Monoacylglycerol As a Metabolic Coupling Factor in Glucose-Stimulated Insulin Secretion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Curcumin, Mixture of Curcumin and Piperine and Curcum (Turmeric) on Lipid Profile of Normal and Hyperlipidemic Rats
The Egyptian Journal of Hospital Medicine Vol., 21: 145 – 161 December 2005 I.S.S.N: 12084 2002–1687 Effect of Curcumin, Mixture of Curcumin and Piperine and Curcum (Turmeric) on Lipid Profile of Normal and Hyperlipidemic Rats GHADA, Z. A. Soliman Lecturer of Biochemistry, Biochemistry Department, National Nutrition Institute, Cairo Abstract Curcumin is a polyphenolic, yellow pigment obtained from rhizomes of Curcuma longa (curcum), used as a spice and food colouring. The extracts have several pharmacological effects. We evaluated the effect of curcum, curcumin, and mixture of curcumin and piperine on plasma lipids in normal and hypercholesterolemic rats. A total of 270 rats, divided into 27 groups, were used. G1, G11: control, G2-G11: normal rats fed control diet supplemented with different levels of curcumin and curcum (G2-G6: 0.1%, 0.25%, 0.5%, 1.0%, 2.0% respectively, G7-G11: 1.67%, 4.167%, 8.34%, 16.67%, and 33.34). G12-G26: at first fed control diet supplemented with 2% cholesterol then G13-17, 21-25 fed a control diet supplemented with different levels of curcumin, and curcum [the same levels as G2-G11; G18-20 fed control diet supplemented with mixture of curcumin (0.1, 0.25, 0.5%) and piperine (20 mg/kg BW)], G12 was sacrificed before addition of studied materials, G26 were fed control diet. Lipid profile, triacylglycerol and phospholipids of plasma and organs as liver and heart were measured. Serum cholesterol (total, LDL-C, VLDL-C), triacylglycerol and phospholipids contents were elevated in cholesterol-fed rats, while HDL-C were decreased. -

Mechanistic Study of Physicochemical and Biochemical Processes
Mechanistic study of physicochemical and biochemical processes affecting intestinal absorption of the sesquiterpene lactone nobilin from multi-component systems in the Caco-2 model. Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von URSULA STEPHANIE THORMANN aus Bern (BE) Basel, 2015 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Dieses Werk ist unter dem Vertrag „Creative Commons Namensnennung-Keine kommerzielle Nutzung-Keine Bearbeitung 3.0 Schweiz“ (CC BY-NC-ND 3.0 CH) lizenziert. Die vollständige Lizenz kann unter creativecommons.org/licenses/by-nc-nd/3.0/ch/eingesehen werden. Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. G. Imanidis und Prof. Dr. H. E. U. Meyer zu Schwabedissen Basel, den 18. Februar 2014 Prof. Dr. J. Schibler Namensnennung-Keine kommerzielle Nutzung-Keine Bearbeitung 3.0 Schweiz (CC BY-NC-ND 3.0 CH) Sie dürfen: Teilen — den Inhalt kopieren, verbreiten und zugänglich machen Unter den folgenden Bedingungen: Namensnennung — Sie müssen den Namen des Autors/Rechteinhabers in der von ihm festgelegten Weise nennen. Keine kommerzielle Nutzung — Sie dürfen diesen Inhalt nicht für kommerzielle Zwecke nutzen. Keine Bearbeitung erlaubt — Sie dürfen diesen Inhalt nicht bearbeiten, abwandeln oder in anderer Weise verändern. Wobei gilt: Verzichtserklärung — Jede der vorgenannten Bedingungen kann aufgehoben werden, sofern Sie die -

Impact of Lipid Sources on Quality Traits of Medical Cannabis-Based Oil Preparations
