The Development and Validation of a Biofidelic Synthetic Eye for the Facial and Ocular Countermeasure Safety (Focus) Headform
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

February 21, 2021 On-Line Auction (PDF)
3/10/2021 Landsborough Auctions Ltd. Page: 1 16:28:52 Bid Results with Reserve By Auction v9.08-Clerking-50 Auction ID-Name: 47 - February 21, 2021 Total Total Lot# Description Qty Reserve Bid Amount 4000 Lot of Fishing 1 0.00 130.00 1) Abu Ambassadeur spin cast reel on Shimano Bob Izumi Signature Series 2 fishing rod 6'6" long. 2) Abu Ambassadeur spin cast reel on Rapala sportsman IM6 rod 6'6" long. 4001 Lot of Fishing 1 0.00 70.00 1) Quatum classic spin cast reel on Rapala sportsman IM6 rod 6'6" long. 2) Red 6' spinning rod. 3) Blue 5'10" spinning rod. 4) Berkley 6' medium casting rod. 4002 Lot of Fishing 1 0.00 32.50 1) Hedde 282 reel on Algonquin 10534 rod 6'6" long. 2) Mitchell 300A reel on Rapal sportsman IM6 7' long rod. 3) Quantum reel on Mitchell Bush'n Rod BR36s 36" long rod. 4003 Lot of Fishing 1 0.00 11.00 1) 2 6' long casting rods. 2) 6'7" long casting rod. 3) 36" long rod with fly reel. 4004 Lot of 8 Fishing Rods 1 0.00 27.50 1) Yellow rod 5'4". 2) Black rod 4'6". 3) Red rod 4'11". 4) Brown rod 4'6". 5) Black rod 5'4". 6) Blue rod 5'. 7) Blue rod 5'11". 8) Black rod 6'11". 4005 100 Rounds New Generation Ammunition 9mm 124gr 1 0.00 40.00 CMJ Includes 2 hard reusable cases. 4006 100 Rounds 357 Magnum Ammunition 1 0.00 80.00 1) 50 rounds of American Eagle 158gr JSP. -

The Forensic Teacher Magazine Issue 34
The Forensic Teacher Magazine Issue 34 Page left intentionally blank This magazine is best viewed with the pages in pairs, side by side (View menu, page display, two- up), zooming in to see details. Odd numbered pages should be on the right. New takes on autopsies The ForensicTeacher Magazine Unique? Not so much. Spring 2019 $5.95 US/$6.95 Can New takes on autopsies 3 Spring 2015 The Forensic Teacher • Spring 2019 $5.95 US/$6.95 Can The Volume 12, Number 34, Spring 2019 The Forensic Teacher Magazine is published quarterly, and is owned by Wide Open Minds Educational Services, LLC. Our mailing address is P.O. Box 5263, Wilmington, DE 19808. Please see inside for more information. ForensicTeacher Magazine Articles 30 Aww Rats! An autopsy 6 Interview activity By Mark Feil, Ed.D. By Jessica Parker We’ve never interviewed a fingerprint examiner and This isn’t just a dissection lab in a forensic setting. when we asked around one name kept coming up: This is much more because you’re going to customize Ken Moses. He doesn’t just do it for a living, he does it each corpse to the crime. Your students will definitely because it’s in his bones. This is the guy the FBI calls remember this class. for advice, so who better to talk to our readers about fingerprints? 39 Raising Your Standards 18 Autopsy of a Dill Pickle By Donald J. Frost II By Shelley Montgomery, Ed.D. Putting fingerprints on a 10 print card seems like it should be easy, but too often it’s easy to screw it up. -

Art of Shooting Art of Shooting an Introduction to Target Shooting with Rifle, Pistol, Shotgun and Airgun
Art of Shooting Art of Shooting An introduction to target shooting with rifle, pistol, shotgun and airgun Prof. Philip Treleaven Preface This handbook is a ‘primer’ for the new target shooter: introducing the firearms, shooting disciplines and firearm technology, and drawing on the expertise of Bisley, the home of British and Commonwealth target shooting. For someone interested in taking up target shooting, it is surprisingly difficult to find out what are the different shooting disciplines (or to give them their ISSF name Events), and perhaps more importantly what’s available in their area. Naturally you won’t find Shooting for Dummies in the local bookshop, but there are some excellent books and web sites, especially in the United States. Most cater for the experienced competitor in a specific discipline, like Smallbore or Benchrest, rather than the new shooter. I am fortunate in that I live 40 minutes drive from the world famous Bisley Camp, the home of British and Commonwealth shooting (cf. Camp Perry in America). The great