Dementia Prevention in Japan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Repeated Story of the Tragedy of the Commons a Short Survey on the Pacific Bluefin Tuna Fisheries and Farming in Japan
A Repeated Story of the Tragedy of the Commons A Short Survey on the Pacific Bluefin Tuna Fisheries and Farming in Japan YASUHIRO SANADA A Repeated Story of the Tragedy of the Commons A Short Survey on the Pacific Bluefin Tuna Fisheries and Farming in Japan YASUHIRO SANADA Organization for Regional and Inter-regional Studies, Waseda University Contents Introduction 1 List of Abbreviations 4 PART 1: PBF Fisheries in Japan 7 PART 2: Fish Farming in Japan 53 Conclusion 89 Annexes 91 Acknowledgements This study was funded by the Pew Charitable Trusts based on a research agreement between Waseda University and the Pew Charitable Trust on “Research and Analysis on Fisheries Issues in Japan.” We gratefully acknowledge generous support from the Pew Charitable Trust. Introduction On November 17, 2014, the news that the International Union for the Conservation of Nature (IUCN) added the Pacific Bluefin tuna (PBF) to its Red List of Threatened Species as “Vulnerable,” which meant that it was threatened with extinction, made headlines and received substantial TV coverage around Japan. After citing the IUCN’s comment that the species was extensively targeted by the fishing industry for the predominant sushi and sashimi markets in Asia, Mainichi Shimbun, one of the major newspapers in Japan, reported that the population was estimated to have declined by 19 to 33% over the past 22 years1. Nihon Keizai Shimbun, a leading Japanese economic newspaper, referring to the fact that the American eel was also added to the List as “Endangered,” pointed out that -

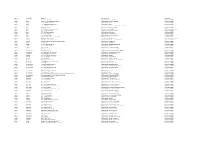
Membership Register MBR0009
LIONS CLUBS INTERNATIONAL CLUB MEMBERSHIP REGISTER SUMMARY THE CLUBS AND MEMBERSHIP FIGURES REFLECT CHANGES AS OF JUNE 2020 CLUB CLUB LAST MMR FCL YR MEMBERSHI P CHANGES TOTAL DIST IDENT NBR CLUB NAME COUNTRY STATUS RPT DATE OB NEW RENST TRANS DROPS NETCG MEMBERS 5160 024661 AMA JAPAN 334 A 4 06-2020 54 1 0 0 -2 -1 53 5160 024662 ANJYO MINAMI JAPAN 334 A 4 06-2020 74 0 0 0 -6 -6 68 5160 024663 ANJYO JAPAN 334 A 4 06-2020 45 3 0 1 -6 -2 43 5160 024669 CHIRYU JAPAN 334 A 4 06-2020 67 4 0 0 -3 1 68 5160 024670 CHITA JAPAN 334 A 4 06-2020 42 4 0 0 -6 -2 40 5160 024675 GAMAGORI JAPAN 334 A 4 06-2020 56 5 0 1 -4 2 58 5160 024680 HANDA JAPAN 334 A 4 06-2020 76 8 0 0 -7 1 77 5160 024681 HEKINAN JAPAN 334 A 4 06-2020 87 6 0 0 -4 2 89 5160 024685 ICHINOMIYA JAPAN 334 A 4 06-2020 199 11 0 0 -10 1 200 5160 024688 INAZAWA JAPAN 334 A 4 06-2020 51 0 0 0 -12 -12 39 5160 024689 ICHINOMIYA NAKA JAPAN 334 A 4 06-2020 40 1 0 0 -4 -3 37 5160 024690 INUYAMA JAPAN 334 A 4 06-2020 65 0 0 0 -2 -2 63 5160 024691 ICHINOMIYA SOUTH JAPAN 334 A 4 06-2020 56 9 0 0 -8 1 57 5160 024696 KARIYA KINUURA JAPAN 334 A 4 06-2020 21 2 1 0 -3 0 21 5160 024698 KANIE JAPAN 334 A 4 06-2020 40 2 0 0 -2 0 40 5160 024700 KARIYA JAPAN 334 A 4 06-2020 65 1 0 1 -3 -1 64 5160 024701 KASUGAI JAPAN 334 A 4 06-2020 84 2 0 0 -18 -16 68 5160 024703 KIRA JAPAN 334 A 4 06-2020 47 2 0 0 -2 0 47 5160 024707 KOMAKI JAPAN 334 A 4 06-2020 73 2 0 0 -10 -8 65 5160 024709 KONAN JAPAN 334 A 4 06-2020 187 3 2 0 -66 -61 126 5160 024710 KOTA JAPAN 334 A 4 06-2020 19 0 0 0 -11 -11 8 5160 024717 MIHAMA JAPAN -

Use of Mobility Scooters on Trains 168.1KB