Article Impact of Lipid Sources on Quality Traits of Medical Cannabis-Based Oil Preparations Alberto Ramella 1, Gabriella Roda 2, Radmila Pavlovic 3,*, Michele Dei Cas 4, Eleonora Casagni 2, Giacomo Mosconi 3, Francisco Cecati 5, Paola Minghetti 2 and Carlo Grizzetti 6 1 Farmacia Dott.ri Giuliana e Alberto Ramella–SAS, Via A. Diaz 1, 21021 Angera (VA), Italy; [email protected] 2 Department of Pharmaceutical Sciences, Università degli Studi di Milano, Via L. Mangiagalli 25, 20133 Milan, Italy; [email protected] (G.R.); [email protected] (E.C.); [email protected] (P.M.) 3 Department of Health, Animal Science and Food Safety, University of Milan, 20133 Milan, Italy; [email protected] 4 Department of Health Sciences, Università degli Studi di Milano, Via A.di Rudinì 8, 20142 Milan, Italy; [email protected] 5 INTEQUI-CONICET, Faculty of Chemistry, Biochemistry and Pharmacy, National University of San Luis, Almirante Brown 1455, CP 5700 San Luis, Argentina; [email protected] 6 S.S.D. Cure Palliative e Terapia del Dolore, Ospedale di Circolo–Fondazione Macchi, ASST Sette Laghi, Viale L. Borri 57, 21100 Varese, Italy; [email protected] * Correspondence: [email protected] Academic Editor: Maria Carla Marcotullio Received: 2 June 2020; Accepted: 29 June 2020; Published: 30 June 2020 Abstract: The feasibility of the use of two lipid sources and their impact on the cannabinoid profile, terpene fingerprint, and degradation products in medical cannabis oil preparations during 3 months of refrigerated storage time were investigated. LCHRMS-Orbitrap® and HS-SPME coupled to GC- MS for the investigation of targeted and untargeted cannabinoids, terpenes, and lipid degradation products in Bedrocan® and Bediol® macerated oils were used as analytical approaches. -

Phospholipid Metabolism in Stimulated Human Platelets: CHANGES in PHOSPHATIDYLINOSITOL, PHOSPHATIDIC ACID, and LYSOPHOSPHOLIPIDS
Phospholipid Metabolism in Stimulated Human Platelets: CHANGES IN PHOSPHATIDYLINOSITOL, PHOSPHATIDIC ACID, AND LYSOPHOSPHOLIPIDS M. Johan Broekman, … , Jean W. Ward, Aaron J. Marcus J Clin Invest. 1980;66(2):275-283. https://doi.org/10.1172/JCI109854. Endogenous phospholipid metabolism in stimulated human platelets was studied by phosphorus assay of major and minor components following separation by two-dimensional thin-layer chromatography. This procedure obviated the use of radioactive labels. Extensive changes were found in quantities of phosphatidylinositol (PI) and phosphatidic acid (PA) as a consequence of thrombin or collagen stimulation. Thrombin addition was followed by rapid alterations in the amount of endogenous PI and PA. The decrease in PI was not precisely reciprocated by an increase in PA when thrombin was the stimulus. This apparent discrepancy could be explained by removal of a transient intermediate in PI metabolism, such as diglyceride, formed by PI-specific phospholipase C (Rittenhouse-Simmons, S., J. Clin. Invest.63: 580-587, 1979). Diglyceride would be unavailable for PA formation by diglyceride kinase, if hydrolyzed by diglyceride lipase (Bell, R. L., D. A. Kennerly, N. Stanford, and P. W. Majerus. Proc. Natl. Acad. Sci. U. S. A.76: 3238-3241, 1979) to yield arachidonate for prostaglandin endoperoxide formation. Thrombin-treated platelets also accumulated lysophospho-glycerides. Specifically, lysophosphatidyl ethanolamines accumulated within 15s following thrombin addition. Fatty acid and aldehyde analysis indicated phospholipase A2 activity, with an apparent preference for diacyl ethanolamine phosphoglycerides. In the case of collagen, these changes occurred concomitantly with aggregation and consumption of oxygen for prostaglandin endoperoxide formation. These studies of endogenous phospholipid metabolism provide information supporting the existence of […] Find the latest version: https://jci.me/109854/pdf Phospholipid Metabolism in Stimulated Human Platelets CHANGES IN PHOSPHATIDYLINOSITOL, PHOSPHATIDIC ACID, AND LYSOPHOSPHOLIPIDS NI. -
