Homocysteine, Tryptophan, and Cognition in the Very Old
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Relationship Between Dietary Patterns and Depression Mediated
Khosravi et al. BMC Psychiatry (2020) 20:63 https://doi.org/10.1186/s12888-020-2455-2 RESEARCH ARTICLE Open Access The relationship between dietary patterns and depression mediated by serum levels of Folate and vitamin B12 Maryam Khosravi1,2, Gity Sotoudeh3*, Maryam Amini4*, Firoozeh Raisi5, Anahita Mansoori6 and Mahdieh Hosseinzadeh7 Abstract Background: Major depressive disorder is among main worldwide causes of disability. The low medication compliance rates in depressed patients as well as the high recurrence rate of the disease can bring up the nutrition-related factors as a potential preventive or treatment agent for depression. The aim of this study was to investigate the association between dietary patterns and depression via the intermediary role of the serum folate and vitamin B12, total homocysteine, tryptophan, and tryptophan/competing amino acids ratio. Methods: This was an individually matched case-control study in which 110 patients with depression and 220 healthy individuals, who completed a semi-quantitative food frequency questionnaire were recruited. We selected the depressed patients from three districts in Tehran through non-probable convenience sampling from which healthy individuals were selected, as well. The samples selection and data collection were performed during October 2012 to June 2013. In addition, to measure the serum biomarkers 43 patients with depression and 43 healthy people were randomly selected from the study population. To diagnose depression the criteria of Diagnostic and StatisticalManualofMentalDisorders, fourth edition, were utilized. Results: The findings suggest that the healthy dietary pattern was significantly associated with a reduced odds of depression (OR: 0.75; 95% CI: 0.61–0.93) whereas the unhealthy dietary pattern increased it (OR: 1.382, CI: 1.116–1.71). -

High Plasma Homocysteine and Low Serum Folate Levels Induced by Antiepileptic Drugs in Down Syndrome
High Plasma Homocysteine and Low Serum Folate Levels induced by Antiepileptic drugs in down Syndrome Volume 18, Number 2, 2012 Abstract IJDS Volume 1, Number 1 Clinical and epidemiological studies suggested an association between hyper-homocysteinemia (Hyper-Hcy) and cerebro- vascular disease. Experimental studies showed potential pro- Authors convulsant activity of Hcy, with several drugs commonly used to treat patients affected by neurological disorders also able to Antonio Siniscalchi,1 modify plasma Hcy levels. We assessed the effect of long-term Giovambattista De Sarro,2 AED treatment on plasma Hcy levels in patients with Down Simona Loizzo,3 syndrome (DS) and epilepsy. We also evaluated the relation- Luca Gallelli2 ship between the plasma Hcy levels, and folic acid or vitamin B12. We enrolled 15 patients in the Down syndrome with epi- 1 Department of lepsy group (DSEp, 12 men and 3 women, mean age 22 ± 12.5 Neuroscience, Neurology years old) and 15 patients in the Down syndrome without Division, “Annunziata” epilepsy group (DSControls, 12 men and 3 women, mean age Hospital, 20 ± 13.7 years old). In the DSEp group the most common Cosenza, Italy form of epilepsy was simple partial epilepsy, while the most common AED used was valproic acid. Plasma Hcy levels were 2 Department of Health Science, School of significantly higher (P < 0.01) in the DSEp group compared Medicine, University with the DSControl group. Significant differences (P < 0.01) of Catanzaro, Clinical between DSEp and DSControls were also observed in serum Pharmacology Unit, concentrations of folic acid, but not in serum levels of vitamin Mater Domini University B12. -

