Irish Clinical Research Infrastructure Network (ICRIN) Assessment of The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
FID in FOCUS Bret Schaefer
FID IN FOCUS Fall Newsletter 2020 A message from incoming Board Chair Bret Schaefer I am honored to be the incoming Board Chair of FID, following Richard Cheung, who has been an incredible leader of this organization for the past several years. I have been serving as Treasurer, and so have seen the tremendous growth that Friends In Deed has experienced, both financially and programmatically. We are serving so many more people in need, but providing our critical services with the same hallmark compassion, connection, and dignity. Of course, during these extremely difficult times of COVID, there have been unprecedented challenges. I am proud of our staff, volunteers and board of directors for stepping up and meeting these challenges head on, adapting our programs to meet the needs of our community, and doing it so successfully. The foundation for the long-term success of FID is the dedicated support we receive from the community both in terms of volunteers and financial support. We are especially gratified by the increased level of donations we have received in response to the economic hardship our most vulnerable neighbors have experienced this year. I am hopeful that our current challenges will inspire the community to support redoubled efforts to serve the homeless and disadvantaged in Pasadena. So, thanks to all you for being part of our team! I look forward to serving FID in the coming year and with your help we will continue to do together what we cannot do alone. Stories from the programs Timely support Creating communities during COVID - Kenneth's Story Kenneth’s mother died a year before his release from jail, which meant that he re- entered society with almost no support network. -

Irish Babies Names 2003.Vp
19 May 2004 Irish Babies’ Names Sean and Emma 1998-2003 2003 1000 Sean Five most popular babies’ names 900 Emma Boys Girls 800 700 Name Count Name Count Sean 897 Emma 791 600 Jack 800 Sarah 606 500 Adam 787 Aoife 571 400 Conor 705 Ciara 535 300 James 626 Katie 468 200 100 Sean and Emma 0 1998 1999 2000 2001 2002 2003 Sean and Emma were the most popular babies’ names registered last year. There were 897 boys named Sean (3.1% of baby boys) and 791 girls named Emma (2.8% of baby girls). See Tables 1 and 2. The top five names for boys remained the same as last year, although the order changed slightly. For girls, Katie replaced Chloe in the top five. See Table 1. There were eight new entries to the top 100 for boys: Cameron, Colin, Daire, Emmanuel, Karl, Max, Reece and Ruairi. The highest new entry was Colin and the highest climber was Kian which rose from 268th place in 1998 to 65th place in 2003. First time entries to the top 100 are Ruairi, Emmanuel and Max. See Table 1. Published by the Central Statistics Office, Ireland. There were nine new names in the top 100 for girls: Alana, Amber, Aoibhe, Ardee Road Skehard Road Dublin 6 Cork Cara, Clara, Faye, Naomi, Sophia and Sorcha. The highest new entry was Clara Ireland Ireland and the highest climber was Abby which rose from 327th place in 1998 to 60th place in 2003. Newcomers to the top 100 are Faye, Naomi, Aoibhe and Sophia. -

Siobhan Greene
April 18, 2019 www.montereyrotary.org LLaa RRuueeddaa THE ROTARY CLUB OF MONTEREY, RI DISTRICT 5230 SERVICE ABOVE SELF TODAY’S PROGRAM and fundraising. Dedicated Director of Activity April 18, 2019 to the movement to Therapy for Alta Bates- Siobhan Greene improve quality at end of Herrick Hospital in Berkeley President and CEO Hospice life, Siobhan serves on the prior to moving the Giving Foundation Reimagine Advisory, is Monterey Peninsula. active with a collective of Siobhan was President of serious illness funders the Rotary Club of examining the system of care Carmel-by-the-Sea (2016) and participates with local and is past-commissioner professional collaboratives for Monterey County’s addressing local needs.Her Juvenile Justice Commission past professional experience having been chair in 2012. includes working with children, Siobhan served on California CASA Board mental health services, and of Directors focusing on at-risk community groups. statewide system improve- Before joining HG Founda- ment for children in foster tion, Siobhan was Executive care; is past-chair of and Siobhan Greene began Director of Voices for continues to be active serving as President/CEO Children – CASA of Monterey with the Monterey Bay for Hospice Giving County for 11 years and Association of Fundraising Foundation in August 2013. currently serves on CASA’s Professionals; and has She specializes in nonprofit Board. Siobhan began her served on AFP’s National executive and financial career working in in-patient Philanthropy Day local management, board psychiatric -
Given Name Alternatives for Irish Research
Given Name Alternatives for Irish Research Name Abreviations Nicknames Synonyms Irish Latin Abigail Abig Ab, Abbie, Abby, Aby, Bina, Debbie, Gail, Abina, Deborah, Gobinet, Dora Abaigeal, Abaigh, Abigeal, Gobnata Gubbie, Gubby, Libby, Nabby, Webbie Gobnait Abraham Ab, Abm, Abr, Abe, Abby, Bram Abram Abraham Abrahame Abra, Abrm Adam Ad, Ade, Edie Adhamh Adamus Agnes Agn Aggie, Aggy, Ann, Annot, Assie, Inez, Nancy, Annais, Anneyce, Annis, Annys, Aigneis, Mor, Oonagh, Agna, Agneta, Agnetis, Agnus, Una Nanny, Nessa, Nessie, Senga, Taggett, Taggy Nancy, Una, Unity, Uny, Winifred Una Aidan Aedan, Edan, Mogue, Moses Aodh, Aodhan, Mogue Aedannus, Edanus, Maodhog Ailbhe Elli, Elly Ailbhe Aileen Allie, Eily, Ellie, Helen, Lena, Nel, Nellie, Nelly Eileen, Ellen, Eveleen, Evelyn Eibhilin, Eibhlin Helena Albert Alb, Albt A, Ab, Al, Albie, Albin, Alby, Alvy, Bert, Bertie, Bird,Elvis Ailbe, Ailbhe, Beirichtir Ailbertus, Alberti, Albertus Burt, Elbert Alberta Abertina, Albertine, Allie, Aubrey, Bert, Roberta Alberta Berta, Bertha, Bertie Alexander Aler, Alexr, Al, Ala, Alec, Ales, Alex, Alick, Allister, Andi, Alaster, Alistair, Sander Alasdair, Alastar, Alsander, Alexander Alr, Alx, Alxr Ec, Eleck, Ellick, Lex, Sandy, Xandra, Zander Alusdar, Alusdrann, Saunder Alfred Alf, Alfd Al, Alf, Alfie, Fred, Freddie, Freddy Albert, Alured, Alvery, Avery Ailfrid Alberedus, Alfredus, Aluredus Alice Alc Ailse, Aisley, Alcy, Alica, Alley, Allie, Allison, Alicia, Alyssa, Eileen, Ellen Ailis, Ailise, Aislinn, Alis, Alechea, Alecia, Alesia, Aleysia, Alicia, Alitia Ally, -