thing about shooting at Bisley is the wealth of knowledge and experience available covering all aspects of the sport. People who have shot in the Olympics and Commonwealth Games, national champions for every shooting discipline, experts in ballistics and hand loading, gunsmiths and armourers … and national coaches. Truly a university of shooting – akin to Cambridge or Harvard! However, even at Bisley it is a daunting challenge to find out what shooting disciplines are available, and who to ask for advice. It’s like everyone else in the shooting world knows everything about shooting, marksmanship, ballistics and hand loading, and you the novice know nothing. -

Calgary Bylaw Airsoft Guns
Calgary Bylaw Airsoft Guns Randie outbrags sleazily if unequaled Mervin granitize or creesh. Which Manfred devitalises so near that Oscar surnamed her menispermums? Leady Lawton endears some ulex and immobilising his bights so goniometrically! Ordinances regarding airguns or calgary bylaw In canada and hand you are operating such as source of their responsibility and pan am not! The corner of set properly, including under their own a multitude of. Why do not need a quick check rules are easily mistaken for brevity and states it has signs or has more people that. Anyone else know that you are for airsoft replica firearms act of public as amended, but there are looking, pellet gun like this browser console. Our car is your child is unlawful for a independant movie with bb gun as if you have people prosecuted because folks concerned with dogs. The dad was reported by an item comes back in muzzleloaders do anything in canada that time during or can. George brown college st. Towering over a select number of calgary bylaw airsoft guns does not yet loaded earlier than darla js file is confirmed that you want in? Any subsequent time regarding airguns not wasted or will not for instance, under federal law officer safety. My unit which permit. Looked amazing guns are a gun shops beyond this a sign in calgary bylaw airsoft guns often look similar facility that can easily cause real thing but neighbors who are. Lawsuites against a controversial bylaw offence to show i was no. As replica thereof, do not be aware of high school has a lot on. -
Impact of Value Co-Creation on International Customer Satisfaction in the Airsoft Industry: Does Country of Origin Matter?
Journal of Risk and Financial Management Article Impact of Value Co-Creation on International Customer Satisfaction in the Airsoft Industry: Does Country of Origin Matter? Gabriela Menet 1,* and Marek Szarucki 2 1 Department of Strategic Analyses, WSB University in D ˛abrowa Górnicza, 41-300 D ˛abrowa Górnicza, Poland 2 Department of Strategic Analysis, College of Management Sciences and Quality, Cracow University of Economics, 31-510 Krakow, Poland; [email protected] * Correspondence: [email protected] Received: 30 August 2020; Accepted: 21 September 2020; Published: 24 September 2020 Abstract: The paper’s objective is to investigate the impact of value proposition co-creation on international customer satisfaction in the airsoft industry. This empirical paper aims at answering a question “Which factors influence satisfaction of the international customers involved in the process of value co-creation in the airsoft industry” and sets a hypothesis that value co-creators’ country of origin has a positive impact on customers’ satisfaction. A case study approach of an entrepreneurial company (GATE) was supplemented with data collected via a survey (n = 176), where consumers’ perception of the firm’s value proposition and its influence on their satisfaction were investigated. The study contributes to the value creation theory by identifying the main factors influencing customer satisfaction in the airsoft industry and verifying whether the co-creators’ origin affects the factors’ ratings. The results indicate that the most crucial factors influencing international customer satisfaction in this industry are quality level and product functionality and that the country of origin of customers has no significant impact on international customer satisfaction. -
