction to Noxious Stimuli E.G
Infection of oral nd maxillofacial surgery • Inflammation: It's tissue reaction to noxious stimuli e.g. thermal, chemical, mechanical, ....etc .In order to repair or replace the damaged tissues. • Infection: It's invasion of tissue by pathogenic micro-organisms or its toxins. • Abscess: pus accumulation in newly formed pathological cavity. • Mechanism of inflammation: • Vascular phase : Vasodilatation of the arterioles - causing hyperaemia • Extravasation of plasma rich in plasma proteins, antibodies and nutrients into the surrounding tissues • Cellular phase : • Collection of leucocytes • Leucotoxin, increases permeability allowing polymorphs into the area. •Exudate forming fibrin, walling off the region • Macrophages — phagocytosis of bacteria, dead cells. • Cardinal signs of inflammation: • Redness - Hotness - Tenderness - Swelling - Loss of function Classification of infection • According to origin • Odontogenic infection • Periapical acute dentoalveolar abscess • Pericoronitis. • Periodontitis • • Non-odontogenic • sinusitis • Sialadenitis • lymphadenitis • Trauma. • Haematogenous • iatrogenic • According to the causative organisms: • Viral • Bacterial (specific-non-specific) • Fungal infection. • According to onset, duration and severity: • Acute. • Subacute. • Chronic. • Oral cavity provides an optimum environment for microorganism growth and colonization: - • Moisture. • - Warmth. • - Protected crypts e.g. fissures, gingival crevices • Oral flora • Number of species 200 .. Number of M.O 106 109MO/cc of saliva • It contains: aerobic, -

Modified Drainage of Submasseteric Space Abscess
https://doi.org/10.5125/jkaoms.2017.43.3.197 TECHNICAL NOTE pISSN 2234-7550·eISSN 2234-5930 Modified drainage of submasseteric space abscess Moon-Gi Choi1,2 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Wonkwang University, 2Wonkwang Dental Research Institute, Wonkwang University, Iksan, Korea Abstract (J Korean Assoc Oral Maxillofac Surg 2017;43:197-203) Once a submasseteric space infection is diagnosed, the key to resolving the infection is via surgical intervention to evacuate the pus. Although it is pos- sible and occasionally practical to drain the submasseteric space via an intraoral approach, an extraoral approach may sometimes be required. Surgeons have encountered complications such as facial nerve damage during extraoral incision and drainage procedures, and they have felt that extraoral dissec- tion was very difficult. As such, an easier and simpler technique is needed. Our department recently modified various drainage techniques for submas- seteric space abscesses. Damage to the marginal branch of the facial nerve did not occur, and this technique was very simple and rapid, such that a nov- ice physician could perform this procedure. This modified technique was possible with trismus and under local anesthesia. After intraorally checking the position of the drain, the intraoral wound is closed with an absorbable suture and the drain is fixed to the extraoral skin. When a masseteric space infection is diagnosed, multiple space involvement is ruled out, and dependent drainage is required, this modified drainage technique can be useful. Key words: Submasseteric space abscess, Modified drainage [paper submitted 2016. 8. 31 / revised 2017. 1. 15 / accepted 2017. -