To passengers using mobility scooters: Make sure to read this before using JR Central lines Accessible trains and mobility scooters you can use Your mobility scooter’s size should not exceed 70cm in width and 120cm in length and height. (These are the same dimensions required for manual and other types of wheelchairs.) Mobility scooter users can board conventional line carriages that are both vestibule-free and step-free. *Limited express train carriages and some rapid or local train carriages that have vestibules or steps cannot accommodate mobility scooters. Meanwhile, you can board some carriages that are equipped with small steps. For details, inquire JR Central’s telephone information center (service is provided in Japanese)*1. The space that mobility scooter users can access on the Tokaido-Sanyo Shinkansen is limited to the multi-purpose room of Series N700 carriages. In addition to being within the dimensions mentioned above, mobility scooters that can be accommodated are only those with both of the following capabilities: (a) Capable of maneuvering right angles (i.e. Mobility scooters that meet both conditions (1) and (2)) (1) Can turn a 0.9m-wide, right angle within five adjustments (2) Can turn a 1.0m-wide, right angle without making any adjustments (b) Capable of turning 180 degrees Can turn 180 degrees within a space that’s less than 1.8m wide Your mobility scooter has these capabilities if the vehicle’s body is labeled with a sticker indicating turning capabilities (“Turning Capability ○○○”), a sticker indicating a star count (“Turning Capability ★★★”), or an “Advanced Mobility Scooter Sticker” issued by the Japan Assistive Products Evaluation Center or other institutions. -
Area Locality Address Description Operator Aichi Aisai 10-1
Area Locality Address Description Operator Aichi Aisai 10-1,Kitaishikicho McDonald's Saya Ustore MobilepointBB Aichi Aisai 2283-60,Syobatachobensaiten McDonald's Syobata PIAGO MobilepointBB Aichi Ama 2-158,Nishiki,Kaniecho McDonald's Kanie MobilepointBB Aichi Ama 26-1,Nagamaki,Oharucho McDonald's Oharu MobilepointBB Aichi Anjo 1-18-2 Mikawaanjocho Tokaido Shinkansen Mikawa-Anjo Station NTT Communications Aichi Anjo 16-5 Fukamachi McDonald's FukamaPIAGO MobilepointBB Aichi Anjo 2-1-6 Mikawaanjohommachi Mikawa Anjo City Hotel NTT Communications Aichi Anjo 3-1-8 Sumiyoshicho McDonald's Anjiyoitoyokado MobilepointBB Aichi Anjo 3-5-22 Sumiyoshicho McDonald's Anjoandei MobilepointBB Aichi Anjo 36-2 Sakuraicho McDonald's Anjosakurai MobilepointBB Aichi Anjo 6-8 Hamatomicho McDonald's Anjokoronaworld MobilepointBB Aichi Anjo Yokoyamachiyohama Tekami62 McDonald's Anjo MobilepointBB Aichi Chiryu 128 Naka Nakamachi Chiryu Saintpia Hotel NTT Communications Aichi Chiryu 18-1,Nagashinochooyama McDonald's Chiryu Gyararie APITA MobilepointBB Aichi Chiryu Kamishigehara Higashi Hatsuchiyo 33-1 McDonald's 155Chiryu MobilepointBB Aichi Chita 1-1 Ichoden McDonald's Higashiura MobilepointBB Aichi Chita 1-1711 Shimizugaoka McDonald's Chitashimizugaoka MobilepointBB Aichi Chita 1-3 Aguiazaekimae McDonald's Agui MobilepointBB Aichi Chita 24-1 Tasaki McDonald's Taketoyo PIAGO MobilepointBB Aichi Chita 67?8,Ogawa,Higashiuracho McDonald's Higashiura JUSCO MobilepointBB Aichi Gamagoori 1-3,Kashimacho McDonald's Gamagoori CAINZ HOME MobilepointBB Aichi Gamagori 1-1,Yuihama,Takenoyacho -

Summary of Family Membership and Gender by Club MBR0018 As of June, 2009
