Cutaneous Leishmaniasis in Morocco: Psychosocial Burden and Simplified Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Teaching of English As a Foreign Language in South Morocco (Tinghir Province): Descriptive and Analytical Study of Middle School and Secondary
Facultad de Ciencias de la Educación Programa Oficial de Doctorado en Formación del Profesorado TESIS DOCTORAL The Teaching of English as a Foreign Language in South Morocco (Tinghir Province): Descriptive and Analytical Study of Middle School and Secondary Souad Zakki Las Palmas de Gran Canaria 2017 Facultad de Ciencias de la Educación Programa Oficial de Doctorado en Formación del Profesorado (Bienio 2013-2014) TESIS DOCTORAL The Teaching of English as a Foreign Language in South Morocco (Tinghir Province): Descriptive and Analytical Study of Middle School and Secondary Dirigida por las doctoras: Mª Victoria Domínguez-Rodríguez Mª del Carmen Mato-Carrodeaguas La doctoranda: Souad Zakki Las Palmas de Gran Canaria 2017 Acknowledgements The completion of this PhD dissertation was possible thanks to the continued support, impulse, advice and constructive criticism provided by a number of people to whom I would like to acknowledge in the following lines. First of all, I want to express my heartfelt gratitude to my PhD supervisors at the Universidad de Las Palmas de Gran Canaria, Dr M.ª Victoria Domínguez- Rodríguez and Dr M.ª del Carmen Mato-Carrodeaguas, for guiding me throughout the development of this work, for sharing with me their expertise as researchers and educators, for showing me the right way to follow when the path in this doctoral journey was hard and stressful, and for awakening in me a real passion for Educational Technology. Second, my most sincere thanks are due to all the members of the middle and secondary schools in the Tinghir Province (Morocco) who contributed each in his/her own way to the provision and/or collection of precious information for the study. -

Monographie Regionale Beni Mellal-Khenifra 2017
Royaume du Maroc المملكة المغربية Haut-Commissariat au المندوبية السامية للتخطيط Plan MONOGRAPHIE REGIONALE BENI MELLAL-KHENIFRA 2017 Direction régionale Béni Mellal-Khénifra Table des matières INTRODUCTION ............................................................................................................ 8 PRINCIPAUX TRAITS DE LA REGION BENI MELLAL- KHENIFRA ................. 10 CHAPITRE I : MILIEU NATUREL ET DECOUPAGE ADMINISTRATIF ............ 15 1. MILIEU NATUREL ................................................................................................... 16 1.1. Reliefs ....................................................................................................................... 16 1.2. Climat ....................................................................................................................... 18 2. Découpage administratif ............................................................................................ 19 CHAPITRE II : CARACTERISTIQUES DEMOGRAPHIQUES DE LA POPULATION ........................................................................................................................ 22 1. Population ................................................................................................................... 23 1.1. Evolution et répartition spatiale de la population .................................................. 23 1.2. Densité de la population .......................................................................................... 26 1.3. Urbanisation ........................................................................................................... -
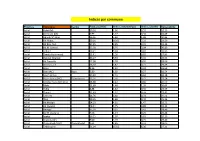
Indices Par Commune
Indices par commune Province Commune Centre Taux_pauvreté indice_volumétrique indice_séverité Vulnérabilité Azilal Azilal (M) 10,26 1,96 0,55 19,23 Azilal Demnate (M) 6,99 1,27 0,34 16,09 Azilal Agoudi N'Lkhair 26,36 5,84 1,88 30,84 Azilal Ait Abbas 50,01 16,62 7,33 23,59 Azilal Ait Bou Oulli 37,95 9,65 3,45 31,35 Azilal Ait M'Hamed 35,58 8,76 3,04 30,80 Azilal Tabant 19,21 3,24 0,81 33,95 Azilal Tamda Noumercid 15,41 2,90 0,82 27,83 Azilal Zaouiat Ahansal 35,27 9,33 3,45 28,53 Azilal Ait Taguella 17,08 3,28 0,95 28,09 Azilal Bni Hassane 16,10 2,87 0,77 29,55 Azilal Bzou 8,56 1,32 0,32 24,68 Azilal Bzou (AC) Bzou 5,80 1,02 0,27 16,54 Azilal Foum Jemaa 15,22 2,51 0,62 31,18 Azilal Foum Jemaa (AC) Foum Jemaa 13,26 2,56 0,72 22,54 Azilal Moulay Aissa Ben Driss 13,38 2,42 0,66 26,59 Azilal Rfala 21,69 4,46 1,35 30,64 Azilal Tabia 8,88 1,42 0,35 23,59 Azilal Tanant 11,63 2,12 0,59 23,41 Azilal Taounza 13,76 2,60 0,74 25,52 Azilal Tisqi 10,35 1,66 0,40 25,26 Azilal Ait Mazigh 24,23 4,91 1,47 33,72 Azilal Ait Ouqabli 18,31 3,25 0,88 33,12 Azilal Anergui 35,18 9,25 3,41 28,49 Azilal Bin El Ouidane 7,96 1,14 0,25 25,44 Azilal Isseksi 16,21 2,97 0,81 29,19 Azilal Ouaouizeght 9,00 1,19 0,25 29,46 Azilal Ouaouizeght (AC) Ouaouizeght 9,61 1,85 0,52 18,05 Azilal Tabaroucht 51,04 15,52 6,36 27,11 Province Commune Centre Taux_pauvreté indice_volumétrique indice_séverité Vulnérabilité Azilal Tagleft 27,66 6,89 2,44 26,89 Azilal Tiffert N'Ait Hamza 16,84 3,99 1,37 21,90 Azilal Tilougguite 24,10 5,32 1,70 30,13 Azilal Afourar 5,73 0,80 0,17 20,51 Azilal -