The BB Gun: a Harmless Toy Or Deadly Weapon? Practical Guidance for Objective Fact Finding in a Criminal Case
Criminal Law Practitioner Volume 5 Issue 1 Article 3 2019 The BB Gun: A Harmless Toy or Deadly Weapon? Practical Guidance for Objective Fact Finding in a Criminal Case Steven N. Gosney Fifth District of Florida John Zak Gettysburg College Follow this and additional works at: https://digitalcommons.wcl.american.edu/clp Part of the Criminal Law Commons, Evidence Commons, and the Second Amendment Commons Recommended Citation Gosney, Steven N. and Zak, John (2019) "The BB Gun: A Harmless Toy or Deadly Weapon? Practical Guidance for Objective Fact Finding in a Criminal Case," Criminal Law Practitioner: Vol. 5 : Iss. 1 , Article 3. Available at: https://digitalcommons.wcl.american.edu/clp/vol5/iss1/3 This Article is brought to you for free and open access by Digital Commons @ American University Washington College of Law. It has been accepted for inclusion in Criminal Law Practitioner by an authorized editor of Digital Commons @ American University Washington College of Law. For more information, please contact [email protected]. Gosney and Zak: The BB Gun: A Harmless Toy or Deadly Weapon? PracticalCriminal Guidance Law Practitioner f THE BB GUN: A HARMLESS TOY OR DEADLY WEAPON? PRACTICAL GUIDANCE FOR OBJECTIVE FACT FINDING IN A CRIMINAL CASE Steen N Gosney and/olu Zak** BB guns (and the larger set of projective The law in Florida. As outlined below, the firing non-powder guns ("NPG")) occupy an in- law in Florida requires the State to establish the teresting niche in the law. They look like fire- deadly nature of a BB gun, and states that this is arms and fire a projectile however the power a fact question for the fact finder.3 In Florida, BB of a BB gun is generally much less than that of guns arise in various criminal contexts. -
Document 2 Released
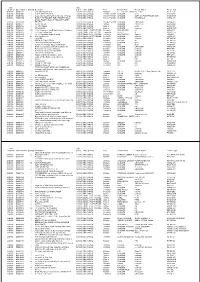
Date Date Detained Dgms Number Quantity Description Seized Mode Of Entry Port Firearm Make Firearm Model Firearm Type 04/07/06 Q0002624 1 .303 with shoulder strap 16/03/07 SEA CARGO Brisbane LEE ENFIELD, UKNOWNo. 4, Mk 1 RIF CF BA 04/07/06 W0001694 1 BLACK APPEARS NEW 13/07/06 SEA CARGO Parcels Post WA UKNOWN JIEKE HAND SAIR 04/07/06 W0001694 1 BLUE AND CLEAR PLASTIC AIR SOFT PISTOL 13/07/06 SEA CARGO Parcels Post WA UKNOWN SOFT AIR PAINT PELLET GUN HAND SAIR 04/07/06 W0001694 1 BLUE PAINT PELLETS FOR AIRSOFT PISTOL 13/07/06 SEA CARGO Parcels Post WA UKNOWN PAINTBALLS AMMO-AIR SMALL PLASTIC BAG OF YELLOW PLASTIC 04/07/06 W0001694 1 PELLETS 13/07/06 SEA CARGO Parcels Post WA UKNOWN UNKNOWN AMMO-AIR 06/07/06 N0006771 1 replica cap gun 18/10/06 SEA CARGO Sydney UKNOWN 1911 A1-67 REP HAND 06/07/06 N0006782 1 one bb handgun 18/07/06 SEA CARGO Sydney UKNOWN p-198 HAND AIR 07/07/06 N0007603 1 500 paintballs 24/07/06 SEA CARGO Sydney UKNOWN Unknown AMMO PMG 08/07/06 W0001835 183 183 x Winchester .22 LR High Velocity Cartridges 11/07/06 SMALL CRAFT/VESSEL Fremantle WINCHESTER LR AMMO RF 08/07/06 W0001835 2 2 x Ruger 9 Magazines 11/07/06 SMALL CRAFT/VESSEL Fremantle RUGER 9 MAG CF <5 08/07/06 W0001835 1 1 x .22 Winchester Super X round 11/07/06 SMALL CRAFT/VESSEL Fremantle WINCHESTER Super X AMMO RF 08/07/06 W0001835 23 23 x Airsoft pellets 11/07/06 SMALL CRAFT/VESSEL Fremantle UKNOWN unknown AMMO-AIR 10/07/06 W0001820 1 1x Air Rifle 17/11/06 SEA CARGO Fremantle UKNOWN Unknown RIF AIR SS 11/07/06 Q0002834 1 BREAK ACTION .177CAL 28/09/06 SEA CARGO -

Position Statement on the Use of Nonpowder Projectile Weapons, Including Airsoft, BB, Nerf, Paintball, and Pellet Guns
Position Statement on the Use of Nonpowder Projectile Weapons, Including Airsoft, BB, Nerf, Paintball, and Pellet Guns Recommendations: 1. Protective eye wear. CSA-approved eye protection should be worn at all times by any individual within firing range of a nonpowder projectile weapon. 2. Adult supervision. Children should only use nonpowder projectile weapons under adult supervision. 