Summary of Family Membership and Gender by Club MBR0018 as of June, 2009 Club Fam. Unit Fam. Unit Club Ttl. Club Ttl. District Number Club Name HH's 1/2 Dues Females Male TOTAL District 334 A 24659 AGUI 0 0 1 43 44 District 334 A 24661 AMA 0 0 0 34 34 District 334 A 24662 ANJYO MINAMI 0 0 10 88 98 District 334 A 24663 ANJYO 0 0 0 76 76 District 334 A 24667 BISAI 0 0 0 29 29 District 334 A 24669 CHIRYU 0 0 0 81 81 District 334 A 24670 CHITA 0 0 1 35 36 District 334 A 24675 GAMAGORI 0 0 1 41 42 District 334 A 24680 HANDA 0 0 3 91 94 District 334 A 24681 HEKINAN 0 0 0 82 82 District 334 A 24685 ICHINOMIYA 0 0 3 76 79 District 334 A 24688 INAZAWA 2 2 0 58 58 District 334 A 24689 ICHINOMIYA NAKA 0 0 0 27 27 District 334 A 24690 INUYAMA 0 0 1 60 61 District 334 A 24691 ICHINOMIYA SOUTH 0 0 0 54 54 District 334 A 24696 KARIYA KINUURA 0 0 0 31 31 District 334 A 24698 KANIE 0 0 2 28 30 District 334 A 24700 KARIYA 0 0 0 56 56 District 334 A 24701 KASUGAI 0 0 0 64 64 District 334 A 24703 KIRA 0 0 0 45 45 District 334 A 24707 KOMAKI 0 0 6 57 63 District 334 A 24709 KONAN 0 0 0 102 102 District 334 A 24710 KOTA 0 0 1 26 27 District 334 A 24717 MIHAMA 0 0 1 49 50 District 334 A 24718 MINAMICHITA 0 0 1 37 38 District 334 A 24721 MIYOSHI AICHI 0 0 2 29 31 District 334 A 24728 NAGOYA KINJO 4 4 5 14 19 District 334 A 24729 NAGOYA HOST 0 0 3 40 43 District 334 A 24730 NAGOYA ATSUTA 0 0 0 25 25 District 334 A 24731 NAGOYA AOI 0 0 1 33 34 District 334 A 24732 NAGOYA EAST 0 0 1 35 36 District 334 A 24733 NAGOYA KITA 0 0 0 36 36 District 334 A 24734 NAGOYA -

Development of Healthy Communities in the “With Corona” Era
Development of Healthy Communities in the “With Corona” Era Katsunori Kondo Center for Preventive Medical Sciences, Chiba University National Center for Geriatrics and Gerontology Japan Gerontological Evaluation Study (JAGES) Japan Gerontological Evaluation Study JAGES Survey of Health and Living Participating ■ Participating municipalities in 2019 survey JAGES 2019 Municipalities ■ Participating municipalities in the previous surveys 64 municipalities Tomakomae Higashikawa Town Town, Nagoya City, Handa City, Higashikagura Hekinan City, Tokoname City, Town, Biei Town Tokai City, Obu City, Chita City, Tobetsu Number of questionnaires sent: Higashiura Town, Taketoyo Town Town 375,421 Yoichi Number of responses: 258,842 Town Response rate: 68.9% Kuriyama JAGES 2016/17 Town Towada Number of municipalities: 40 City Rokunohe Gonohe Town Number of questionnaires sent: Town Hachinohe Approx. 300 thousand Kosaka Town Town Aichi Nanbu Number of responses: Approx. Town Prefecture Niigata Sannohe 200 thousand City Town Tokamachi Response rate: Approx. 69.5% City Hayakawa Iwanuma Town City Chuo JAGES 2013/14 Matsumoto City Katsurao Toyonaka City Village Number of municipalities: 30 City Kaga Oarai Taka City Town Number of questionnaires sent: Town Saitama Takahama City Approx. 200 thousand Tottori Town City Kashiwa Number of responses: Approx. Chizu City Town Nagara Fukuoka Matsudo Town 140 thousand City City Response rate: Approx. 70.8% Ichikawa City Mutsuzawa Town Tenri Oyama Machida Yokohama City Town City City JAGES 2010/11 Ichihara Kobe Ikoma Morimachi Hachioji City City Number of municipalities: 31 City Town City Tsukumi Yao Number of questionnaires sent: Matsuura City City City Usuki Approx. 170 thousand City Moriguchi City, Kadoma City, Number of responses: Approx. Mifune Taketa Shijonawate City Town Kokonoe City 110 thousand Town Response rate: Approx. -

Impact of Increased Long-Term Care Insurance Payments on Employment and Wages in Formal Long-Term Care
