Ceftaroline Fosamil for the Treatment of Gram-Positive Endocarditis: CAPTURE Study Experience
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Polymyxin B in Combination with Doripenem Against Heteroresistant Acinetobacter Baumannii: Pharmacodynamics of New Dosing Strategies
J Antimicrob Chemother 2016; 71: 3148–3156 doi:10.1093/jac/dkw293 Advance Access publication 3 August 2016 Polymyxin B in combination with doripenem against heteroresistant Acinetobacter baumannii: pharmacodynamics of new dosing strategies Gauri G. Rao1,2, Neang S. Ly1,2,Ju¨rgen B. Bulitta1,3, Rachel L. Soon1,2, Marie D. San Roman1,2, Patricia N. Holden1,2, Cornelia B. Landersdorfer4, Roger L. Nation4, Jian Li4, Alan Forrest1,5 and Brian T. Tsuji1,2* 1Laboratory for Antimicrobial Pharmacodynamics, School of Pharmacy and Pharmaceutical Sciences, University at Buffalo, The State University of New York, Buffalo, NY, USA; 2The New York State Center of Excellence in Bioinformatics & Life Sciences, University at Buffalo, The State University of New York, Buffalo, NY, USA; 3Center for Pharmacometrics and Systems Pharmacology, College of Pharmacy, University of Florida, Orlando, FL, USA; 4Drug Delivery, Disposition and Dynamics, Monash Institute of Pharmaceutical Sciences, Monash University, Melbourne, Australia; 5Eshelman School of Pharmacy, The University of North Carolina at Chapel Hill, NC, USA *Corresponding author. Tel: +1-716-881-7543; Fax: +1-716-849-6890; E-mail: [email protected] Received 13 October 2015; returned 3 January 2016; revised 14 June 2016; accepted 19 June 2016 Objectives: Polymyxin B is being increasingly utilized as a last resort against resistant Gram-negative bacteria. We examined the pharmacodynamics of novel dosing strategies for polymyxin B combinations to maximize efficacy and minimize the emergence of resistance and drug exposure against Acinetobacter baumannii. Methods: The pharmacodynamics of polymyxin B together with doripenem were evaluated in time–kill experi- ments over 48 h against 108 cfu/mL of two polymyxin-heteroresistant A. -

Medical Review(S) Clinical Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 200327 MEDICAL REVIEW(S) CLINICAL REVIEW Application Type NDA Application Number(s) 200327 Priority or Standard Standard Submit Date(s) December 29, 2009 Received Date(s) December 30, 2009 PDUFA Goal Date October 30, 2010 Division / Office Division of Anti-Infective and Ophthalmology Products Office of Antimicrobial Products Reviewer Name(s) Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD Review Completion October 29, 2010 Date Established Name Ceftaroline fosamil for injection (Proposed) Trade Name Teflaro Therapeutic Class Cephalosporin; ß-lactams Applicant Cerexa, Inc. Forest Laboratories, Inc. Formulation(s) 400 mg/vial and 600 mg/vial Intravenous Dosing Regimen 600 mg every 12 hours by IV infusion Indication(s) Acute Bacterial Skin and Skin Structure Infection (ABSSSI); Community-acquired Bacterial Pneumonia (CABP) Intended Population(s) Adults ≥ 18 years of age Template Version: March 6, 2009 Reference ID: 2857265 Clinical Review Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD NDA 200327: Teflaro (ceftaroline fosamil) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 9 1.1 Recommendation on Regulatory Action ........................................................... 10 1.2 Risk Benefit Assessment.................................................................................. 10 1.3 Recommendations for Postmarketing Risk Evaluation and Mitigation Strategies ........................................................................................................................ -

Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and Its Application
Infect Dis Ther (2017) 6:57–67 DOI 10.1007/s40121-016-0144-8 REVIEW Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and its Application Juwon Yim . Leah M. Molloy . Jason G. Newland Received: November 10, 2016 / Published online: December 30, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT infections, CABP caused by penicillin- and ceftriaxone-resistant S. pneumoniae and Ceftaroline is a novel cephalosporin recently resistant Gram-positive infections that fail approved in children for treatment of acute first-line antimicrobial agents. However, bacterial skin and soft tissue infections and limited data are available on tolerability in community-acquired bacterial pneumonia neonates and infants younger than 2 months (CABP) caused by methicillin-resistant of age, and on pharmacokinetic characteristics Staphylococcus aureus, Streptococcus pneumoniae in children with chronic medical conditions and other susceptible bacteria. With a favorable and those with invasive, complicated tolerability profile and efficacy proven in infections. In this review, the microbiological pediatric patients and excellent in vitro profile of ceftaroline, its mechanism of action, activity against resistant Gram-positive and and pharmacokinetic profile will be presented. Gram-negative bacteria, ceftaroline may serve Additionally, clinical evidence for use in as a therapeutic option for polymicrobial pediatric patients and proposed place in therapy is discussed. Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/ 1F47F0601BB3F2DD. Keywords: Antibiotic resistance; Ceftaroline J. Yim (&) fosamil; Children; Methicillin-resistant St. John Hospital and Medical Center, Detroit, MI, Staphylococcus aureus; Streptococcus pneumoniae USA e-mail: [email protected] L. -

Charm II Antibiotic Analysis—Grain
Charm ii Antibiotic Analysis for Grain Products PROCeDURAL FLOWCHART + Binding Tracer Reagent Tablet Tablet Sample Charm ii 7600 analyzer Incubate START STOP Centrifuge Families DeteCteD = Aminoglycosides = Amphenicols/Chloramphenicol Resuspend = Beta-lactams = Macrolides = Sulfonamides C2Soft = Tetracyclines (optional) Count Results SAMPLE SIZe 50 to 100 g Computer Report SAMPLE PREPARATION Homogenize product in extraction solution for 60 seconds. Filter or centrifuge for 3 minutes. sample printout Test supernatant. Date = 08/23/10 preparation time Approximately 10-15 minutes, Time = 14:28:12 depending on the number of Operator = 1 samples. Time Counted = 60 Sample I.D. = 7764 ASSAY TIME Approximately 10 minutes, depending on drug family. Assay = Chloramphenicol CAPACITY 6 to 12 samples in assay, Lot# = ATBL 014 depending on drug family. Control Point = 2564 Sample (CPM) = 3676 Interpretation = Not Found Charm sciences, inc. 659 Andover Street, Lawrence, MA 01843, USA | Tel: +1.978.687.9200 | www.charm.com Charm ii Antibiotic Analysis for Grain Products Charm ii Kit Drug test sensitivity 1 (ppb) aminoglycosides (STIIHG) Streptomycin 2000 Dihydrostreptomycin 7500 Gentamicin 5000 aminoglycosides (GIIHG) Gentamicin 1000 Neomycin 500 Beta-lactams (PIIG) Penicillin-G 200 Amoxicillin 450 Ampicillin 400 Cephapirin 200 Ceftiofur 500 Cloxacillin 2500 Oxacillin 3750 Dicloxacillin 2500 Cefazolin 1500 Cefodroxil 1500 Cefotaxime 400 Cephalexin 1500 Cephradine 1500 Cefquinome 1000 Hetacillin 400 Nafcillin 3000 Penethamate 200 Piperacillin 1000 Ticarcillin 3500 Chloramphenicol Chloramphenicol 40 Florfenicol 160 & other amphenicols (CIIHG) Thiamphenicol 200 Chloramphenicol (AIIHG) Chloramphenicol 5 macrolides (EIIG) Erythromycin 1000 Tylosin 1000 Spiramycin 1000 Pirlimycin 2000 Tilmicosin 1000 Lincomycin 2500 sulfonamides (SMIIHG) Sulfamethazine 500 Sulfadimethoxine 200 Sulfathiazole 400 Sulfadiazine 200 tetracyclines (TIIHG) Tetracycline 100 Chlortetracycline 800 Oxytetracycline 800 1 Exceed 90% positive at a 95% confidence limit Charm sciences, inc. -