Advances in Biotechnology July 10-12, 2017 Dubai, UAE
Hmamouch Asmae et al., Adv Biochem Biotehcnol 2017, 02: 05 (Suppl) DOI: 10.29011/2574-7258-C1-003 International Conference on Advances in Biotechnology July 10-12, 2017 Dubai, UAE Contribution of biotechnology in the molecular diagnosis of cutaneous leishmaniasis at microclimates area of Boulemane and Sefrou provinces, Morocco. Hmamouch Asmae1,2, Sebti Faiza1,3, Hakkour Maryam1,4, El Alem Mohamed Mahmoud1,4, Habbari Khalid3, Fellah Hajiba1,4 and Bekhti Khadija2 1National Reference Laboratory of Leishmaniasis, National Institute of Hygiene, Rabat, Morocco 2Laboratory of Microbial Biotechnology, Sciences and Techniques Faculty, Sidi Mohammed Ben Abdellah University, Fez, Morocco 3Faculty of Sciences and Techniques, Sultan Moulay Slimane University, Beni Mellal, Morocco 4Laboratory of Zoology and General Biology, Faculty of Sciences, Mohammed V University in Rabat, Morocco Leishmaniasis is among the most important emerging vector-borne protozoal diseases in terms of disability adjusted life year (DALY’s). In Morocco, 2933 cases of CL were declared in 2015 with fluctuations in the number of cases reported over the years. As with other vector-borne diseases, the geographical distribution of cases suggests that CL transmission is sensitive to vector density which is correlated to climatic conditions. Our study target Boulemane and Sefrou provinces (among the most endemic foci of CL in Morocco) which are characterized by a diversity of microclimates area. The objectives of this study are to (i) determine the impact of the environmental conditions on the distribution of CL in these provinces, and (ii) identify the Leishmania species responsible for CL at each microclimate of these provinces using molecular techniques. Molecular characterization of parasites was performed using a previously described PCR-ITS1-RFLP method. -