DISCUSSION PAPER SERIES IZA DP No. 12383 Impact of Increased Long-Term Care Insurance Payments on Employment and Wages in Formal Long-Term Care Ayako Kondo MAY 2019 DISCUSSION PAPER SERIES IZA DP No. 12383 Impact of Increased Long-Term Care Insurance Payments on Employment and Wages in Formal Long-Term Care Ayako Kondo University of Tokyo and IZA MAY 2019 Any opinions expressed in this paper are those of the author(s) and not those of IZA. Research published in this series may include views on policy, but IZA takes no institutional policy positions. The IZA research network is committed to the IZA Guiding Principles of Research Integrity. The IZA Institute of Labor Economics is an independent economic research institute that conducts research in labor economics and offers evidence-based policy advice on labor market issues. Supported by the Deutsche Post Foundation, IZA runs the world’s largest network of economists, whose research aims to provide answers to the global labor market challenges of our time. Our key objective is to build bridges between academic research, policymakers and society. IZA Discussion Papers often represent preliminary work and are circulated to encourage discussion. Citation of such a paper should account for its provisional character. A revised version may be available directly from the author. ISSN: 2365-9793 IZA – Institute of Labor Economics Schaumburg-Lippe-Straße 5–9 Phone: +49-228-3894-0 53113 Bonn, Germany Email: [email protected] www.iza.org IZA DP No. 12383 MAY 2019 ABSTRACT Impact of Increased Long-Term Care Insurance Payments on Employment and Wages in Formal Long-Term Care* This paper examines the effect of raising Long-term Care Insurance (LTCI) payments on employment and wages of workers in the long-term care (LTC) industry. -

Characteristics of Heavy Rainfall and Flood Damage in Aichi Prefecture from September 11Th to 12Th 2000
Journal of Natural Disaster Science, Volume 24, Number 1, 2002, pp15-24 Characteristics of Heavy Rainfall and Flood Damage in Aichi Prefecture from September 11th to 12th 2000 Haruhiko YAMAMOTO Faculty of Agriculture, Yamaguchi University Kiyoshi IWAYA United Department of Agricultural Science, Graduate School of Tottori University (Received for 4. Apr., 2002) ABSTRACT Record heavy rainfall occurred in Aichi Prefecture from September 11 to 12 2000. We collected about 250 sam- ples of precipitation data observed by various organizations, and analyzed the characteristics of the heavy rainfall that occurred in Aichi Prefecture. The Midori Ward Engineering-Works Office, Nagoya City recorded a daily precipitation of 499.5mm on September 11th and 147.5mm on the 12th. The total precipitation was 647.0mm. In the area from Midori Ward, Nagoya City to Agui Town in Chita district, in the NNE to SSW direction and area 6km wide by 20km long, total precipitation exceeded 600mm. Heavy rainfall of more than 80mm in the area run- ning north and south from Moriyama Ward, Nagoya City to Agui Town appeared at 19:00, and strong rainfall occurred in the surrounding region. Flood damage was severe in 3km north-south and 1km east-west areas bounded by the Shin River, JR Tokaido, Nagoya Railroad Inuyama , and Johoku lines. In the southwest part of Ashihara-cho, Nishi Ward where the bank of the Shin River collapsed and in Nishibiwajima Town, flood depth exceeded 200cm in buildings. Aichi Prefecture is located in the center of Japan and faces the 1. INTRODUCTION Pacific Ocean to the south. The Nobi Plain spreads over the west- The Akisame-front which had been stagnated near Honshu ern part of the prefecture and the Minamialps mountain range over was activated from September 11 to 12, 2000 (Tokyo District the northeast. -