Insulin Resistance and Endothelial Function Are Improved After Folate
European Journal of Endocrinology (2004) 151 483–489 ISSN 0804-4643 CLINICAL STUDY Insulin resistance and endothelial function are improved after folate and vitamin B12 therapy in patients with metabolic syndrome: relationship between homocysteine levels and hyperinsulinemia Emanuela Setola, Lucilla Domenica Monti1, Elena Galluccio1, Altin Palloshi2, Gabriele Fragasso2, Rita Paroni3, Fulvio Magni4, Emilia Paola Sandoli1, Pietro Lucotti, Sabrina Costa1, Isabella Fermo3, Marzia Galli-Kienle4, Anna Origgi, Alberto Margonato2 and PierMarco Piatti Cardiovascular and Metabolic Rehabilitation Unit, Rehabilitation and Functional Reeducation Division, 1Laboratory L20, Core Laboratory, Diabetology, Endocrinology, Metabolic Disease Unit, 2Clinical Cardiology Unit, Cardiothoracic and Vascular Department, 3Department of Laboratory Medicine, Scientific Institute H. San Raffaele and 4University of Milano-Bicocca, Faculty of Medicine, Milan, Italy (Correspondence should be addressed to PM Piatti, Cardiovascular and Metabolic Rehabilitation Unit, Via Olgettina 60, 20132 Milano, Italy; Email: [email protected]) Abstract Objective: The purpose of this study was (a) to study whether a folate and vitamin B12 treatment, aimed at decreasing homocysteine levels, might ameliorate insulin resistance and endothelial dys- function in patients with metabolic syndrome according to the National Cholesterol Education Pro- gram–Adult Treatment Panel-III criteria and (b) to evaluate whether, under these metabolic conditions, there is a relationship between hyperhomocysteinemia and insulin resistance. Design and methods: A double-blind, parallel, identical placebo–drug, randomized study was per- formed for 2 months in 50 patients. Patients were randomly allocated to two groups. In group 1, patients were treated with diet plus placebo for 2 months. In group 2, patients were treated with diet plus placebo for 1 month, followed by diet plus folic acid (5 mg/day) plus vitamin B12 (500 mg/day) for another month. -

Homocysteine: a Risk Factor Worth Treating
Volume 6, No.1 2004 A CONCISE UPDATE OF IMPORTANT ISSUES CONCERNING NATURAL HEALTH INGREDIENTS Thomas G. Guilliams Ph.D. HOMOCYSTEINE: A RISK FACTOR WORTH TREATING As an emerging independent risk factor for cardiovascular disease and other aging diseases such as Alzheimer’s, homocysteine related research has generated a vast amount of literature and sparked a vigorous debate over the past decade. In fact, a comprehensive textbook is now available describing the role of homocysteine in health and disease (3). This review will survey the history of homocysteine research, the rationale for considering homocysteine as a causative agent, rather than just a marker for vascular diseases; and review the intervention trials for lowering homocysteine in patients. Homocysteine is a sulfur amino acid and a normal intermediate lesions in these individuals and he further postulated that in methionine metabolism. When excess homocysteine is made and moderately elevated homocysteine due to heterozygous mutations not readily converted into methionine or cysteine, it is excreted out of in homocysteine related genes or poor vitamin status would also lead the tightly regulated cell environment into the blood. It is the role of to increased risk of cardiovascular disease (4). the liver and kidney to remove excess homocysteine from the blood. By the early 1990’s, elevated homocysteine was being In many individuals with in-born errors of homocysteine considered an independent risk factor for cardiovascular disease metabolism, kidney or liver disease, nutrient deficiencies or (along with cholesterol and other lipid markers, age, gender, smoking concomitant ingestion of certain pharmaceuticals, homocysteine status, obesity, hypertension and diabetes). -

S-Adenosylmethionine Deficiency and Brain Accumulation of S-Adenosylhomocysteine in Thioacetamide-Induced Acute Liver Failure
nutrients Article S-Adenosylmethionine Deficiency and Brain Accumulation of S-Adenosylhomocysteine in Thioacetamide-Induced Acute Liver Failure Anna Maria Czarnecka , Wojciech Hilgier and Magdalena Zieli ´nska* Department of Neurotoxicology, Mossakowski Medical Research Centre, Polish Academy of Sciences, 5 Pawi´nskiego Street, 02-106 Warsaw, Poland; [email protected] (A.M.C.); [email protected] (W.H.) * Correspondence: [email protected]; Tel.: +48-22-6086470; Fax: +48-22-6086442 Received: 11 June 2020; Accepted: 15 July 2020; Published: 17 July 2020 Abstract: Background: Acute liver failure (ALF) impairs cerebral function and induces hepatic encephalopathy (HE) due to the accumulation of neurotoxic and neuroactive substances in the brain. Cerebral oxidative stress (OS), under control of the glutathione-based defense system, contributes to the HE pathogenesis. Glutathione synthesis is regulated by cysteine synthesized from homocysteine via the transsulfuration pathway present in the brain. The transsulfuration-transmethylation interdependence is controlled by a methyl group donor, S-adenosylmethionine (AdoMet) conversion to S-adenosylhomocysteine (AdoHcy), whose removal by subsequent hydrolysis to homocysteine counteract AdoHcy accumulation-induced OS and excitotoxicity. Methods: Rats received three consecutive intraperitoneal injections of thioacetamide (TAA) at 24 h intervals. We measured AdoMet and AdoHcy concentrations by HPLC-FD, glutathione (GSH/GSSG) ratio (Quantification kit). Results: AdoMet/AdoHcy ratio was reduced in the brain but not in the liver. The total glutathione level and GSH/GSSG ratio, decreased in TAA rats, were restored by AdoMet treatment. Conclusion: Data indicate that disturbance of redox homeostasis caused by AdoHcy in the TAA rat brain may represent a deleterious mechanism of brain damage in HE. -