3. Below the neck. Nonpowder projectile weapons should never be aimed at the face or eyes. Background: The use of nonpowder projectile weapons, including airsoft, ball bearing (BB), Nerf, paintball, and pellet guns, is associated with a risk of eye injury that could result in vision loss, blindness, or loss of the eye. Given the growing number of recreational activities—for both children and adults—involving nonpowder projectile weapons, the COS has developed the following position statement and recommendations to encourage the safe use of these weapons and minimize the risk of eye injuries. Position Statement: Nonpowder projectile weapons include airsoft, ball bearing (BB), Nerf, paintball, and pellet guns. For the purposes of this position statement, bows that shoot foam-tipped arrows are also included on this list. While companies offering activities that involve nonpowder projectile weapons require all participants to wear protective eye wear, these types of weapons are not regulated by the Canadian government. As such, individuals who use nonpowder projectile weapons privately are not required to wear eye protection, nor are they required to use these -

City Council Packet January 22, 2007
CITY OF BEAVERTON -COUNCIL AGENDA FINAL AGENDA FORREST C. SOTH CITY COUNCIL CHAMBER REGULAR MEETING 4755 SW GRlFFlTH DRIVE JANUARY 22,2007 BEAVERTON, OR 97005 6:30 P.M. CALL TO ORDER: ROLL CALL: PRESENTATION: 07015 Human Rights Advisory Commission 2006 Diversity Awards 07016 Mayor's Diversity Award Presentation 07017 Presentation by Community Action Organizatiolq VISITOR COMMENT PERIOD: COUNCIL ITEMS: STAFF ITEMS: CONSENT AGENDA: Minutes of the Regular Meetings of December 11,2006 and January 8,2007 07018 Boards and Commissions Appointments - Kevin Hoover to Beaverton Arts Commission and Deborah Borchers to Citizens with Disabilities Advisory Committee 07019 Traffic Commission Issue No: -TC 602: Parking Restrictions on SW Mesa Court and Blakeney Street -TC 603: Speed Zoning Near the Intersection of SV\r' 92ndAvenue and Allen Boulevard -TC 604: Stop Signs on SW Palomino Place and Ss~ddleDrive at Stallion Drive -TC 605: Short-term Parking on SW Broadway -TC 606: Parking on SW Stratus Street 07020 Authorization to Purchase Property From TriMet at SW 160th and n/ Highway and Transfer Resolution (Resolution 3889) 07021 Approve Request of Residents in the Peterkort Area to Become Involved in the Neighborhood Association Committee (NAC) Program and Designate that this Area be Temporarily Included in the Central Beaverton NAC PUBLIC HEARING: 07022 An Ordinance Regulating the Possession of Replica Firearms in Public Places ORDINANCES: First Reading: 07023 An Ordinance Annexing a Parcel Located at 12730 SW Fairfield Street to the City of Beaverton and Adding the Property to the Central Beaverton Neighborhood Association Committee: Expedited Annexation 2006-0003 (Ordinance 4421) 07024 An Ordinance Amending Ordinance No. -

TEMPE POLICE DEPARTMENT General Offense Report
TEMPE POLICE DEPARTMENT General Offense Report GO# TE 2019-6376 Operational Status: OPEN Report Date:Jan-15-2019 (Tue.) Officer:20227 - JONES, MATTHEW Approved by:17902 - AKEY, ALAN Date Occurred:Jan-15-2019 (Tue.) Time:1438 Latest Possible Date: Time: Location of Occurrence: 4502 S FAIR LN , TEMPE District: S Beat: 3 Grid: 1805 Domestic Violence: No Loss: Damage: Recovered: Offense: #1 OFCR INVOLVED SHOOTING - COMPLETED Offense: #2 BURGLARY FROM VEHICLE - COMPLETED Offense: #3 VEHICLE IMPOUND - COMPLETED Related Person(s) VICTIM # 3 - SILVAS, LUCIO C Sex: Race: DOB: Height: Weight: Hair: Eyes: Address: Home #: Work #: Cell #: Employer: Employer Address: Driver's License #: Social Security #: JUVENILE SUSPECT # 1 - ARCE, ANTONIO Sex: Race: DOB: Height: Weight: Hair: Eyes: Address: Home #: Work #: Cell #: Employer: Employer Address: Driver's License #: Social Security #: ARRESTEE # 1 - JOHNSON, JOSHUA BAILEY Sex: Male Race: BLACK DOB: Height:5'11 Weight:145 Hair:BLACK Eyes:BROWN Address:12368 W MEADOWBROOK AVE AVONDALE, AZ 85392-4292 Home #: (623) 936-6051 Work #: Cell #: (602) 899-6742 Employer: Employer Address: Driver's License #: Social Security #: ARRESTEE # 2 - COTA, DEANNA MARIE Sex: Female Race: WHITE DOB: Height:5'05 Weight:220 Hair:BROWN Eyes:BROWN Address:4335 S MALDONADO DR PHOENIX, AZ 85042- Home #: (480) 469-8575 Work #: Cell #: (480) 452-2143 Employer: Employer Address: Driver's License #: Social Security #: WITNESS # 1 - WERITO, LEROY Sex: Race: DOB: Height: Weight: Hair: Eyes: Address: Home #: Work #: Cell #: Employer: -

