Community Health Needs Assessment 2019-2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Changing Economic Patterns in the Miami Metropolitan Area, 1940-1948
Changing Economic Patterns in the Miami Metropolitan Area, 1940-1980 By Raymond A. Mohl* The Miami metropolitan area has been a dynamic and changing urban region since World War Two. Beginning as a tourist and retirement haven, Miami developed a more diversified economy in the post-war years. Small-scale and specialized manufacturing spread during and after the 1950s. Air travel acquired a growing importance in the local economy after the war. The population of the Miami Metropolitan area (Miami SMSA) rocketed upward in the post-war era, reaching 1.6 million in 1980 - a demographic change which in turn stimulated the local construction industry for several decades. The arrival of Cuban refugees in the 1960s and 1970s helped to reshape the economy, as well. Hard-working, upwardly mobile Cubans energetically developed new business and industry, not only in Little Havana but throughout the entire metropolitan area. By the end of the 1970s Miami had emerged as an exciting center of international trade and banking. Foreign investment was pouring into the city, as was illegal drug money. Symbolic of these economic changes, new skyscraper construction in the city's central business district began to transform Miami's skyline. The city that began as a tourist playground early in the twentieth century had become by 1980 an international business center with a booming economy. Miami's tourist trade remains a vital component of the local economy. By 1940, the Miami metropolitan area was serving about two million vacationers each year - putting them up in hotels, motels, and apartments, serving them in restaurants and retail establishments, and *Dr. -

BARRY UNIVERSITY for the Southeast Florida Regional Partnership
PROJECT IDEA FROM BARRY UNIVERSITY for the Southeast Florida Regional Partnership Partnership Member General Information Partnership Member: Barry University, Inc. Membership Status: General Partner Address: 11300 NE Second Avenue, Miami Shores, Florida 33161 Main Contact Name: Patrick Lynch, Director, Office of Grant Programs Telephone: (305) 899-3072 Email / Website: [email protected] / www.barry.edu Are you part of the proposed Consultant Team respond to the SOQ? No Name of Directors / Officers: Barry University is governed by an independent, self- perpetuating Board of Trustees and is sponsored by the Sisters of St. Dominic of Adrian, Michigan. The Board is made up of 31 community leaders, higher education professionals and philanthropic patrons whose responsibility, according to the Articles of Incorporation, is to manage the business affairs of the University. Mr. William J. Heffernan, Chairman Eduardo A. Otero, MD Nelson L. Adams III, MD, Vice Chairman Mr. John Primeau Mr. Alejandro Aguirre Ms. Patricia M. Rosello Sister Linda Bevilacqua, OP, PhD, University President Donald S. Rosenberg, Esquire Mr. John M. Bussel Luigi Salvaneschi, PhD Patricia L. Clements, PhD Sister Corinne Sanders, OP, EdD Mr. Edward Feenane Joel H. Sharp, Jr., Esquire Sister Rosemary T. Finnegan, OP James Stelnicki, DPM Robert B. Galt III, Esquire Sister Sharon Weber, OP, PhD Mr. Gregory F. Greene Ms. Shirley McVay Wiseman Mr. Jorge A. Gross Christopher J. Gruchacz, CPA Reverend Charnel Jeanty Keith B. Kashuk, DPM Joseph P. Klock, Jr., Esquire Dr. Neta Kolasa Mrs. Olga Melin Charles R. Modica, JD Gerald W. Moore, Esquire Mr. Michael O. O’Neil, Jr. Ms. Maura Owens Barry University, Page 1 of 5 Number of Years in Business: 71 Overview and Form of Organization: A general overview of the Partnership and Consortium member and its staff, including form of organization. -