Association of Methionine to Homocysteine Status with Brain Magnetic Resonance Imaging Measures and Risk of Dementia
Research JAMA Psychiatry | Original Investigation Association of Methionine to Homocysteine Status With Brain Magnetic Resonance Imaging Measures and Risk of Dementia Babak Hooshmand, MD, PhD, MPH; Helga Refsum, MD, PhD; A. David Smith, DPhil; Grégoria Kalpouzos, PhD; Francesca Mangialasche, MD, PhD; Christine A. F. von Arnim, MD; Ingemar Kåreholt, PhD; Miia Kivipelto, MD, PhD; Laura Fratiglioni, MD, PhD Supplemental content IMPORTANCE Impairment of methylation status (ie, methionine to homocysteine ratio) may be a modifiable risk factor for structural brain changes and incident dementia. OBJECTIVE To investigate the association of serum markers of methylation status and sulfur amino acids with risk of incident dementia, Alzheimer disease (AD), and the rate of total brain tissue volume loss during 6 years. DESIGN, SETTING, AND PARTICIPANTS This population-based longitudinal study was performed from March 21, 2001, to October 10, 2010, in a sample of 2570 individuals aged 60 to 102 years from the Swedish Study on Aging and Care in Kungsholmen who were dementia free at baseline and underwent comprehensive examinations and structural brain magnetic resonance imaging (MRI) on 2 to 3 occasions during 6 years. Data analysis was performed from March 1, 2018, to October 1, 2018. MAIN OUTCOMES AND MEASURES Incident dementia, AD, and the rate of total brain volume loss. RESULTS This study included 2570 individuals (mean [SD] age, 73.1 [10.4] years; 1331 [56.5%] female). The methionine to homocysteine ratio was higher in individuals who consumed vitamin supplements (median, 1.9; interquartile range [IQR], 1.5–2.6) compared with those who did not (median, 1.8; IQR, 1.3–2.3; P < .001) and increased per each quartile increase of vitamin B12 or folate. -

Blood Levels of Homocysteine and Increased Risks of Cardiovascular Disease Causal Or Casual?
REVIEW ARTICLE Blood Levels of Homocysteine and Increased Risks of Cardiovascular Disease Causal or Casual? William G. Christen, ScD; Umed A. Ajani, MBBS; Robert J. Glynn, ScD; Charles H. Hennekens, MD Background: Accumulating data from epidemiologi- load) and/or a greater frequency of elevated homocyste- cal studies suggest that individuals with elevated blood ine level in persons with cardiovascular disease as com- levels of homocysteine have increased risks of cardio- pared with persons without cardiovascular disease. Re- vascular disease. We reviewed the currently available evi- sults of most prospective studies, however, indicated dence of an association between homocysteine and car- smaller or no association. The few prospective studies diovascular disease and examined whether the strength that reported a positive association between homocys- of the evidence varies according to study design. teine level and risks of cardiovascular disease included patients with preexisting vascular disease. Methods: We used a computerized MEDLINE litera- ture search, 1966 through September 1998, to identify Conclusions: In contrast to cross-sectional and case- all epidemiological studies that examined the relation- control studies, results of prospective studies indicated ship of homocysteine level with risks of coronary heart less or no predictive ability for plasma homocysteine in or cerebrovascular disease. Two measures of plasma ho- cardiovascular disease. Instead, elevated homocysteine mocysteine level and its association with risk of cardio- level may be an acute-phase reactant that is predomi- vascular disease were extracted: mean homocysteine level nantly a marker of atherogenesis, or a consequence of in cases and controls, and relative risk of cardiovascular other factors more closely linked to risks of cardiovas- disease for elevated homocysteine level. -

