Positive Allosteric Modulators (Pams) in Mouse Models of Overt Cannabimimetic Activity, Subjective Drug Effects, and Neuropathic Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Targeting the Endocannabinoid System to Reduce Nociception
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2011 Targeting the endocannabinoid system to reduce nociception Lamont Booker Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2419 This Dissertation is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. Targeting the Endocannabinoid System to Reduce Nociception A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at Virginia Commonwealth University. By Lamont Booker Bachelor’s of Science, Fayetteville State University 2003 Master’s of Toxicology, North Carolina State University 2005 Director: Dr. Aron H. Lichtman, Professor, Pharmacology & Toxicology Virginia Commonwealth University Richmond, Virginia April 2011 Acknowledgements The author wishes to thank several people. I like to thank my advisor Dr. Aron Lichtman for taking a chance and allowing me to work under his guidance. He has been a great influence not only with project and research direction, but as an excellent example of what a mentor should be (always willing to listen, understanding the needs of each student/technician, and willing to provide a hand when available). Additionally, I like to thank all of my committee members (Drs. Galya Abdrakmanova, Francine Cabral, Sandra Welch, Mike Grotewiel) for your patience and willingness to participate as a member. Our term together has truly been memorable! I owe a special thanks to Sheryol Cox, and Dr. -

S41467-020-19780-Z.Pdf
ARTICLE https://doi.org/10.1038/s41467-020-19780-z OPEN Endocannabinoid signaling regulates the reinforcing and psychostimulant effects of ketamine in mice Wei Xu1,3, Hongchun Li1,3, Liang Wang1, Jiamei Zhang1, Chunqi Liu1, Xuemei Wan1, Xiaochong Liu1, Yiming Hu1, ✉ Qiyao Fang1, Yuanyuan Xiao1, Qian Bu1, Hongbo Wang2, Jingwei Tian2, Yinglan Zhao1 & Xiaobo Cen 1 The abuse potential of ketamine limits its clinical application, but the precise mechanism remains largely unclear. Here we discovered that ketamine significantly remodels the 1234567890():,; endocannabinoid-related lipidome and activates 2-arachidonoylglycerol (2-AG) signaling in the dorsal striatum (caudate nucleus and putamen, CPu) of mice. Elevated 2-AG in the CPu is essential for the psychostimulant and reinforcing effects of ketamine, whereas blockade of the cannabinoid CB1 receptor, a predominant 2-AG receptor, attenuates ketamine-induced remodeling of neuronal dendrite structure and neurobehaviors. Ketamine represses the transcription of the monoacylglycerol lipase (MAGL) gene by promoting the expression of PRDM5, a negative transcription factor of the MAGL gene, leading to increased 2-AG pro- duction. Genetic overexpression of MAGL or silencing of PRDM5 expression in the CPu robustly reduces 2-AG production and ketamine effects. Collectively, endocannabinoid signaling plays a critical role in mediating the psychostimulant and reinforcing properties of ketamine. 1 National Chengdu Center for Safety Evaluation of Drugs, State Key Laboratory of Biotherapy/Collaborative Innovation Center for Biotherapy, West China Hospital, Sichuan University, 610041 Chengdu, People’s Republic of China. 2 Ministry of Education, Collaborative Innovation Center of Advanced Drug Delivery System and Biotech Drugs in Universities of Shandong, Yantai University, 264005 Yantai, People’s Republic of China. -

Inhibition of Monoacylglycerol Lipase Reduces the Reinstatement Of
International Journal of Neuropsychopharmacology (2019) 22(2): 165–172 doi:10.1093/ijnp/pyy086 Advance Access Publication: November 27, 2018 Regular Research Article regular research article Inhibition of Monoacylglycerol Lipase Reduces the Reinstatement of Methamphetamine-Seeking and Anxiety-Like Behaviors in Methamphetamine Self-Administered Rats Yoko Nawata, Taku Yamaguchi, Ryo Fukumori, Tsuneyuki Yamamoto Department of Pharmacology, Faculty of Pharmaceutical Science, Nagasaki International University, Nagasaki, Japan Correspondence: Tsuneyuki Yamamoto, PhD, Department of Pharmacology, Faculty of Pharmaceutical Science, Nagasaki International University, 2825–7 Huis Ten Bosch Sasebo, Nagasaki 859–3298, Japan ([email protected]). Abstract Background: Methamphetamine is a highly addictive psychostimulant with reinforcing properties. Our laboratory previously found that Δ8-tetrahydrocannabinol, an exogenous cannabinoid, suppressed the reinstatement of methamphetamine- seeking behavior. The purpose of this study was to determine whether the elevation of endocannabinoids modulates the reinstatement of methamphetamine-seeking behavior and emotional changes in methamphetamine self-administered rats. Methods: Rats were tested for the reinstatement of methamphetamine-seeking behavior following methamphetamine self- administration and extinction. The elevated plus-maze test was performed in methamphetamine self-administered rats during withdrawal. We investigated the effects of JZL184 and URB597, 2 inhibitors of endocannabinoid hydrolysis, on the reinstatement of methamphetamine-seeking and anxiety-like behaviors. Results: JZL184 (32 and 40 mg/kg, i.p.), an inhibitor of monoacylglycerol lipase, significantly attenuated both the cue- and stress-induced reinstatement of methamphetamine-seeking behavior. Furthermore, URB597 (3.2 and 10 mg/kg, i.p.), an inhibitor of fatty acid amide hydrolase, attenuated only cue-induced reinstatement. AM251, a cannabinoid CB1 receptor antagonist, antagonized the attenuation of cue-induced reinstatement by JZL184 but not URB597. -