Authorizatino for 3Rd Party Disclosures
Completion Date: UNIVERSITY OF MIAMI Attachment 46 MILLER SCHOOL rd lJHealth Authorization for 3 Party Disclosures lHVERSITY Of MIAMI t£ALJH SYSTEM of MEDICINE I authorize the use or disclosure of health information about me as described below. 1. Person(s) or class of persons authorized to use or disclose the information (e.g., UHealth medical records, physician): _______________________________________________________________________________________________________ 2. Person(s) or class of persons authorized to receive the information (e.g., name & relationship: family, attorney, employer, etc.): ___________________________________________________________________________________________________________ If you would like your records to be sent to a third party, please provide an address or fax where you would like us to send the information. Please attach additional pages if more than one third party. Name: ____________________________________________ Address: __________________________________________ City: _____________________________________________ State: ______________________ Zip: _________________ Phone: _____________________________________________ Fax: _____________________________________________ 3. Description of information that may be used or disclosed (e.g., all information related to a specific type of treatment): ___________________________________________________________________________________________________________ ___________________________________________________________________________________________________________ -

Miami-Miami Beach-Kendall, Florida
HUD PD&R Housing Market Profiles Miami-Miami Beach-Kendall, Florida Quick Facts About Miami-Miami Beach-Kendall By T. Michael Miller | As of June 1, 2019 Current sales market conditions: balanced Overview Current apartment market conditions: balanced The Miami-Miami Beach-Kendall Metropolitan Division (hereafter, Miami-Dade County), on the southeastern coast of Florida, is Known as a destination for beautiful beaches coterminous with Miami-Dade County. The coastal location makes and eclectic nightlife, the Miami HMA attracted Miami-Dade County an attractive destination for trade and tourism. an estimated 15.9 million visitors in 2017, which During 2018, nearly 8.78 million tons of cargo passed through had an economic impact of more than $38.9 PortMiami, an increase of 2 percent from 2017. The number of billion on the HMA’s economy (Greater Miami cruise passengers out of PortMiami also hit record highs, with Convention & Visitors Bureau). 5.3 million passengers sailing during 2017, up nearly 5 percent from 2016 (Greater Miami Convention & Visitors Bureau). y As of June 1, 2019, the population of Miami-Dade County is estimated at 2.79 million, reflecting an average annual increase of 24,000, or 0.9 percent, since 2016 (U.S. Census Bureau population estimates as of July 1). Net in-migration averaged 9,050 people annually during the period, accounting for 38 percent of the population growth. y From 2011 to 2016, population growth was more rapid because of stronger international in-migration. Population growth averaged 30,550 people, or 1.2 percent, annually, and net in-migration averaged 17,900 people annually, which was 59 percent of the growth. -

Resume-January. 2020
Phone: 305.628.6635 Email: [email protected] Dr. Hagai Gringarten Selected Achievements • Founder, Publisher and Editor-in-Chief of the Journal of Multidisciplinary Research (JMR), an academic peer reviewed research journal, indexed by premier international partners such as ProQuest, Cabells, EBSCO, and Gale- Cengage. Improved brand recognition, increased exposure, created additional Web traffic, and increased the quality of published academic research. • Board member-The Florida Undergraduate Research Consortium (FURC). A consortium of 24 Florida universities and one of the nation's largest multi- disciplinary research conferences. • Co-chair of the Branding Committee Task Force for proposed St. Thomas University-Barry University merger • Co-author Ethical Branding and Marketing: Cases and Lessons. New York. Rutledge Publishing. Published in Japan, UK & USA • Co-authored Over a Cup of Coffee, a bestselling book about coffee as a consumer product, and the importance of coffee in today’s world. • As President of the American Marketing Association of South Florida, took a non-performing chapter and turned it around. Established fundamental goals and infrastructure and created a vibrant, viable chapter. • Co-founder and faculty advisor- Journal of Student Research (JSR) Education Ph.D. Lynn University, Graduate School of Business, Boca Raton, Florida. Major: Corporate and Organizational Management Doctoral Dissertation: Price and Store Image as Mitigating Factors in the Perception and Evaluation of Retailers’ Customer-Based Brand Equity. Committee Members: Senior Associate Dean, Ralph Norcio (Dissertation Chair), Dean Thomas Kruczek , and Adam Kosnitzky. 1 Post Graduate Certificate, Branding Northwestern University, Kellogg School of Management, Evanston, Illinois Post Graduate Certificate, Case Studies Harvard Graduate School of Business, Cambridge, Massachusetts M.B.A. -