Melatonin As a Reducer of Neuro- and Vasculotoxic Oxidative Stress Induced by Homocysteine
antioxidants Review Melatonin as a Reducer of Neuro- and Vasculotoxic Oxidative Stress Induced by Homocysteine Kamil Karolczak * and Cezary Watala Department of Haemostatic Disorders, Medical University of Lodz, ul. Mazowiecka 6/8, 92-215 Lodz, Poland; [email protected] * Correspondence: [email protected] Abstract: The antioxidant properties of melatonin can be successfully used to reduce the effects of oxidative stress caused by homocysteine. The beneficial actions of melatonin are mainly due to its ability to inhibit the generation of the hydroxyl radical during the oxidation of homocysteine. Melatonin protects endothelial cells, neurons, and glia against the action of oxygen radicals generated by homocysteine and prevents the structural changes in cells that lead to impaired contractility of blood vessels and neuronal degeneration. It can be, therefore, assumed that the results obtained in experiments performed mainly in the in vitro models and occasionally in animal models may clear the way to clinical applications of melatonin in patients with hyperhomocysteinemia, who exhibit a higher risk of developing neurodegenerative diseases (e.g., Parkinson’s disease or Alzheimer’s disease) and cardiovascular diseases of atherothrombotic etiology. However, the results that have been obtained so far are scarce and have seldom been performed on advanced in vivo models. All findings predominately originate from the use of in vitro models and the scarcity of clinical evidence is huge. Thus, this mini-review should be considered as a summary of the outcomes of the initial research in the field concerning the use of melatonin as a possibly efficient attenuator of oxidative Citation: Karolczak, K.; Watala, C. -
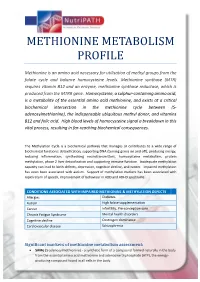
Methionine Metabolism Profile
METHIONINE METABOLISM PROFILE Methionine is an amino acid necessary for utilisation of methyl groups from the folate cycle and balance homocysteine levels. Methionine synthase (MTR) requires vitamin B12 and an enzyme, methionine synthase reductase, which is produced from the MTRR gene. Homocysteine, a sulphur-containing amino acid, is a metabolite of the essential amino acid methionine, and exists at a critical biochemical intersection in the methionine cycle between (S- adenosylmethionine), the indispensable ubiquitous methyl donor, and vitamins B12 and folic acid. High blood levels of homocysteine signal a breakdown in this vital process, resulting in far-reaching biochemical consequences. The Methylation Cycle is a biochemical pathway that manages or contributes to a wide range of biochemical functions: detoxification, supporting DNA (turning genes on and off), producing energy, reducing inflammation, synthesising neurotransmitters, homocysteine metabolism, protein methylation, phase 2 liver detoxification and supporting immune function. Inadequate methylation capacity can lead to birth defects, depression, cognitive decline, and cancer. Impaired methylation has even been associated with autism. Support of methylation markers has been associated with rapid return of speech, improvement of behaviour in ADD and ADHD spectrums. CONDITIONS ASSOCIATED WITH IMPAIRED METHIONINE & METHYLATION DEFECTS Allergies Diabetes Autism High folate supplementation Cancer Infertility, Pre-conception care Chronic Fatigue Syndrome Mental health disorders -

Folate Deficiency Was Associated with Increased Alanine Aminotransferase and Glutamyl Transpeptidase Concentrations in a Chine
J Nutr Sci Vitaminol, 62, 265–271, 2016 Folate Deficiency Was Associated with Increased Alanine Aminotransferase and Glutamyl Transpeptidase Concentrations in a Chinese Hypertensive Population: A Cross-Sectional Study Wen-Xing LI1,2, Wei LI3, Jia-Qian CAO4,5, Haiyue YAN3, Yuanyuan SUN3, Hong ZHANG3, Qiang ZHANG3, Ling TANG3, Manman WANG3, Jing-Fei HUANG2,6,7 and Dahai LIU3,* 1 Institute of Health Sciences, Anhui University, Hefei 230601, Anhui, P. R. China 2 State Key Laboratory of Genetic Resources and Evolution, Kunming Institute of Zoology, Chinese Academy of Sciences, Kunming 650223, Yunnan, P. R. China 3 Center for Stem Cell and Translational Medicine, School of Life Sciences, Anhui University, Hefei 230601, Anhui, P. R. China 4 CAS Key Laboratory of Pathogenic Microbiology & Immunology, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, P. R. China 5 University of Chinese Academy of Sciences, Beijing 100049, P. R. China 6 KIZ-SU Joint Laboratory of Animal Models and Drug Development, College of Pharmaceutical Sciences, Soochow University, Suzhou 215123, Jiangsu, P. R. China 7 Collaborative Innovation Center for Natural Products and Biological Drugs of Yunnan, Kunming 650223, Yunnan, P. R. China (Received February 29, 2016) Summary Alanine aminotransferase (ALT), aspartate transaminase (AST), and glutamyl transpeptidase (GGT) were three key enzymes in the hepatic metabolism. This study aimed to investigate the effect of homocysteine (Hcy) metabolism gene polymorphisms and serum Hcy and folate level on the hepatic functions in a Chinese hypertensive population. A repre- sentative sample with 480 subjects aged 28–75 was enrolled in 2005.9–2005.12 from six hospitals in different Chinese regions. -