Positive Allosteric Modulators (Pams) in Mouse Models of Overt Cannabimimetic Activity, Subjective Drug Effects, and Neuropathic Pain
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2021 Investigating Cannabinoid Type-1 Receptor (CB1R) Positive Allosteric Modulators (PAMs) in Mouse Models of Overt Cannabimimetic Activity, Subjective Drug Effects, and Neuropathic Pain Jayden Elmer Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Behavioral Neurobiology Commons, Behavior and Behavior Mechanisms Commons, Medicinal and Pharmaceutical Chemistry Commons, Nervous System Diseases Commons, and the Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/6777 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. 2021 Investigating Cannabinoid Type-1 Receptor (CB1R) Positive Allosteric Modulators (PAMs) in Mouse Models of Overt Cannabimimetic Activity, Subjective Drug Effects and Neuropathic Pain Jayden A. Elmer Investigating Cannabinoid Type-1 Receptor (CB1R) Positive Allosteric Modulators (PAMs) in Mouse Models of Overt Cannabimimetic Activity, Subjective Drug Effects and Neuropathic Pain A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Jayden Aric Elmer Bachelor of Science, University of Virginia, 2018 Director: Dr. Aron Lichtman, Professor, Department of Pharmacology & Toxicology; Associate Dean of Research and Graduate Studies, School of Pharmacy Virginia Commonwealth University Richmond, Virginia July 2021 Acknowledgements I would first like to extend my gratitude towards the CERT program at VCU. The CERT program opened the doors for me to get involved in graduate research. -
Complementary Analytical Platforms of NMR Spectroscopy and LCMS Analysis in the Metabolite Profiling of Isochrysis Galbana
marine drugs Article Complementary Analytical Platforms of NMR Spectroscopy and LCMS Analysis in the Metabolite Profiling of Isochrysis galbana Muhammad Safwan Ahamad Bustamam 1, Hamza Ahmed Pantami 2 , Awanis Azizan 1 , Khozirah Shaari 1,2, Chong Chou Min 3, Faridah Abas 1 , Norio Nagao 3, Maulidiani Maulidiani 4, Sanjoy Banerjee 1, Fadzil Sulaiman 1 and Intan Safinar Ismail 1,2,* 1 Natural Medicine and Products Research Laboratory, Institute of Bioscience, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia; [email protected] (M.S.A.B.); [email protected] (A.A.); [email protected] (K.S.); [email protected] (F.A.); [email protected] (S.B.); [email protected] (F.S.) 2 Department of Chemistry, Faculty of Science, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia; [email protected] 3 Department of Aquaculture, Faculty of Agriculture, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia; [email protected] (C.C.M.); [email protected] (N.N.) 4 Faculty of Science and Marine Environment, Universiti Malaysia Terengganu, Kuala Nerus 21030, Terengganu, Malaysia; [email protected] * Correspondence: safi[email protected]; Tel.: +60-3-9769-7492 Abstract: This study was designed to profile the metabolites of Isochrysis galbana, an indigenous and Citation: Bustamam, M.S.A.; less explored microalgae species. 1H Nuclear Magnetic Resonance (NMR) spectroscopy and Liquid Pantami, H.A.; Azizan, A.; Shaari, K.; Chromatography-Mass Spectrometry (LCMS) were used to establish the metabolite profiles of five Min, C.C.; Abas, F.; Nagao, N.; different extracts of this microalga, which are hexane (Hex), ethyl acetate (EtOAc), absolute ethanol Maulidiani, M.; Banerjee, S.; (EtOH), EtOH:water 1:1 (AqE), and 100% water (Aq). -

2010 National Ambulatory Medical Care Survey Public Use Data File