NIH Public Access Author Manuscript Drug Alcohol Depend
NIH Public Access Author Manuscript Drug Alcohol Depend. Author manuscript; available in PMC 2015 October 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Drug Alcohol Depend. 2014 October 1; 143: 251–256. doi:10.1016/j.drugalcdep.2014.08.004. Effects of the cannabinoid CB1 receptor allosteric modulator ORG 27569 on reinstatement of cocaine- and methamphetamine- seeking behavior in rats* Li Jinga,b, Yanyan Qiua, Yanan Zhangc, and Jun-Xu Lia aDepartment of Pharmacology and Toxicology, University at Buffalo, Buffalo, New York, USA bDepartment of Physiology and Pathophysiology, Tianjin Medical University, Tianjin, China cResearch Triangle Institute, Research Triangle Park, North Carolina, USA Abstract Background—Cannabinoid CB1 receptors play an essential role in drug addiction. Given the side effect profiles of orthosteric CB1 antagonism, new strategies have been attempted to modulate this target, such as CB1 receptor allosteric modulation. However, the effect of CB1 allosteric modulation in drug addiction is unknown. The present study examined the effects of the CB1 receptor allosteric modulator ORG27569 on the reinstatement of cocaine- and methamphetamine- seeking behavior in rats. Methods—Rats were trained to self-administer 0.75 mg/kg cocaine or 0.05 mg/kg methamphetamine in 2-hr daily sessions for 14 days which was followed by 7 days of extinction sessions in which rats responded on the levers with no programmed consequences. On reinstatement test sessions, rats were administered ORG27569 (1.0, 3.2, 5.6 mg/kg, i.p.) or SR141716A (3.2 mg/kg, i.p.) 10 min prior to re-exposure to cocaine- or methamphetamine-paired cues or a priming injection of cocaine (10 mg/kg, i.p.) or methamphetamine (1 mg/kg, i.p.). -

Relevance of Peroxisome Proliferator Activated Receptors in Multitarget Paradigm Associated with the Endocannabinoid System
International Journal of Molecular Sciences Review Relevance of Peroxisome Proliferator Activated Receptors in Multitarget Paradigm Associated with the Endocannabinoid System Ana Lago-Fernandez , Sara Zarzo-Arias, Nadine Jagerovic * and Paula Morales * Medicinal Chemistry Institute, Spanish Research Council, Juan de la Cierva 3, 28006 Madrid, Spain; [email protected] (A.L.-F.); [email protected] (S.Z.-A.) * Correspondence: [email protected] (N.J.); [email protected] (P.M.); Tel.: +34-91-562-2900 (P.M.) Abstract: Cannabinoids have shown to exert their therapeutic actions through a variety of targets. These include not only the canonical cannabinoid receptors CB1R and CB2R but also related orphan G protein-coupled receptors (GPCRs), ligand-gated ion channels, transient receptor potential (TRP) channels, metabolic enzymes, and nuclear receptors. In this review, we aim to summarize reported compounds exhibiting their therapeutic effects upon the modulation of CB1R and/or CB2R and the nuclear peroxisome proliferator-activated receptors (PPARs). Concomitant actions at CBRs and PPARα or PPARγ subtypes have shown to mediate antiobesity, analgesic, antitumoral, or neuroprotective properties of a variety of phytogenic, endogenous, and synthetic cannabinoids. The relevance of this multitargeting mechanism of action has been analyzed in the context of diverse pathologies. Synergistic effects triggered by combinatorial treatment with ligands that modulate the aforementioned targets have also been considered. This literature overview provides structural and pharmacological insights for the further development of dual cannabinoids for specific disorders. Citation: Lago-Fernandez, A.; Zarzo-Arias, S.; Jagerovic, N.; Keywords: PPAR; cannabinoids; CB1R; CB2R; FAAH; multitarget; endocannabinoid system Morales, P. Relevance of Peroxisome Proliferator Activated Receptors in Multitarget Paradigm Associated with the Endocannabinoid System. -