Homocysteine Redux
HOMOCYSTEINE REDUX Ingredients: Trimethylglycine 300mg, Pyridoxal 5 Phosphate (enteric coated) 5mg, Vitamin B-12 200mcg, Dimethyl Glycine 25mg, Niacinamide 20mg, Cysteine 15mg, Molybdenum Chelate 30mcg, Selenium Chelate 15mcg, Vitamin B-6 (enteric coated) 15mg, Folic Acid 275mcg, Vitamin E Succinate 10i.u, Red Beet Root 25mg, Choline Bitartrate 10mg, Magnesium Chelate 100mg, Zinc Chelate 10mg. Supportive Function: Homocysteine is a toxic substance, and is slowly reaching the ranks with cholesterol as a household word associated with risk for heart disease. Faulty pathways are suspect, and Homocysteine Redux was formulated to totally support every aspect of the biochemical reactions in the pathway. When the homocysteine pathway is facilitated and functioning correctly, SAM (S-adenosyl methionine) is produced to methylate brain neurotransmitters. Natural sulfur is also produced at the end of the pathway, providing a building block for joint/connective tissue. When are homocysteine nutrients helpful? Clinical applications include decreasing risk for heart disease; atherosclerosis (hardening of the arteries), thrombosis (clots), etc., vascular, ocular, and skeletal complications, osteoporosis, depression, Fibromyalgia, alcoholism, depression, diabetic complications, Parkinson’s, Alzheimer’s, multiple sclerosis, rheumatoid arthritis, schizophrenia, spontaneous abortion, and all complications of impaired sulfation pathways, i.e. sluggish liver detoxification, adrenal problems, joint cartilage degeneration. Clinical Applications/Research: B vitamins: Many studies have now shown that supplementation of particular B vitamins, most notably folate, B-6, B-12, and niacinamide, can protect the heart by lowering homocysteine levels. These B vitamins have major roles in the pathway of homocysteine metabolism, and supplementation seems to facilitate the clearance of this potentially harmful substance. Many studies have shown decreased homocysteine levels and decreased risk for heart disease with the consumption of these B vitamins (Science News 1998; 153:105; Rosenberg IH. -

Homocysteine
Homocysteine What is homocysteine? Homocysteine is a sulphur containing amino acid that is synthesized by the body rather than ingested via diet. It is created from a process called demethylation of another amino acid, methionine and can be recycled back into methionine (a benign amino acid) or converted into cysteine (a benign amino acid with antioxidant properties) in the presence of adequate B-vitamins. Why measure homocysteine? High homocysteine levels are linked to such vascular disorders as heart disease, stroke and peripheral artery disease as well as dementia and Alzheimer’s disease. Specifically, elevated homocysteine is associated with thrombosis (blood clots) causing a 2-3 fold increase in risk of cardiovascular events. It is considered as strong of an indicator of vascular disease as smoking or hypertension. Evidence also suggests a link between elevated homocsysteine and migraines, erectile dysfunction, shortened telomeres (a marker for aging) and even age-related hearing loss. Homocysteine levels should be less than 11 umol/mL. Why is homocysteine harmful? Some research suggests that high levels of homocysteine may act as an arterial abrasive and physically damage arteries. This arterial trauma affects the endothelial lining of the arteries, which normally responds to enzymatic or hormonal cues to dilate or contract. When the endothelial lining of the blood vessels becomes dysfunctional, vascular health is seriously compromised. High homocysteine can also stem from renal disease since homocysteine is partially cleared through the kidneys. Patients with kidney disease often have very high levels of homocysteine, which some consider the primary reason that vascular disease so often coincides with renal failure.