2010 NAMCS MICRO-DATA FILE DOCUMENTATION PAGE 1 ABSTRACT This material provides documentation for users of the 2010 National Ambulatory Medical Care Survey (NAMCS) public use micro-data file. NAMCS is a national probability sample survey of visits to office-based physicians conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention. It is a component of the National Health Care Surveys which measure health care utilization across a variety of health care providers. Section I, "Description of the National Ambulatory Medical Care Survey," includes information on the scope of the survey, the sample, field activities, data collection procedures, medical coding procedures, population estimates, and sampling errors. Section II provides technical information, including a detailed description of the contents of each data record by location, and a list of physician specialties represented in the survey. Section III contains marginal data and estimates for selected items on the data record. The appendixes contain sampling errors, instructions and definitions for completing the Patient Record form, and lists of codes used in the survey. PAGE 2 2010 NAMCS MICRO-DATA FILE DOCUMENTATION SUMMARY OF CHANGES FOR 2010 The 2010 NAMCS public use micro-data file is, for the most part, similar to the 2009 file, but there are some important changes. These are described in more detail below and reflect changes to the survey instruments, the Patient Record form and the Physician Induction Interview form. There are also new injury-related items on the public use file, but these are simply recoded data from existing items on the Patient Record form and are described in a separate section below. -

The Effects of Dosage-Controlled
ICTXXX10.1177/1534735419881498Integrative Cancer TherapiesBar-Sela et al 881498research-article20192019 Research Article Integrative Cancer Therapies Volume 18: 1 –8 The Effects of Dosage-Controlled © The Author(s) 2019 Article reuse guidelines: sagepub.com/journals-permissions Cannabis Capsules on Cancer-Related DOI:https://doi.org/10.1177/1534735419881498 10.1177/1534735419881498 Cachexia and Anorexia Syndrome in journals.sagepub.com/home/ict Advanced Cancer Patients: Pilot Study Gil Bar-Sela, MD1,2 , Daniela Zalman, MD3, Valerya Semenysty, MD3, and Eyal Ballan, PhD4 Abstract Background: Cancer-related cachexia and anorexia syndrome (CACS) is a common phenomenon in cancer patients. Cannabis has been suggested to stimulate appetite but research on this issue has yielded mixed results. The current study aimed to evaluate the effect of dosage-controlled cannabis capsules on CACS in advanced cancer patients. Methods: The cannabis capsules used in this study contained two fractions of oil-based compounds. The planned treatment was 2 × 10 mg per 24 hours for six months of tetrahydrocannabinol (THC) 9.5 mg and cannabidiol (CBD) 0.5 mg. If patients suffered from side effects, dosage was reduced to 5 mg × 2 per day (THC 4.75 mg, CBD 0.25 mg). Participants were weighed on every physician visit. The primary objective of the study was a weight gain of ≥10% from baseline. Results: Of 24 patients who signed the consent form, 17 started the cannabis capsules treatment, but only 11 received the capsules for more than two weeks. Three of six patients who completed the study period met the primary end-point. The remaining three patients had stable weights. -

Novel Fatty Acid Methyl Esters from the Actinomycete Micromonospora Aurantiaca