Research Paper Inventory and Management of Dinosaurs Traces
International Journal of Global Science Research ISSN: 2348-8344 (Online) Vol. 5, Issue. 2, October 2018, pp. 793-814 DOI: 10.26540/ijgsr.v5.i2.2018.106 Available Online at www.ijgsr.com © Copyright 2014 | ijgsr.com | All Rights Reserved Research Paper Inventory and Management of Dinosaurs Traces: A case Study of Azilal Region, Morocco Fayçal AMINE, M’Hamed BERRAHMA and Abdellatif AARAB Mohamed V University, ENS, Department of Earth Sciences, Geosciences, Natural Resources and Development Laboratory, Avenue Mohamed Bel Hassan El Ouazzani, P.O. Box 5118 Takaddoum, Rabat, Morocco. *Corresponding author E-mail: [email protected] Received: 30/09/2018 Revised: 13/10/2018 Accepted: 18/10/2018 Abstract: The preservation of geosites in under considerations has been the scope of the heritage framework is necessary at a numerous geological studies since the 20th time when urbanization, the exploitation of Century and particularly in the past 30 years. fossils and minerals are real threats to this Recent advances have revealed that irreversible heritage. This work is a geotourism is an emerging and still contribution to the preservation and underdeveloped face of tourism, mainly in development of dinosaur trace deposits by Morocco, and mapping the geoheritage of geological and geomorphological Azilal region remains lacunars. The description of the study area, then by importance of study of geoheritage of the mapping using Geographic Information Azilal Region is related the dinosaurs traces, Systems (GIS) and finally by the proposal of worked by many paleontologists and the models of development and preservation geologists (Dresnay, 1971, 1975; Couvreur, of these geosites. 1977; Dutuit & Ouazzou, 1980; Jenny et al., Keywords: Azilal region, Morocco, 1981a,b; Laville, 1981; Monbaron, 1978, Geoheritage, Geo-Routes, GIS, Geotouristic 1980, 1981, 1982a, b, 1983; Biron, 1982; Interess Local, Dinosaurs. -

Weathering Morocco's Syria Returnees | the Washington Institute
MENU Policy Analysis / PolicyWatch 2148 Weathering Morocco's Syria Returnees by Vish Sakthivel Sep 25, 2013 ABOUT THE AUTHORS Vish Sakthivel Vish Sakthivel was a 2013-14 Next Generation Fellow at The Washington Institute. Brief Analysis The Moroccan government should be encouraged to adopt policies that preempt citizens from joining the Syrian jihad and deradicalize eventual returnees. ast week, al-Qaeda in the Islamic Maghreb (AQIM) released a video titled "Morocco: The Kingdom of Corruption L and Tyranny." In addition to pushing young Moroccans to join the jihad, the video inveighs against King Muhammad VI -- one of several public communiques in what appears to be an escalating campaign against the ruler. The timing of the video could not be more unsettling. A week before its release, against the backdrop of an increasingly insecure Sahel region, the government arrested several jihadist operatives in the northern cities of Fes, Meknes, and Taounate and the southern coastal town of Tiznit. Meanwhile, Moroccan fighters are traveling to Syria in greater numbers and forming their own jihadist groups, raising concerns about what they might do once they return home. VIDEO AND RESPONSE T he video released by al-Andalus, AQIM's media network, begins by outlining the king's alleged profiteering and corruption, citing WikiLeaks and the nonfiction book Le Roi Predateur by Catherine Graciet and Eric Laurent. It then moves to the king's close friends Mounir Majidi and Fouad Ali el-Himma, accusing them of perpetuating monopolies and patronage networks that impoverish the country while allowing the king to become one of world's richest monarchs. -

Leishmaniasis in Northern Morocco: Predominance of Leishmania Infantum Compared to Leishmania Tropica
Hindawi BioMed Research International Volume 2019, Article ID 5327287, 14 pages https://doi.org/10.1155/2019/5327287 Research Article Leishmaniasis in Northern Morocco: Predominance of Leishmania infantum Compared to Leishmania tropica Maryam Hakkour ,1,2,3 Mohamed Mahmoud El Alem ,1,2 Asmae Hmamouch,2,4 Abdelkebir Rhalem,3 Bouchra Delouane,2 Khalid Habbari,5 Hajiba Fellah ,1,2 Abderrahim Sadak ,1 and Faiza Sebti 2 1 Laboratory of Zoology and General Biology, Faculty of Sciences, Mohammed V University in Rabat, Rabat, Morocco 2National Reference Laboratory of Leishmaniasis, National Institute of Hygiene, Rabat, Morocco 3Agronomy and Veterinary Institute Hassan II, Rabat, Morocco 4Laboratory of Microbial Biotechnology, Sciences and Techniques Faculty, Sidi Mohammed Ben Abdellah University, Fez, Morocco 5Faculty of Sciences and Technics, University Sultan Moulay Slimane, Beni Mellal, Morocco Correspondence should be addressed to Maryam Hakkour; [email protected] Received 24 April 2019; Revised 17 June 2019; Accepted 1 July 2019; Published 8 August 2019 Academic Editor: Elena Pariani Copyright © 2019 Maryam Hakkour et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In Morocco, Leishmania infantum species is the main causative agents of visceral leishmaniasis (VL). However, cutaneous leishmaniasis (CL) due to L. infantum has been reported sporadically. Moreover, the recent geographical expansion of L. infantum in the Mediterranean subregion leads us to suggest whether the nonsporadic cases of CL due to this species are present. In this context, this review is written to establish a retrospective study of cutaneous and visceral leishmaniasis in northern Morocco between 1997 and 2018 and also to conduct a molecular study to identify the circulating species responsible for the recent cases of leishmaniases in this region. -