Effect of Curcumin, Mixture of Curcumin and Piperine and Curcum (Turmeric) on Lipid Profile of Normal and Hyperlipidemic Rats
The Egyptian Journal of Hospital Medicine Vol., 21: 145 – 161 December 2005 I.S.S.N: 12084 2002–1687 Effect of Curcumin, Mixture of Curcumin and Piperine and Curcum (Turmeric) on Lipid Profile of Normal and Hyperlipidemic Rats GHADA, Z. A. Soliman Lecturer of Biochemistry, Biochemistry Department, National Nutrition Institute, Cairo Abstract Curcumin is a polyphenolic, yellow pigment obtained from rhizomes of Curcuma longa (curcum), used as a spice and food colouring. The extracts have several pharmacological effects. We evaluated the effect of curcum, curcumin, and mixture of curcumin and piperine on plasma lipids in normal and hypercholesterolemic rats. A total of 270 rats, divided into 27 groups, were used. G1, G11: control, G2-G11: normal rats fed control diet supplemented with different levels of curcumin and curcum (G2-G6: 0.1%, 0.25%, 0.5%, 1.0%, 2.0% respectively, G7-G11: 1.67%, 4.167%, 8.34%, 16.67%, and 33.34). G12-G26: at first fed control diet supplemented with 2% cholesterol then G13-17, 21-25 fed a control diet supplemented with different levels of curcumin, and curcum [the same levels as G2-G11; G18-20 fed control diet supplemented with mixture of curcumin (0.1, 0.25, 0.5%) and piperine (20 mg/kg BW)], G12 was sacrificed before addition of studied materials, G26 were fed control diet. Lipid profile, triacylglycerol and phospholipids of plasma and organs as liver and heart were measured. Serum cholesterol (total, LDL-C, VLDL-C), triacylglycerol and phospholipids contents were elevated in cholesterol-fed rats, while HDL-C were decreased. -

Cannabinoid Interventions for PTSD: Where to Next?
Accepted Manuscript Cannabinoid interventions for PTSD: Where to next? Luke Ney, Allison Matthews, Raimondo Bruno, Kim Felmingham PII: S0278-5846(19)30034-X DOI: https://doi.org/10.1016/j.pnpbp.2019.03.017 Reference: PNP 9622 To appear in: Progress in Neuropsychopharmacology & Biological Psychiatry Received date: 14 January 2019 Revised date: 20 March 2019 Accepted date: 29 March 2019 Please cite this article as: L. Ney, A. Matthews, R. Bruno, et al., Cannabinoid interventions for PTSD: Where to next?, Progress in Neuropsychopharmacology & Biological Psychiatry, https://doi.org/10.1016/j.pnpbp.2019.03.017 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT 1 Cannabinoid interventions for PTSD: Where to next? Luke Ney1, Allison Matthews1, Raimondo Bruno1 and Kim Felmingham2 1School of Psychology, University of Tasmania, Australia 2School of Psychological Sciences, University of Melbourne, Australia ACCEPTED MANUSCRIPT ACCEPTED MANUSCRIPT 2 Abstract Cannabinoids are a promising method for pharmacological treatment of post- traumatic stress disorder (PTSD). Despite considerable research devoted to the effect of cannabinoid modulation on PTSD symptomology, there is not a currently agreed way by which the cannabinoid system should be targeted in humans. In this review, we present an overview of recent research identifying neurological pathways by which different cannabinoid-based treatments may exert their effects on PTSD symptomology. -