![CSR Report 2008[PDF:3510KB]](https://docslib.b-cdn.net/cover/3340/csr-report-2008-pdf-3510kb-7103340.webp)
CSR Report 2008[PDF:3510KB]
Editori Chubu Electric Power Group CSR Report 2008 This report a sustainab initiatives. Organiza Chubu Elec CSR Electric Pow Report P REPORT Fiscal year 2008) (This repor some impo 2008 occurred o Guideline GRI, Sustai Ministry of Chubu Electric Power Group CSR Report Reporting Date of P September Contactin 1 Higashi-s 461-8680, CSR Group Division Chubu Elec TEL: +81-5 FAX: +81-5 E-mail: Csr Legend In the main explained i location of Look! P00 Related art on the spe report. HP Detailed in n air Electric Pow http://www Web Related we Photogra The photog activities C companies Uchigatani Children sh a beautiful (See the re with regarding f e “waterless” se of harmful Look! www.chuden.co.jp/english/index.html P8,9 Editorial Policy CONTENTS This report describes our efforts to help achieve a sustainable society, and the results of our Chubu Electric Power Group CSR Report 2008 initiatives. Organizations Covered by This Report Chubu Electric Power Co., Inc. and the Chubu R Electric Power Group Companies Editorial Policy Corporate Profile Report Period Chubu Electric Power Group ORT Fiscal year 2007 (April 2007 through March 2008) (This report also includes information regarding CSR in the Chubu Electric Power Group 1 some important events and activities that Message from the President & Director 2 008 occurred outside the above period.) Management Goals 4 Guidelines Used as References CSR Promotion Framework and Activities 6 GRI, Sustainability Reporting Guidelines 2006 Ministry of the Environment, Environmental Highlights of 2007 Reporting -

UNESCO World Conference on Education for Sustainable Development
ESD Catchphrase ESD, creating me From among 770 applications nationwide, this work by Noriko Kawamura (Toyota City) was awarded first prize. This catchphrase expresses the idea that it is I who should create a sustainable society toward the future, and it is EDS that that will create the future nurtures me. Support Plan for Organizing the UNESCO World Conference on Education for Sustainable Development that wil me l cre g at in e t th a e Logo of the host region Design concept e r f c u “ESD Flower That Connects, Grows and , t Blooms” D u This logo design is based on the concept that r ESD serves as a catalyst for connecting educa- S e tion concerning the environment, development, E human rights and various other social challenges with the thought and activities of individual local residents. This concept is expressed with a single line patterned on the “E” of Education. In addition, the four petals, embedded with the letters E, S and D, represent the ESD steps: notice, know, act and expand. http://www.esd-aichi-nagoya.jp Aichi-Nagoya Committee for UNESCO World Conference on ESD R FSC 認証用紙 ユニバーサルデザインフォント この印刷物は、FSC R 認証用 視認性、判読性に優れたユニバーサルデザインフォント 紙を使用しています。 (書体)を使用しています。 Greetings Ⅰ Introduction In November 2014, the UNESCO World Conference on Education for Sustainable Development (ESD) will be held in Nagoya City, Aichi Prefecture. This Conference is of great signicance, in that it will mark the end of the United Nations Decade of Education for Sustainable Development (DESD) (2005 – 2014), which was proposed by Japan. Under the 1. -

はじめに Introduction 前言