In Vitro Susceptibilities of Escherichia Coli and Klebsiella Spp. To
Jpn. J. Infect. Dis., 60, 227-229, 2007 Short Communication In Vitro Susceptibilities of Escherichia coli and Klebsiella Spp. to Ampicillin-Sulbactam and Amoxicillin-Clavulanic Acid Birgul Kacmaz* and Nedim Sultan1 Department of Central Microbiology and 1Department of Microbiology, Faculty of Medicine, Gazi University, Ankara, Turkey (Received January 30, 2007. Accepted April 13, 2007) SUMMARY: Ampicillin-sulbactam (A/S) and amoxicillin-clavulanic acid (AUG) are thought to be equally efficacious clinically against the Enterobacteriaceae family. In this study, the in vitro activities of the A/S and AUG were evaluated and compared against Escherichia coli and Klebsiella spp. Antimicrobial susceptibility tests were performed by standard agar dilution and disc diffusion techniques according to the Clinical and Laboratory Standards Institute (CLSI). During the study period, 973 strains were isolated. Of the 973 bacteria isolated, 823 were E. coli and 150 Klebsiella spp. More organisms were found to be susceptible to AUG than A/S, regardless of the susceptibility testing methodology. The agar dilution results of the isolates that were found to be sensitive or resistant were also compatible with the disc diffusion results. However, some differences were seen in the agar dilution results of some isolates that were found to be intermediately resistant with disc diffusion. In E. coli isolates, 17 of the 76 AUG intermediately resistant isolates (by disc diffusion), and 17 of the 63 A/S intermediately resistant isolates (by disc diffusion) showed different resistant patterns by agar dilution. When the CLSI breakpoint criteria are applied it should be considered that AUG and A/S sensitivity in E. coli and Klebsiella spp. -

Below Are the CLSI Breakpoints for Selected Bacteria. Please Use Your Clinical Judgement When Assessing Breakpoints
Below are the CLSI breakpoints for selected bacteria. Please use your clinical judgement when assessing breakpoints. The lowest number does NOT equal most potent antimicrobial. Contact Antimicrobial Stewardship for drug selection and dosing questions. Table 1: 2014 MIC Interpretive Standards for Enterobacteriaceae (includes E.coli, Klebsiella, Enterobacter, Citrobacter, Serratia and Proteus spp) Antimicrobial Agent MIC Interpretive Criteria (g/mL) Enterobacteriaceae S I R Ampicillin ≤ 8 16 ≥ 32 Ampicillin-sulbactam ≤ 8/4 16/8 ≥ 32/16 Aztreonam ≤ 4 8 ≥ 16 Cefazolin (blood) ≤ 2 4 ≥ 8 Cefazolin** (uncomplicated UTI only) ≤ 16 ≥ 32 Cefepime* ≤ 2 4-8* ≥ 16 Cefotetan ≤ 16 32 ≥ 64 Ceftaroline ≤ 0.5 1 ≥ 2 Ceftazidime ≤ 4 8 ≥ 16 Ceftriaxone ≤ 1 2 ≥ 4 Cefpodoxime ≤ 2 4 ≥ 8 Ciprofloxacin ≤ 1 2 ≥ 4 Ertapenem ≤ 0.5 1 ≥ 2 Fosfomycin ≤ 64 128 ≥256 Gentamicin ≤ 4 8 ≥ 16 Imipenem ≤ 1 2 ≥ 4 Levofloxacin ≤ 2 4 ≥ 8 Meropenem ≤ 1 2 ≥ 4 Piperacillin-tazobactam ≤ 16/4 32/4 – 64/4 ≥ 128/4 Trimethoprim-sulfamethoxazole ≤ 2/38 --- ≥ 4/76 *Susceptibile dose-dependent – see chart below **Cefazolin can predict results for cefaclor, cefdinir, cefpodoxime, cefprozil, cefuroxime axetil, cephalexin and loracarbef for uncomplicated UTIs due to E.coli, K.pneumoniae, and P.mirabilis. Cefpodoxime, cefinidir, and cefuroxime axetil may be tested individually because some isolated may be susceptible to these agents while testing resistant to cefazolin. Cefepime dosing for Enterobacteriaceae ( E.coli, Klebsiella, Enterobacter, Citrobacter, Serratia & Proteus spp) Susceptible Susceptible –dose-dependent (SDD) Resistant MIC </= 2 4 8 >/= 16 Based on dose of: 1g q12h 1g every 8h or 2g every 8 h Do not give 2g q12 Total dose 2g 3-4g 6g NA Table 2: 2014 MIC Interpretive Standards for Pseudomonas aeruginosa and Acinetobacter spp. -