Exclusionary Development Knowledge and Accessibility in Rural Morocco
Exclusionary Development Knowledge and Accessibility in Rural Morocco by Grace Doherty B.A. in Global Studies, May 2014, University of Minnesota-Twin Cities A Thesis submitted to The Faculty of The Columbian College of Arts and Sciences of The George Washington University in partial fulfillment of the requirements for the degree of Master of Science August 31, 2017 Thesis directed by Mona Atia Associate Professor of Geography and International Affairs 1 © Copyright 2017 by Grace Doherty All rights reserved ii Dedication The author wishes to dedicate this thesis to her parents. iii Acknowledgments The author wishes to thank her advisor, Dr. Mona Atia, for her mentorship and fundamental support in navigating the international research process. She would also like to thank Dr. Marie Price and Dr. Nuala Cowan for serving on her thesis committee and for their constructive feedback throughout the course of her degree. In the field, Mr. Said Samlali was an invaluable member of the team, offering cultural guidance and arranging logistical details in Rabat and southeastern Morocco. The author also wishes to acknowledge Mr. Youssef “Noureddine” Ben Moula for his essential role as linguistic and cultural translator and Mr. Tyler Overfelt, fellow student at the George Washington University, a jack-of-all-trades in data management and qualitative fieldwork. The author also thanks fellow Geography graduate student Mr. Matthew Mittler, who made this work possible through his geospatial expertise. The GWU Humanitarian Mapping Society (HMS) provided an immense support in digitizing mapping products. Finally, the author would like to thank fellow Research Assistants Andrew Copenhaver and Forrest Melvin for their friendship and commiseration over the course of the writing. -

1/Ncerta,~;N, Ltortuhl,S Preparing Africa for a Changing Climate
1/ncerta,~;n, ltortUhl,s Preparing Africa for a changing climate 2008–09 in brief Dust storm rolls over Khartoum, Sudan Photo: Sokoine University of Agriculture Climate Change Adaptation in Africa program year in review n 2008–09 the Climate Change Adaptation in of ‘learning by doing’. It weds scientific and Africa (CCAA) program entered its third year. local knowledge to test adaptation strategies that ILaunched in 2006 by Canada’s International respond to needs identified by local people. Development Research Centre (IDRC) and the United Kingdom’s Department for International Development (DFID), the CCAA program aims to Programming directions for 2008–09 improve the capacity of African countries to adapt to climate change in ways that benefit the most This year, we focused on consolidating our invest- vulnerable. To this end, it supports three mutually ments in research and capacity building; addressing reinforcing activity strands: research; communications research and capacity gaps; and engaging more and networking; and education and training. widely with African and international audiences. Africa is among the most natural resource depen- ` We expanded our portfolio to address more areas dent regions in the world and the most exposed to of greatest vulnerability in Africa. We launched climate variability and change. CCAA supports African a call for new research on urban adaptation and researchers whose work helps communities confront approved two new projects that explore the links uncertainty. Our approach is to help them identify between water, health, and climate change. changes, pinpoint their greatest vulnerabilities, and plan CAD 7.4 million (GBP 4.15 million) 1 was invested adaptation strategies for a range of possible futures. -
Atelier Guide
Atelier Guide Atelier for Arts and Production Managers Elefsina- Beirut Module I | 24 – 28 February 2021 Index Welcome by 2023 ELEVSIS .................................................................................................................. 2 Welcome by The Festival Academy .................................................................................................... 3 Programme ......................................................................................................................................... 5 Schedule in CET/ Brussels times ......................................................................................................... 8 Facilitator, Mentors and Speakers Biographies ................................................................................ 12 Cultural programme and performances ........................................................................................... 24 Participants ....................................................................................................................................... 26 The Festival Academy ....................................................................................................................... 29 Host & co-organisers......................................................................................................................... 35 Structural Partners ......................................................................................................................... 36 1 Atelier for Young Festival Managers -