Eddy A. López Solo Exhibitions Selected Group Exhibitions
UPDATED 08/21/2021 EDDY A. LÓPEZ Assistant Professor of Art l Bucknell University l Department of Art + Art History address: 310 Art Building, Bucknell University, Lewisburg, PA 17837 phone: 570.577.1619 l email: [email protected] l web: eddyalopez.com SOLO EXHIBITIONS 2022 TBD, Galeria Codice, Managua, Nicaragua. July, 2022. Postponed from 2020 due to COVID-19. Decrees, Executive Orders, Laws and Other Absurdities, Haas Gallery, Bloomsburg, University, Bloomsburg, PA. 2021 Beautiful War, Marshall University, Huntington, WV. October, 2021, Postponed from 2020 due to COVID-19. 2018 Remixes, Lycoming College Art Gallery, Lycoming College, Williamsport, PA. Beautiful War, Downtown Gallery, Samek Art Museum, Bucknell University, Lewisburg, PA. 2017 Remixes, Vandiver Gallery, South Carolina School of the Arts, Anderson University, Anderson, SC. Composites, Mattie Kelly Arts Center Gallery, Northwest Florida College, Niceville, FL. 2014 Amalgam, University of Miami Gallery at Wynwood, Miami, FL 2000 An Artist’s Quest, Power International Art Gallery, Coral Gables, FL SELECTED GROUP EXHIBITIONS 2021 International Academic Printmaking Alliance 3rd Printmaking Biennale, Central Academy of Fine Arts Art Museum, Beijing, CH. October 2020-October 2021. 41st National Print Exhibition, Artlink Contemporary Gallery, Fort Wayne, IN. Juried by Ruth Lingen. Refuge-Refugee, Northern Illinois University Art Museum, DeKalb, Il. August-November. Re-Emergence! Explorations in Photography and Printmaking, Remarque/New Grounds Print Gallery, Albuquerque, NM. July-August. Cimarron National Works on Paper Exhibition, Gardiner Gallery of Art, Oklahoma State University, Stillwater, OK. Juried by Larissa Goldston. Recollections, Bend Gallery, online exhibition. Curated by Thuong Tran & Maddie May. School of the Art Institute of Chicago, Chicago, IL. -

Project Experience
Project Experience Commercial First Bank of Miami, Kendall Branch Healthcare Historic First Bank of Miami, Coral Gables, FL United Home Care Assisted Living Facilities, Miami, FL Miami News/ Freedom Tower 355 Alhambra Plaza, Coral Gables, FL Florida Atlantic University Health Services, Boca Raton, FL Old Dillard Museum, Miami, FL 255 Aragon Avenue, Coral Gables, FL Camillus Health Concern Clinic, Miami, FL Miami Dade County School Board Ponce de Leon Middle School Westside Plaza I, Miami, FL Broward College Health Sciences Center, Boca Raton, FL Security Building, Miami, FL Westside Plaza II, Miami, FL Miami Bridge Youth Shelter Emergency Care Weiland Clinic, Coral Gables FL General Bank Hialeah Branch Residential Plaza Blue Lagoon Assisted Living Facility, Miami, FL Koubeck House, Miami, FL Republic National Bank, Miami, FL Pan American Community Health Services, Miami, FL Ingraham Building, Miami, FL Miami Dade College Medical Center Campus Charles Deering Estate, Miami, FL Education University of Miami, Batchelor Children’s Research Institute San Carlos Institute, Key West, FL Miami Dade County Public Schools Miami Central Senior High School Florida State University, College of Law, Tallahassee, FL Miami Dade County Public Schools Ponce de Leon Middle School Interiors Granada House, Coral Gables, FL Miami Dade College Aquatic Center Del Monte Fresh Produce Food Lab, Miami, FL Alhambra Circle House, Coral Gables, FL Miami Dade College Inter American Campus John S. and James L. Knight Foundation, Chinese Village House, Coral Gables, FL -