Summary of Product Characteristics
SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Augmentin 125 mg/31.25 mg/5 ml powder for oral suspension Augmentin 250 mg/62.5 mg/5 ml powder for oral suspension 2. QUALITATIVE AND QUANTITATIVE COMPOSITION When reconstituted, every ml of oral suspension contains amoxicillin trihydrate equivalent to 25 mg amoxicillin and potassium clavulanate equivalent to 6.25 mg of clavulanic acid. Excipients with known effect Every ml of oral suspension contains 2.5 mg aspartame (E951). The flavouring in Augmentin contains maltodextrin (glucose) (see section 4.4). This medicine contains less than 1 mmol sodium (23 mg) per ml, that is to say essentially ‘sodium- free’. When reconstituted, every ml of oral suspension contains amoxicillin trihydrate equivalent to 50 mg amoxicillin and potassium clavulanate equivalent to 12.5 mg of clavulanic acid. Excipients with known effect Every ml of oral suspension contains 2.5 mg aspartame (E951). The flavouring in Augmentin contains maltodextrin (glucose) (see section 4.4). This medicine contains less than 1 mmol sodium (23 mg) per ml, that is to say essentially ‘sodium- free’. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder for oral suspension. Off-white powder. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Augmentin is indicated for the treatment of the following infections in adults and children (see sections 4.2, 4.4 and 5.1): • Acute bacterial sinusitis (adequately diagnosed) • Acute otitis media • Acute exacerbations of chronic bronchitis (adequately diagnosed) • Community acquired pneumonia • Cystitis • Pyelonephritis 2 • Skin and soft tissue infections in particular cellulitis, animal bites, severe dental abscess with spreading cellulitis • Bone and joint infections, in particular osteomyelitis. -

Ampicillin (Ampicillin Sodium) INJECTION, POWDER, FOR
Ampicillin for Injection, USP Rx Only (For Intramuscular or Intravenous Injection) To reduce the development of drug-resistant bacteria and maintain the effectiveness of ampicillin and other antibacterial drugs, ampicillin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ampicillin for injection, USP the monosodium salt of [2S-[2α,5α,6β(S*)]]-6- [(aminophenylacetyl)amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid, is a synthetic penicillin. It is an antibacterial agent with a broad spectrum of bactericidal activity against both penicillin-susceptible Gram-positive organisms and many common Gram-negative pathogens. Ampicillin for injection, USP is a white to cream-tinged, crystalline powder. The reconstituted solution is clear, colorless and free from visible particulates. Each vial of Ampicillin for injection, USP contains ampicillin sodium equivalent to 250 mg, 500 mg, 1 gram or 2 grams ampicillin. Ampicillin for injection, USP contains 65.8 mg [2.9 mEq] sodium per gram ampicillin. It has the following molecular structure: The molecular formula is C16H18N3NaO4S, and the molecular weight is 371.39. The pH range of the reconstituted solution is 8 to 10. CLINICAL PHARMACOLOGY Ampicillin for injection diffuses readily into most body tissues and fluids. However, penetration into the cerebrospinal fluid and brain occurs only when the meninges are inflamed. Ampicillin is excreted largely unchanged in the urine and its excretion can be delayed by concurrent administration of probenecid. Due to maturational changes in renal function, ampicillin half-life decreases as postmenstrual age (a sum of gestational age and postnatal age) increases for infants with postnatal age of less than 28 days. -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -
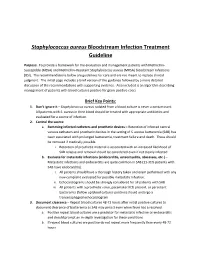
Staphylococcus Aureus Bloodstream Infection Treatment Guideline
Staphylococcus aureus Bloodstream Infection Treatment Guideline Purpose: To provide a framework for the evaluation and management patients with Methicillin- Susceptible (MSSA) and Methicillin-Resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI). The recommendations below are guidelines for care and are not meant to replace clinical judgment. The initial page includes a brief version of the guidance followed by a more detailed discussion of the recommendations with supporting evidence. Also included is an algorithm describing management of patients with blood cultures positive for gram-positive cocci. Brief Key Points: 1. Don’t ignore it – Staphylococcus aureus isolated from a blood culture is never a contaminant. All patients with S. aureus in their blood should be treated with appropriate antibiotics and evaluated for a source of infection. 2. Control the source a. Removing infected catheters and prosthetic devices – Retention of infected central venous catheters and prosthetic devices in the setting of S. aureus bacteremia (SAB) has been associated with prolonged bacteremia, treatment failure and death. These should be removed if medically possible. i. Retention of prosthetic material is associated with an increased likelihood of SAB relapse and removal should be considered even if not clearly infected b. Evaluate for metastatic infections (endocarditis, osteomyelitis, abscesses, etc.) – Metastatic infections and endocarditis are quite common in SAB (11-31% patients with SAB have endocarditis). i. All patients should have a thorough history taken and exam performed with any new complaint evaluated for possible metastatic infection. ii. Echocardiograms should be strongly considered for all patients with SAB iii. All patients with a prosthetic valve, pacemaker/ICD present, or persistent bacteremia (follow up blood cultures positive) should undergo a transesophageal echocardiogram 3. -

Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F
Philadelphia College of Osteopathic Medicine DigitalCommons@PCOM PCOM Scholarly Papers 2014 Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F. DeBellis Kimberly L. Barefield Philadelphia College of Osteopathic Medicine, [email protected] Follow this and additional works at: https://digitalcommons.pcom.edu/scholarly_papers Part of the Medicine and Health Sciences Commons Recommended Citation DeBellis, Heather F. and Barefield, Kimberly L., "Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia" (2014). PCOM Scholarly Papers. 1913. https://digitalcommons.pcom.edu/scholarly_papers/1913 This Article is brought to you for free and open access by DigitalCommons@PCOM. It has been accepted for inclusion in PCOM Scholarly Papers by an authorized administrator of DigitalCommons@PCOM. For more information, please contact [email protected]. Open Access: Full open access to Clinical Medicine Reviews this and thousands of other papers at http://www.la-press.com. in Therapeutics Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia Heather F. DeBellis and Kimberly L. Tackett South University School of Pharmacy, Savannah, GA, USA. ABSTR ACT: Ceftaroline fosamil is a new fifth-generation cephalosporin indicated for the treatment of community-acquired bacterial pneumonia (CABP). It possesses antimicrobial effects against both Gram-positive and Gram-negative bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), but not against anaerobes. Organisms covered by this novel agent that are commonly associated with CABP are Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, and Klebsiella pneumoniae; however, ceftaroline fosamil lacks antimicrobial activity against Pseudomonas and Acinetobacter species. -

Ceftaroline in Complicated Skin and Skin-Structure Infections
Infection and Drug Resistance Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Ceftaroline in complicated skin and skin-structure infections Paul O Hernandez1 Abstract: Ceftaroline is an advanced-generation cephalosporin antibiotic recently approved by Sergio Lema2 the US Food and Drug Administration for the treatment of complicated skin and skin-structure Stephen K Tyring3 infections (cSSSIs). This intravenous broad-spectrum antibiotic exerts potent bactericidal activity Natalia Mendoza2,4 by inhibiting bacterial cell wall synthesis. A high affinity for the penicillin-binding protein 2a (PBP2a) of methicillin-resistant Staphylococcus aureus (MRSA) makes the drug especially 1University of Texas School of Medicine at San Antonio, beneficial to patients with MRSA cSSSIs. Ceftaroline has proved in multiple well-conducted San Antonio, TX, 2Woodhull clinical trials to have an excellent safety and efficacy profile. In adjusted doses it is also recom- Medical and Mental Health Center, mended for patients with renal or hepatic impairment. Furthermore, the clinical effectiveness Brooklyn, NY, 3Department of Dermatology, University of Texas and high cure rate demonstrated by ceftaroline in cSSSIs, including those caused by MRSA Health Science Center at Houston, and other multidrug-resistant strains, warrants its consideration as a first-line treatment option 4 Houston, TX, USA; Department of for cSSSIs. This article reviews ceftaroline and its pharmacology, efficacy, and safety data to Dermatology, El