เรื่อง Management of Odontogenic Infection
เอกสารประกอบการสอน กระบวนวิชา DOS 408482 เรื่อง Management of odontogenic infection วัตถุประสงค : เพื่อใหนักศกษาสามารถึ 1. เพื่อใหนักศึกษามีความรู ความเขาใจในการร ักษาการติดเชื้อสาเหตุจากฟน 2. เพื่อใหนักศึกษาสามารถประยุกตความรูดังกลาวมาใชในทางคล ินิกได จัดทําโดย... อาจารย วุฒินันท จตพศุ ภาควิชาศัลยศาสตรชองปาก คณะทันตแพทยศาสตร มหาวิทยาลยเชั ียงใหม -1- Management of Odontogenic Infection การแพรกระจายของการติดเชื้อจากชองปาก 1. ทางเนื้อเยื่อเกยวพี่ ัน (connective tissue) or direct spread 2. ทางระบบไหลเวียนนาเหล้ํ ือง (lymphatic drainage) 3. ทางระบบไหลเวียนโลหิต (hematogenic spread) ลักษณะของการติดเชื้อสาเหตุจากชองปากและฟน 1. Dentoalveolar infection เชน gum boil จากโรคปริทันต 2. Maxillary sinusitis (ติดเชื้อใน maxillary sinus) 3. Fascial space infection 4. Osteomyelitis of jaw bone 5. Septicemia (systemic infection) 6. Other organs infections Fascial space infection แบงตามลักษณะกายวิภาค ดังน ี้ 1. Lower vestibular infection (vestibule of mandible) เปนการติดเชื้อทําใหเก ิดการบวมบริเวณ vestibule เปนโพรงหนองที่มี buccinator muscle เปน ขอบเขตดานลางและดานบน เปน oral mucosa อาการและอาการแสดง(sings and symptoms) : บวมบริเวณ vestibule ทาง buccal หรือ labial ตรงตําแหนงฟ นท ี่เปนสาเหต ุ กดนิ่ม หรือแข็ง มีอาการเจ็บ สาเหต ุ : Apical infection, periodontal abscess การแพรกระจาย : อาจลกลามผุ าน buccinator muscle เขาสู buccal space การผาระบายหนอง : ลง incision ตามแนวขนานกับสันเหงือก บริเวณ vestibule ที่บวม 2. Mental space infection เปนชองวางระหวางกล ามเน ื้อ mentalis และ depressor labii inferioris กับกระดูก mandible บริเวณดานหนา (symphysis) โดยอยูใตกลามเนื้อ -
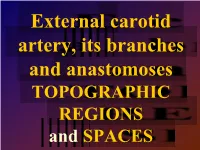
TOPOGRAPHIC REGIONS and SPACES
External carotid artery, its branches and anastomoses TOPOGRAPHIC REGIONS and SPACES branches: Arteria carotis Temporalis superficialis, maxillaris, externa ACE thyroidea sup., lingualis, pharyngea ascendens, auricularis posterior, occipitalis a. pharyngea ascendens a. STCLM For full head External carotid instead of orbit, inner artery ECA ear and brain Variety Varieties External carotid artery ECA Anterolaterally – STCLM, n. XII., glandula parotis and branches from n. VII., fascia and skin Medially – pharyngeal wall, ICA, m. stylopharyngeus a ramus pharyngealis n. X. Pro hlavu mimo očnice vnitřního ucha a mozku Superficial temporal artery for gl. parotis, TMJ, m. orbicularis oculi, m. temporalis; • rr. glandulares • a. transversa faciei (pro mimické svaly) • rr. auriculares anteriores (capsule TMJ) • a. zygomaticoorbitalis • a. temporalis media • r. frontalis • r. parietalis Arteria maxillaris – branches Three segments: Retromandibular Pterygoid Pterygopalatine Maxillary artery – retromandibular part • a. auricularis profunda • a. tympanica anterior • a. meningea media • a. alveolaris inferior Maxillary artery – pterygoid part • Superior posterior alveolar a. • Infraorbital a. • Palatine descendens a.: a. palatina major et minores a. canalis pterygoidei • a. sphenopalatina: a. nasales posteriores laterales et nasales posteriores septales Maxillary artery – branches from pterygopalatinous part Anastomoses between maxillary artery and ACI on nasal septum Internal carotid artery – intracranial branches Ophtalmic artery Facial artery For -

Space Infections
Dr. Mohit Bindal Senior Lecturer Department Of OMFS DR.MOHIT BINDAL, Subharti Dental College, SVSU CONTENTS INTRODUCTION HOST DEFENSE AND INFECTION MICROBIOLOGY AND ANTIBIOTIC THERAPY FASCIAE OF HEAD AND NECK CLASSIFICATION OF SPACES MAXILLARY SPACES MANDIBULAR SPACES SECONDARY SPACES COMPLICATIONS OVERALL MANAGEMENT STAGES OF INFECTION CONCLUSION INTRODUCTION Fascial spaces are potential spaces between the layers of fascia- Shapiro Represent major pathways for spread of infections When infections spread deeply into soft tissue- involvement following path of least resistance INFECTIONS AND HOST DEFENSE In establishing presence of an infection, interaction occurs among three factors: 1. Host 2. Environment 3. Microorganism Infection occurs when either host is immunocompromised or when pathogenecity and number of microbes invading host is more SPREAD OF OROFACIAL INFECTION FACTORS INFLUENCING SPREAD GENERAL FACTORS: Host resistance Virulence of microorganism Medically compromised LOCAL FACTORS: - Intact anatomical barriers Alveolar bone Periosteum Adjacent muscles and fascia. ANATOMICAL CONSIDERATIONS MUSCLE ATTACHMENTS- Posteriors- Buccinator- midroot level Anteriors –Intrinsic lip muscles & risorius- at apex In maxilla- infection above attachment of muscle enters extra oral space In mandible- infection below attachment of muscle enters extra oral space PREDISPOSING FACTORS 1. Dental caries or periodontal infections 2. Lowered body resistance 3. Trauma Primary signs & symptoms of these infections: - Redness - Raised temperature