Miami DDA Master Plan
DOWNTOWN MIAMI DWNTWN MIAMI... Epicenter of the Americas 2025 Downtown Miami Master Plan 9 200 ber Octo TABLE OF CONTENTS: INTRODUCTION 05 About the Downtown Development Authority 06 Master Plan Overview 06 Foundation 06 Districts 08 Principles 09 Considerations 09 Acknowledgements 10 How to Use this Document 12 VISION 13 Vision Statement 14 GOALS 15 1. Enhance our Position as the Business and 19 Cultural Epicenter of the Americas 2. Leverage our Beautiful and Iconic Tropical Waterfront 27 3. Elevate our Grand Boulevards to Prominence 37 4. Create Great Streets and Community Spaces 45 5. Promote Transit and Regional Connectivity 53 IMPLEMENTATION 61 Process 62 Matrix 63 CONCLUSION 69 APPENDIX 71 Burle Marx Streetscape Miami DDA DOWNTOWN MIAMI MASTER PLAN 2025 2025 DOWNTOWN MIAMI... EPICENTER OF THE AMERICAS 2 3 INTRODUCTION About the DDA Master Plan Overview Foundation Districts Principles Considerations Acknowledgements How to Use the Document DOWNTOWN MIAMI MASTER PLAN 2025 4 Introduction Introduction ABOUT THE DDA FOUNDATION “Roadmap to Success” Downtown Master Plan Study Miami 21 (Duany Plater-Zyberk): 2009 A Greenprint for Our Future: The Miami-Dade Street CRA Master Plans (Dover Kohl / Zyscovich): (Greater Miami Chamber of Commerce (GMCoC), Tree Master Plan (Miami-Dade County Community 2004 / 2006 Miami 21’s mission is to overhaul the City of Miami’s The Miami Downtown Development Authority (DDA) is The Master Plan stands on a foundation of various New World Center (NWC) Committee): 2009 Image Advisory Board): 2007 a quasi-independent -

Career Advancement Miami Survival Guide: How to Prepare for a Successful Summer in Miami the Resources in This Guide Are for Informational Purposes Only
Career Advancement Miami Survival Guide: How to Prepare for a Successful Summer in Miami The resources in this guide are for informational purposes only. Career Advancement does not endorse or guarantee any of the services described in this document. Students should exercise their own discretion when planning for their summer internship. If you would like more information or have questions about this document, feel free to speak with a Career Advancement adviser. You can make an appointment on UChicago Handshake. 3. Location is everything. It is vital that your housing Welcome to Miami! situation is near your work and/or near transportation that Miami is a city like no other. Known for its beautiful beaches, will get you to work quickly. warm weather, diversity, culture, and distinct arts scene. 4. Decide what is important to you. Once you’ve decided on Miami is an exciting metropolitan city with a Latin Flair. what neighborhoods or borough would be convenient for Downtown Miami is also home to the largest concentration of you, it’s always helpful to explore what attractions they international banks in America, and houses many other large have to offer. Whether you love trying new restaurants, firms and businesses. This city also offers a variety of shopping, or visiting museums and other cultural opportunities for UChicago students who are seeking institutions, try to find a place that will give you the most internships and full-time jobs. time to explore your favorite things. The type of housing you’re looking for, your budget, and your 5. Politely ask your employer about housing resources. -
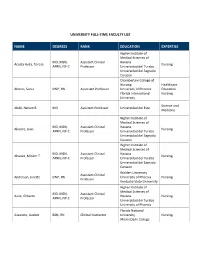
University Full-Time Faculty List
UNIVERSITY FULL-TIME FACULTY LIST NAME DEGREES RANK EDUCATION EXPERTISE Higher Institute of Medical Sciences of MD, MSN, Assistant Clinical Havana Acosta Avila, Teresa Nursing APRN, NP-C Professor Universidad del Turabo Universidad del Sagrado Corazon Chamberlain College of Nursing Healthcare Alonso, Sonia DNP, RN Associate Professor University of Phoenix Education Florida International Nursing University Science and Alubi, Nelson B. MD Assistant Professor Universidad del Este Medicine Higher Institute of Medical Sciences of MD, MSN, Assistant Clinical Havana Alvarez, Juan Nursing APRN, NP-C Professor Universidad del Turabo Universidad del Sagrado Corazon Higher Institute of Medical Sciences of MD, MSN, Assistant Clinical Havana Alvarez, Miriam T. Nursing APRN, NP-C Professor Universidad del Turabo Universidad del Sagrado Corazon Walden University Assistant Clinical Anderson, Julette DNP, RN University of Phoenix Nursing Professor Kentucky State University Higher Institute of Medical Sciences of MD, MSN, Assistant Clinical Avila, Gilberto Havana Nursing APRN, NP-C Professor Universidad del Turabo University of Phoenix Florida National Azzareto, Lizabet BSN, RN Clinical Instructor University Nursing Miami Dade College Higher Institute of Medical Sciences of Villa MD, MSN, Assistant Clinical Clara Bembibre, Ruben Nursing APRN, NP-C Professor Universidad del Turabo Universidad del Sagrado Corazon California Coast Education University Brown, Santarvis PhD(c), MBA Professor Business Columbia Southern Administration University University of -