Novel fatty acid methyl esters from the actinomycete Micromonospora aurantiaca Jeroen S. Dickschat*, Hilke Bruns and Ramona Riclea Full Research Paper Open Access Address: Beilstein J. Org. Chem. 2011, 7, 1697–1712. Institut für Organische Chemie, Technische Universität Braunschweig, doi:10.3762/bjoc.7.200 Hagenring 30, 38106 Braunschweig, Germany Received: 20 August 2011 Email: Accepted: 28 November 2011 Jeroen S. Dickschat* - [email protected] Published: 20 December 2011 * Corresponding author This article is part of the Thematic Series "Biosynthesis and function of secondary metabolites". Keywords: actinomycetes; FAMEs; fatty acid biosynthesis; GC–MS; volatiles Associate Editor: S. Flitsch © 2011 Dickschat et al; licensee Beilstein-Institut. License and terms: see end of document. Abstract The volatiles released by Micromonospora aurantiaca were collected by means of a closed-loop stripping apparatus (CLSA) and analysed by GC–MS. The headspace extracts contained more than 90 compounds from different classes. Fatty acid methyl esters (FAMEs) comprised the major compound class including saturated unbranched, monomethyl and dimethyl branched FAMEs in diverse structural variants: Unbranched, α-branched, γ-branched, (ω−1)-branched, (ω−2)-branched, α- and (ω−1)-branched, γ- and (ω−1)-branched, γ- and (ω−2)-branched, and γ- and (ω−3)-branched FAMEs. FAMEs of the last three types have not been described from natural sources before. The structures for all FAMEs have been suggested based on their mass spectra and on a retention index increment system and verified by the synthesis of key reference compounds. In addition, the structures of two FAMEs, methyl 4,8-dimethyldodecanoate and the ethyl-branched compound methyl 8-ethyl-4-methyldodecanoate were deduced 2 2 2 2 from their mass spectra. -

Journal of Pharmaceutical Research Effect of Octyl Salicylate with Respect to the Physical Appearance of Mono/Di Caprylic and Capric Fatty Acids Formulations
Research Article Journal of Pharmaceutical Research Effect of Octyl Salicylate With Respect To the Physical Appearance of Mono/Di Caprylic and Capric Fatty Acids Formulations Siti Salwa Abd Gani*1,3,4, Majella E Lane2, Rabiatul Adawiah Ramli3, Mahiran Basri1,3,4 and Nor Fadzillah Mohd Mokhtar1,5 1Centre of Foundation Studies for Agricultural Science, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia * 2UCL School of Pharmacy, 29-39 Brunswick Square, London, Corresponding author WC1N 1AX, United Kingdom Siti Salwa Abd Gani, Centre of Foundation Studies for Agricultural Science, Universiti Putra Malaysia, 43400 Serdang and Selangor, 3Lapsah IPPH, Universiti Putra Malaysia, 43400Serdang, Selangor, Malaysia, Tel: +60-3-8948431; Fax: +60-3-89466997; E-mail: Malaysia [email protected] and [email protected]. 4Faculty of Science, Universiti Putra Malaysia, 43400Serdang, Submitted: 03 Nov 2016; Accepted: 17 Nov 2016; Published: 21 Nov 2016 Selangor, Malaysia 5Institute for Mathematical Research, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia Abstract Caprylic and capric acids are classified as medium-chain fatty acids. In this study, the behavior of the caprylic and capric acids formulations containing octyl salicylate were investigated. The formulations were prepared using homogenization proses. The characteristics of the formulation such as particle size, flow behavior, microscopic view and absorbance of the formulations were investigated. Particle sizes of the formulations were found ranging from 352.7 - 704.2 nm. The viscosity of the formulations changed as the shear rate was varied and could be classified as non-Newtonian fluids. The viscosity decreases when the fluid undergoes longer shear stress with time. The formulations containing octyl salicylate shows higher absorbance as compared to the formulations without octyl salicylate. -