Arrêté Du Ministre De L'agriculture Et De La Pêche Maritime N° 1721
2524 BULLETIN OFFICIEL N° 6074 -27 ramadan 1433 (16-8-2012) TEXTES PARTICULIERS Arrete du ministre de !'agriculture et de la peche maritime Zidouh, Had Boumoussa et Ouled Nacer. n° 1721-12 du 26 joumada I 1433 (18 avril 2012) ART. 4. - Les caracteristiques du miel d'indication geographique portant reconnaissance de !'indication geographique « Miel d'Euphorbe Tadla Azilal » sont Jes suivantes: « Miel d'Euphorbe Tadla Azilal » et homologation du cahier des charges y afferent. 1. le miel est produit par des abeilles d'ecotype Apis mellifera spp ayant butine sur les associations vegetales naturelles et spontanees des peuplements d'Euphorbe appele LE MINISTRE DE L'AGRICULTURE ET DE LA PECHE MARITIME, scientifiquement Euphorbia resinifern de la region Tadla Azilal ; Vu la loin° 25-06, relative aux signes distinctifs d'origine 2. son odeur est de faible intensite, son arOme et sa saveur et de qualite des denrees alimentaires et des produits agricoles uniques sont specifiques a la plante d'euphorbe. II presente une et halieutiques, promulguee par le dahir n° 1-08-56 du sensation d'amertume Iegere en bouche et poivree au niveau de 17 joumada I 1429 (23 mai 2008), notamment son article 14 ; la gorge; Vu le decret n° 2-08-403 du 6 hija 1429 (5 decembre 2008) 3. le miel est de texture Iiquide ou cristallise avec une pris en application de la loi n° 25-06 relative aux signes couleur doree moyennement foncee. Lorsque le miel est distinctifs d'origine et de qualite des denrees alimentaires et des cristallis6, ii est 6pais et granuleux avec une coloration plus pale produits agricoles et halieutiques ; et claire. -

Morocco and United States Combined Government Procurement Annexes
Draft Subject to Legal Review for Accuracy, Clarity, and Consistency March 31, 2004 MOROCCO AND UNITED STATES COMBINED GOVERNMENT PROCUREMENT ANNEXES ANNEX 9-A-1 CENTRAL LEVEL GOVERNMENT ENTITIES This Chapter applies to procurement by the Central Level Government Entities listed in this Annex where the value of procurement is estimated, in accordance with Article 1:4 - Valuation, to equal or exceed the following relevant threshold. Unless otherwise specified within this Annex, all agencies subordinate to those listed are covered by this Chapter. Thresholds: (To be adjusted according to the formula in Annex 9-E) For procurement of goods and services: $175,000 [Dirham SDR conversion] For procurement of construction services: $ 6,725,000 [Dirham SDR conversion] Schedule of Morocco 1. PRIME MINISTER (1) 2. NATIONAL DEFENSE ADMINISTRATION (2) 3. GENERAL SECRETARIAT OF THE GOVERNMENT 4. MINISTRY OF JUSTICE 5. MINISTRY OF FOREIGN AFFAIRS AND COOPERATION 6. MINISTRY OF THE INTERIOR (3) 7. MINISTRY OF COMMUNICATION 8. MINISTRY OF HIGHER EDUCATION, EXECUTIVE TRAINING AND SCIENTIFIC RESEARCH 9. MINISTRY OF NATIONAL EDUCATION AND YOUTH 10. MINISTRYOF HEALTH 11. MINISTRY OF FINANCE AND PRIVATIZATION 12. MINISTRY OF TOURISM 13. MINISTRY OF MARITIME FISHERIES 14. MINISTRY OF INFRASTRUCTURE AND TRANSPORTATION 15. MINISTRY OF AGRICULTURE AND RURAL DEVELOPMENT (4) 16. MINISTRY OF SPORT 17. MINISTRY REPORTING TO THE PRIME MINISTER AND CHARGED WITH ECONOMIC AND GENERAL AFFAIRS AND WITH RAISING THE STATUS 1 Draft Subject to Legal Review for Accuracy, Clarity, and Consistency March 31, 2004 OF THE ECONOMY 18. MINISTRY OF HANDICRAFTS AND SOCIAL ECONOMY 19. MINISTRY OF ENERGY AND MINING (5) 20.