Mechanistic Study of Physicochemical and Biochemical Processes
Mechanistic study of physicochemical and biochemical processes affecting intestinal absorption of the sesquiterpene lactone nobilin from multi-component systems in the Caco-2 model. Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von URSULA STEPHANIE THORMANN aus Bern (BE) Basel, 2015 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Dieses Werk ist unter dem Vertrag „Creative Commons Namensnennung-Keine kommerzielle Nutzung-Keine Bearbeitung 3.0 Schweiz“ (CC BY-NC-ND 3.0 CH) lizenziert. Die vollständige Lizenz kann unter creativecommons.org/licenses/by-nc-nd/3.0/ch/eingesehen werden. Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. G. Imanidis und Prof. Dr. H. E. U. Meyer zu Schwabedissen Basel, den 18. Februar 2014 Prof. Dr. J. Schibler Namensnennung-Keine kommerzielle Nutzung-Keine Bearbeitung 3.0 Schweiz (CC BY-NC-ND 3.0 CH) Sie dürfen: Teilen — den Inhalt kopieren, verbreiten und zugänglich machen Unter den folgenden Bedingungen: Namensnennung — Sie müssen den Namen des Autors/Rechteinhabers in der von ihm festgelegten Weise nennen. Keine kommerzielle Nutzung — Sie dürfen diesen Inhalt nicht für kommerzielle Zwecke nutzen. Keine Bearbeitung erlaubt — Sie dürfen diesen Inhalt nicht bearbeiten, abwandeln oder in anderer Weise verändern. Wobei gilt: Verzichtserklärung — Jede der vorgenannten Bedingungen kann aufgehoben werden, sofern Sie die -

The Enantioselective-Controlled Delivery of Propranolol by Cellulose
The Enantioselective-Controlled Delivery of Propranolol by Cellulose Membrane Grafted with Molecularly Imprinted Polymer Chatchada Bodhibukkana A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Pharmaceutical Sciences Prince of Songkla University 2008 i Copyright of Prince of Songkla University Thesis Title The Enantioselective-Controlled Delivery of Propranolol by Cellulose Membrane Grafted with Molecularly Imprinted Polymer Author Miss Chatchada Bodhibukkana Major program Pharmaceutical Sciences Major Advisor Examining Committee ………………………………………… ………………………………Chairperson (Assoc. Prof. Dr. Roongnapa Srichana) (Assoc. Prof. Dr. Ruedeekorn Wiwattanapatapee) ………………………………Committee Co-advisor (Assoc. Prof. Dr. Varaporn Junyaprasert ) ………………………………………… ………………………………Committee (Assoc. Prof. Dr. Teerapol Srichana) (Assoc. Prof. Dr. Roongnapa Srichana) ………………………………………… ………………………………Committee (Prof. Gary P. Martin) (Assoc. Prof. Dr. Teerapol Srichana) The Graduate School, Prince of Songkla University, has approved this thesis as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Pharmaceutical Sciences …………………………………………… (Assoc. Prof. Dr. Krerkchai Thongnoo) Dean of Graduate School ii propranolol !" #$ %& '(")* %&% **+, - )!,!. */*- 0 1,!2 ( 2550 ! 26 7 %8%),(9-+:%&;*,< + (composite membrane) #$ ; :%%* %&% **+, (Molecularly imprinted polymer, MIP) *& !" L* %&L* ; ; S-enantiomer ; racemic propranolol + ,: N68 +%& +N$'O !,& %&$*- #$ ") -
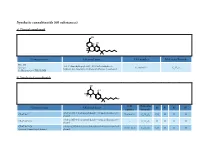
Synthetic Cannabinoids (60 Substances) A) Classical Cannabinoid
Synthetic cannabinoids (60 substances) a) Classical cannabinoid OH H OH H O Common name Chemical name CAS number Molecular Formula HU-210 3-(1,1’-dimethylheptyl)-6aR,7,10,10aR-tetrahydro-1- Synonym: 112830-95-2 C H O hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol 25 38 3 11-Hydroxy-Δ-8-THC-DMH b) Nonclassical cannabinoids OH OH R2 R3 R4 R1 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyloctan- 2- yl) CP-47,497 70434-82-1 C H O CH H H H phenol 21 34 2 3 rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylheptan- 2- yl) CP-47,497-C6 - C H O H H H H phenol 20 32 2 CP-47,497-C8 rel-2- [(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylnonan- 2- yl) 70434-92-3 C H O C H H H H Synonym: Cannabicyclohexanol phenol 22 36 2 2 5 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyldecan- 2- yl) CP-47,497-C9 - C H O C H H H H phenol 23 38 2 3 7 rel-2- ((1 R,2 R,5 R)-5- hydroxy- 2- (3- hydroxypropyl)cyclohexyl)- 3-hydroxy CP-55,940 83003-12-7 C H O CH H H 5-(2- methyloctan- 2- yl)phenol 24 40 3 3 propyl rel-2- [(1 S,3 R)-3- hydroxy-5,5-dimethylcyclohexyl]- 5- (2- Dimethyl CP-47,497-C8 - C H O C H CH CH H methylnonan-2- yl)phenol 24 40 2 2 5 3 3 c) Aminoalkylindoles i) Naphthoylindoles 1' R R3' R2' O N CAS Molecular Common name Chemical name R1’ R2’ R3’ number Formula [1-[(1- methyl- 2- piperidinyl)methyl]- 1 H-indol- 3- yl]- 1- 1-methyl-2- AM-1220 137642-54-7 C H N O H H naphthalenyl-methanone 26 26 2 piperidinyl -