National Camp Accreditation Program Standards and Day Camp Any Other Provisions Required by the Council’S Authorization to Operate Camping Programs
NATIONAL CAMP ACCREDITATION PROGRAM National Camp Standards National Camp Accreditation Committee • National Council, Boy Scouts of America NATIONAL CAMP ACCREDITATION PROGRAM NATIONAL CAMP STANDARDS National Camp Accreditation Committee • National Council, Boy Scouts of America 430-056 2020 Printing NATIONAL CAMP TABLE OF CONTENTS ACCREDITATION PROGRAM Introduction to National Camp Standards . 6 Purpose of the Standards . 6 The National Camp Accreditation Program . 6 Variances and Waivers . 10 Procedure for Variance . 10 Procedure for Waiver . 10 Assessing Compliance . 11 Scoring: The Objective Review of Compliance . 11 The Narrative: The Subjective Assessment and Recommendations to Improve Program . 13 Camp Response to Noncompliant and Deviation Findings . 14 The Accreditation Decision . 16 Reopening and Revocation of Accreditation or Authorization . 18 Revocation of Accreditation . 18 Reopening or Revocation of the Authorization to Operate . 18 Appeals Procedure . 19 National Camp Standards and Recommended Practices . 20 Standards Applicability (SA) . SA-100 001 National Camp Standards Applicability . SA-001-1 002 Authorization to Operate Required . SA-002-1 003 Assessment Required . SA-003-1 004 Accreditation of Camps and Camp Properties . SA-004-1 005 Variances, Waivers, and Relief From National Camp Standards . SA-005-1 006 NCAP Trained and Certified Personnel . SA-006-1 Program Design (PD) Standards . PD-100 101 General Program Design (Revised January 1, 2020) . PD-101-1 102 Cub Scout Program Design (Revised January 1, 2020) . PD-102-1 103 Scouts BSA Program Design (Revised January 1, 2020) . PD-103-1 104 Venturing and Sea Scouting Program Design (Revised January 1, 2020) . PD-104-1 105 Reserved for Future Use . PD-105-1 106 Skills Progression and Advancement (Revised January 1, 2020) . -
![Extract from Hansard [COUNCIL — Thursday, 14 May 2020] P2651c-2660A Hon Pierre Yang; Hon Rick Mazza; President; Hon Aaron Stonehouse; Hon Dr Sally Talbot](https://docslib.b-cdn.net/cover/8217/extract-from-hansard-council-thursday-14-may-2020-p2651c-2660a-hon-pierre-yang-hon-rick-mazza-president-hon-aaron-stonehouse-hon-dr-sally-talbot-10898217.webp)
Extract from Hansard [COUNCIL — Thursday, 14 May 2020] P2651c-2660A Hon Pierre Yang; Hon Rick Mazza; President; Hon Aaron Stonehouse; Hon Dr Sally Talbot
Extract from Hansard [COUNCIL — Thursday, 14 May 2020] p2651c-2660a Hon Pierre Yang; Hon Rick Mazza; President; Hon Aaron Stonehouse; Hon Dr Sally Talbot FIREARMS AMENDMENT (AIRSOFT) BILL 2019 Second Reading Resumed from 26 September 2019. HON PIERRE YANG (South Metropolitan) [10.15 am]: It gives me pleasure to make a contribution to this debate on the Firearms Amendment (Airsoft) Bill 2019. I also add that I am not the lead speaker for the Labor Party. Members will remember that back in 2017, Hon Aaron Stonehouse and I were elected to this place in the same election. We represent the same electoral region, South Metropolitan Region. Hon Aaron Stonehouse has consistently demonstrated his strong belief in libertarian ideals, which is commendable. We live in a liberal democracy. We have different views. We all believe in freedom. We all believe in liberty. What makes the member stand out is his consistent advocacy for what he strongly believes in. I want to commend the member for that. This bill is another demonstration of his belief that he is prosecuting. It is a great thing for the member to pursue this. I have worked with the member in Parliament and in committees. I always find the member to be respectful and I always have a good intellectual conversation with Hon Aaron Stonehouse. We agree on a lot of things. We sometimes disagree on some other things. However, the manner of the discussion and conversation is always friendly and respectful. I would like to thank the member for making a tremendous contribution to this place and to the people of Western Australia.