Business and Economic Research Initiative
Business and Economic Research Initiative EMPLOYMENT REPORT United States, Florida, and Miami Metro Area by: Neela D. Manage College of Business, Florida Atlantic University November 2018 1. November 2018 Employment Report United States, Florida, and Miami Metro Area I. United States and Florida The U.S. unemployment rate in November 2018 was 3.7 percent (seasonally adjusted), unchanged from September and October 2018. Over the year, the unemployment rate declined by 0.4 percentage point from 4.1 percent in November 2017. This month’s unemployment rate is the lowest rate in almost 50 years (was 3.7 percent in October 1969). The labor force participation rate in the U.S. labor market was 62.9 percent. There were 149.89 million employees on nonfarm payrolls in November and the U.S. economyI. UNITED created STATES 155,000 jobs AND since FLORIDA October 2018 and 2,443,000 jobs over the year. Florida’s unemployment rate fell slightly to a seasonally adjusted 3.3 percent in November, a 0.1 Thepercentage U.S. unemployment point decline rate in over November the month 2018 andwas 3.7a 0.6 percent percentage (seasonally point adjusted), decline overunchanged the year. from Florida September was and Octoberone of 2018. six states Over thethat year, had the unemployment unemployment rate rate decredeclinedases by in0.4 November percentage ( alongpoint from with 4.1 Connecticut, percent in November 2017.Maryland, This month’s New unemploymentYork Oklahoma, rate and is the Vermont lowest rate – decline in almost in each50 years 0.1 (was percentage 3.7 percent point). -

2020 Suite Menu Index
> UNIVERSITY OF MIAMI HURRICANES 2020 SUITE MENU INDEX Making It Better To Be There Since 1929.™ 2 WELCOME! Welcome to the 2020 season. INDEX It’s going to be a fantastic year for entertaining at Hard Rock Stadium! We are thrilled to welcome you, delight your guests, and Here’s to the Miami Hurricanes, and to great times at thank you for your support of the University of Miami Hurricanes. Hard Rock Stadium. Welcome and thanks for joining us! Undoubtedly, there will be many special moments throughout the year, and we are dedicated to ensuring Centerplate’s Cheers! hospitality services add to your unforgettable memories of this Hurricanes season enjoyed together with family, friends, and colleagues. Ryan Cellucci From traditional fan-favorite foods, to on-trend locally sourced Ryan Cellucci, Suites Manager regional specialties, everything we prepare is meant to create Centerplate Catering at Hard Rock Stadium and enrich the time you spend together with your guests. We believe in the power of hospitality to help people connect in meaningful ways, and our mission is simple: Making It Better to Be There®. In keeping with our commitment to your satisfaction, we are honored to host your event and we welcome special requests. Please let me know how we may help create special dishes that O 305.623.6425 are perfect for your celebration. My contact information is listed [email protected] here for your convenience. Please call! 3 INDEX PAGE Service Directory 5 From the Grill 16 EZPlanit Ordering Instructions 6 Sandwiches 17 INDEX Commitment to Quality & Safety 7 Hand-Carved Action Cart 18 Personalized Hospitality Package 9 Very Vegan 19 Make it Local 10 Bake It Local 20 Guacamole & Taco Cart 11 Sweet Selections 21 Snacks 12 Beverages 23 Appetizers 13 Order Timing 24 Salad-Sides-Fruit-Veggies 14 Fine Print 25-26 Hard Rock Stadium Flatbreads 15 Click on any of the INDEX items to jump immediately to that page.