Digestion of Dietary Fat of Dietary Digestion D
Digestion of dietary fat YouYou areare cordiallycordially invitedinvited toto attendattend thethe publicpublic defence of Digestion of dietary fat mymy thesisthesis entitledentitled Gastrointestinal behaviour of emulsions DigestionDigestion ofof dietarydietary fatfat and human physiological responses GastrointestinalGastrointestinal behaviourbehaviour ofof emulsionsemulsions andand humanhuman physiologicalphysiological responsesresponses Anne Helbig To be held on Friday, 21st June 2013, at 13:30 in the Aula of Wageningen University Generaal Foulkesweg 1, Wageningen After the graduation will be a reception in the Aula. Anne Helbig The party and the BBQ will take place at 18:30 in the garden of the SSR Generaal Foulkesweg 30, Wageningen Anne Helbig Please indicate if you would like to attend the party/BBQ by sending an email to one of my paranymphs Marijke Beenes 2013 ([email protected]) Stéphanie Ladirat ([email protected]) Digestion of dietary fat Gastrointestinal behaviour of emulsions and human physiological responses Anne Helbig Thesis committee Promoters Prof. dr. ir. H. Gruppen Professor of Food Chemistry Wageningen University Prof. dr. R.J. Hamer Professor of Technology of Cereal Proteins Wageningen University Co-promoter Dr. Erika Silletti NIZO food research, Ede Other members Prof. dr.ir. C. de Graaf, Wageningen University Prof. dr. W.H.M. Saris, Maastricht University Medical Centre Prof. P. Wilde, Norwich Research Park, UK Dr. M. Foltz, Unilever R&D, Vlaardingen This research was conducted under the auspices of the Graduate School VLAG (Advanced studies in Food Technology, Agrobiotechnology and Health Sciences). Digestion of dietary fat Gastrointestinal behaviour of emulsions and human physiological responses Anne Helbig Thesis submitted in fulfillment of the requirements for the degree of doctor at Wageningen University by the authority of the Rector Magnificus Prof. -
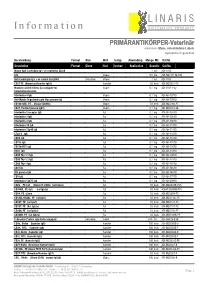
List & Label Preview File
L I N A R I S I n f o r m a t i o n B I O L O G I S C H E P R O D U K T E PRIMÄRANTIKÖRPER-Veterinär erkennen: Maus, verschiedene Labels alphabetisch geordnet Beschreibung Format Klon Wirt Isotyp Anwendung Menge ME Kat.Nr. Description Format Clone Host Isotype Application Quantity Cat.No. Mouse Anti-Cardiolipin Ig's -ve control for ELISA 1 ml ADI-5502 IgG Mouse 0,5 mg ADI-AMPT11-M-500 Anti-Cardiolipin Ig's +ve control for ELISA polyclonal Mouse 1 ml ADI-5503 CD27 PE (Armenian Hamster IgG1) Hamster 50 tests ADI-MCD027-PE Monoclonal Anti-VSV-G-Cy conjugate for Mouse 0,1 mg ADI-VSV11-Cy Immunofluorescence Interleukin-4 IgG Mouse 0,1 mg ADI-AB-10710 Anti-Myelin Oligodendrocyte Glycoprotein IgG Mouse 0,1 mg ADI-AB-19910 CD160 mAb, PE, , (mouse IgG2bk) Mouse 50 tests ADI-MCD160-PE CD81, Purified (mouse IgG1) Mouse 0,1 mg ADI-MCD081-UL Interleukin-2 receptor IgG Rat 0,1 mg ADI-AB-10310 Interleukin-2 IgG Rat 0,1 mg ADI-AB-10510 Interleukin-4 IgG Rat 0,1 mg ADI-AB-10810 Interleukin-10 IgG Rat 0,1 mg ADI-AB-11310 Interleukin-12p40 IgG Rat 0,1 mg ADI-AB-11410 CTLA-4 IgG Rat 0,1 mg ADI-AB-11610 CD80 IgG Rat 0,1 mg ADI-AB-13310 CD11a IgG Rat 0,1 mg ADI-AB-13510 CD11b-FITC IgG Rat 0,1 mg ADI-AB-13610 B220 IgG Rat 0,1 mg ADI-AB-13910 CD90 Thy-1.1 IgG Rat 0,1 mg ADI-AB-14010 CD90 Thy-1.2 IgG Rat 0,1 mg ADI-AB-14110 CD90 Thy-1 IgG Rat 0,1 mg ADI-AB-14210 CD4 IgG Rat 0,1 mg ADI-AB-16510 IFN-gamma IgG Rat 0,1 mg ADI-AB-16610 CD3 IgG Rat 0,1 mg ADI-AB-17510 Interleukin-12p75 IgG Rat 0,1 mg ADI-AB-20910 CD8b , PE-Cy5 (Clone CT-CD8b) (rat IgG2a) Rat 50 tests