Inhibition of Fatty Acid Amide Hydrolase (FAAH) by Macamides
Molecular Neurobiology (2019) 56:1770–1781 https://doi.org/10.1007/s12035-018-1115-8 Inhibition of Fatty Acid Amide Hydrolase (FAAH) by Macamides M. Alasmari1 & M. Bӧhlke1 & C. Kelley1 & T. Maher1 & A. Pino-Figueroa1 Received: 25 October 2017 /Accepted: 11 May 2018 /Published online: 20 June 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract The pentane extract of the Peruvian plant, Lepidium meyenii (Maca), has been demonstrated to possess neuroprotective activity in previous in vitro and in vivo studies (Pino-Figueroa et al. in Ann N Y Acad Sci 1199:77–85, 2010; Pino-Figueroa et al. in Am J Neuroprot Neuroregener 3:87–92, 2011). This extract contains a number of macamides that may act on the endocannabinoid system (Pino-Figueroa et al. in Ann N Y Acad Sci 1199:77–85, 2010; Pino-Figueroa et al., 2011; Dini et al. in Food Chem 49:347–349, 1994). The aim of this study was to characterize the inhibitory activity of four of these maccamides (N- benzylstearamide, N-benzyloleamide, N-benzyloctadeca-9Z,12Z-dienamide, and N-benzyloctadeca-9Z,12Z,15Z-trienamide) on fatty acid amide hydrolase (FAAH), an enzyme that is responsible for endocannabinoid degradation in the nervous system (Kumar et al. in Anaesthesia 56:1059–1068, 2001). The four compounds were tested at concentrations between 1 and 100 μM, utilizing an FAAH inhibitor screening assay. The results demonstrated concentration-dependent FAAH inhibitory activities for the four macamides tested. N-Benzyloctadeca-9Z,12Z-dienamide demonstrated the highest FAAH inhibitory activ- ity whereas N-benzylstearamide had the lowest inhibitory activity. -

Impact of Lipid Sources on Quality Traits of Medical Cannabis-Based Oil Preparations
Article Impact of Lipid Sources on Quality Traits of Medical Cannabis-Based Oil Preparations Alberto Ramella 1, Gabriella Roda 2, Radmila Pavlovic 3,*, Michele Dei Cas 4, Eleonora Casagni 2, Giacomo Mosconi 3, Francisco Cecati 5, Paola Minghetti 2 and Carlo Grizzetti 6 1 Farmacia Dott.ri Giuliana e Alberto Ramella–SAS, Via A. Diaz 1, 21021 Angera (VA), Italy; [email protected] 2 Department of Pharmaceutical Sciences, Università degli Studi di Milano, Via L. Mangiagalli 25, 20133 Milan, Italy; [email protected] (G.R.); [email protected] (E.C.); [email protected] (P.M.) 3 Department of Health, Animal Science and Food Safety, University of Milan, 20133 Milan, Italy; [email protected] 4 Department of Health Sciences, Università degli Studi di Milano, Via A.di Rudinì 8, 20142 Milan, Italy; [email protected] 5 INTEQUI-CONICET, Faculty of Chemistry, Biochemistry and Pharmacy, National University of San Luis, Almirante Brown 1455, CP 5700 San Luis, Argentina; [email protected] 6 S.S.D. Cure Palliative e Terapia del Dolore, Ospedale di Circolo–Fondazione Macchi, ASST Sette Laghi, Viale L. Borri 57, 21100 Varese, Italy; [email protected] * Correspondence: [email protected] Academic Editor: Maria Carla Marcotullio Received: 2 June 2020; Accepted: 29 June 2020; Published: 30 June 2020 Abstract: The feasibility of the use of two lipid sources and their impact on the cannabinoid profile, terpene fingerprint, and degradation products in medical cannabis oil preparations during 3 months of refrigerated storage time were investigated. LCHRMS-Orbitrap® and HS-SPME coupled to GC- MS for the investigation of targeted and untargeted cannabinoids, terpenes, and lipid degradation products in Bedrocan® and Bediol® macerated oils were used as analytical approaches.