はじめに 愛 知 県へようこそ! 愛知生活便利帳は、外国から来日されたみなさんが愛知県で生活を始めるにあたって役に立つ情報を集めたものです。 左ページに日本語、右ページに英語で掲載されています。そのあとに、同じ内容で中国語を掲載しましたので見比べて活用してく ださい。 最後に、この冊子の発行にあたり、情報提供にご協力いただいた各関係機関の方々に改めてお礼申し上げます。 ご 利 用にあたって ○ 掲載された情報は、関係機関 Web サイト、各種リーフレット、関連書籍などを元に当協会が編纂したものです。 ○ できる限り最新の情報を掲載するように努めましたが、発行後、内容が変更される場合もありますのであらかじめご了承ください。 ○ 定訳がない団体名や主な法制度名などは、英語・中国語訳とともに、できる限り日本語のローマ字表記も記載しています。 ○ ここに掲載された内容は一般的なものであり、個別のケースによって取扱いが異なる場合があります。実際に手続きをされる際は 専門機関等でご確認ください。 ○ 掲載団体等の問合せ先に対応言語の記載がないものは日本語のみの対応となります。お問合せの際は日本語のできる人をご同伴 ください。 ○ 掲載団体等の受付時間は変更される場合があります。また、祝祭日および年末年始に休業する場合もありますので事前に各団体 等にご確認ください。 ○ 掲載された内容に関して損害が生じた場合、当協会は一切の責任を負いません。 Introduction Welcome to Aichi Prefecture! Aichi Handbook is a collection of useful information for all of you who just have come to Japan from abroad to start life in Aichi Prefecture. The contents are written in English on the right side page and its Japanese translations are on the left side page. The Chinese ver si on follows next so that you can compare each language version with a Japanese translation. We would like to express our sincere gratitude to those from various organizations for kindly providing information for the publication of this guidebook. For the use of this handbook ○ The published information is collected and edited by the Aichi International Association based on the relevant websites, variou s leaflets, and books. ○ We tried to published the latest information as possible in this book. Please note that information in this handbook is subject change without notice. ○ We listed the names of organizations -

A Guidebook for Your Future and Money
For the foreigners who lives in Aichi Prefecture You'll be glad to know! A Guidebook for your Future and Money えいご 英 語 / E n g li s h Let's learn about your future and money ~ Expenses you will need for your life Table of Contents P3 P4 P5 Giving Birth Education Housing Expense:approx.510,000yen Expense:approx.10,480,000yen Expense:approx:34,420,000yen (one house) All-Japan Federation of National In the case of Kindergarten ~ High School:Public/University:Private Health Insurance Organizations [Birth Jyutaku Kinyu Shien Kikou「 2018nen- Ministry of Education, Culture, Sports, Science and Technology do furatto 35 riyousha chousa 」 Costs 2016] 「Kodomono Gakusyu Chousa 」 (Heisei 30nen-do) [Education Expense Survey for Child](2018) Japanese Housing Finance Agency 「Kokuritsudaigaku nadono jyugyouryou sonotano hiyouni [Year of 2018 Flat35 Usage Survey] kansuru syourei 」 A ministerial ordinance of tuiti ons and the other expenses for National University 「Heisei 29nen-do shiritsu daigaku nyugakusyani kakaru syonendo gakusei noufukin heikingaku(tei-in hitori atari) no Chousani tsuite 」 [Survey Result of Average of First Year Expenses (one person) for Private University Students in 2017 P6 P7 P8 Post-retirement Living support with In the case of death living expenses meals and bathing ・Funeral ・Inheritance Expense: approx.260,000yen Expense :approx.170,000yen per a month per a month Soumukyoku 「Kakei Chousa Nenpou Kousei roudoushou 「Heisei 29nen-do (Kakeisyushihen)Heisei 30nen-dono Kaigo Kyufuhi Jittai Chousa Hyou 5 」 Kakeino Gaiyou Dai 9 hyou 」 Ministry of Health, Labour and Welfare Ministry of Internal Affairs and [2017 Actual Survey on the amount of Communications [Family Income and nursing allowance receive] Expenditure Survey 2018] *Hoken Kyuufugaku, Kouhi futangaku oyobi riyousha futangakuno Goukei (Heisei 30 nen-do shinsabun) P9-10 Inquiry・Consultation desk 1 In a long life, things can be both fun and troublesome And when something happens it cost a lot of money.