Baby Girl Names | Registered in 2019
Vital Statistics Baby2019 BabyGirl GirlsNames Names | Registered in 2019 From:Jan 01, 2019 To: Dec 31, 2019 First Name Frequency First Name Frequency First Name Frequency Aadhini 1 Aarnavi 1 Aadhirai 1 Aaro 1 Aadhya 2 Aarohi 2 Aadila 1 Aarora 1 Aadison 1 Aarushi 1 Aadroop 1 Aarya 3 Aadya 3 Aarza 2 Aafiya 1 Aashvee 1 Aaghnya 1 Aasiya 1 Aahana 2 Aasiyah 2 Aaila 1 Aasmi 1 Aaira 3 Aasmine 1 Aaleena 1 Aatmja 1 Aalia 1 Aatri 1 Aaliah 1 Aayah 2 Aalis 1 Aayara 1 Aaliya 1 Aayat 1 Aaliyah 17 Aayla 1 Aaliyah-Lynn 1 Aayna 1 Aalya 1 Aayra 2 Aamina 1 Aazeen 1 Aamna 1 Abagail 1 Aanaya 1 Abbey 4 Aaniya 1 Abbi 1 Aaniyah 1 Abbie 1 Aanya 3 Abbiejean 1 Aara 1 Abbigail 3 Aaradhya 1 Abbiteal 1 Aaradya 1 Abby 10 Aaraya 1 Abbygail 1 Aaria 2 Abdirashid 1 Aariya 1 Abeeha 1 Aariyah 1 Aberlene 1 Aarna 3 Abhideep 1 Abi 1 Abiah 1 10 Jun 2020 1 Abiegail 02:22:21 PM1 Abigael 1 Abigail 141 Abigale 1 1 10 Jun 2020 2 02:22:21 PM Baby Girl Names | Registered in 2019 First Name Frequency First Name Frequency Abigayle 1 Addalyn 4 Abihail 1 Addalynn 1 Abilene 2 Addasyn 1 Abina 1 Addelyn 1 Abisha 2 Addi 1 Ablakat 1 Addie 2 Aboni 1 Addilyn 3 Abrahana 1 Addilynn 2 Abreen 1 Addison 61 Abrielle 2 Addisyn 2 Absalat 1 Addley 1 Abuk 2 Addy 1 Abyan 1 Addyson 2 Abygale 1 Adedoyin 1 Acadia 1 Adeeva 1 Acelynn 1 Adeifeoluwa 1 Achai 1 Adela 1 Achan 1 Adélaïde 1 Achol 1 Adelaide 20 Ackley 1 Adelaine 1 Ada 23 Adelayne 1 Adabpreet 1 Adele 4 Adaeze 1 Adèle 2 Adah 1 Adeleigha 1 Adair 1 Adeleine 1 Adalee 1 Adelheid 1 Adalena 1 Adelia 3 Adaley 1 Adelina 2 Adalina 2 Adeline 40 Adalind 1 Adella -

MISCELLANEOUS LIST INDEX Chester County Court of Common
Chester County Court of Common Pleas PAGE 1 MISCELLANEOUS LIST INDEX From September 27, 2021 through October 01, 2021 Courtroom Event Judge Pages Courtroom 3 Judge Emanuel A. Bertin ....................................... 1 — 8 Courtroom 12 Judge Bret M. Binder ....................................... 9 — 9 Courtroom 6 Judge David F. Bortner ....................................... 10 — 23 Courtroom 5 Judge Jacqueline C. Cody ....................................... 24 — 30 Courtroom 19 Judge Allison Bell Royer ....................................... 31 — 31 Courtroom 8 Judge Jeffrey R. Sommer ....................................... 32 — 33 Courtroom 3 Judge Phyllis Streitel ....................................... 34 — 40 Courtroom 17 Judge Ann Marie Wheatcraft ....................................... 41 — 41 WEDNESDAY, SEPTEMBER 29, 2021 AT 09:30 AM JUDGE EMANUEL A. BERTIN Courtroom 3 9:30 AM Summary Appeals Baker, James E. SA-0000307-2021 / Blackmore, David H. SA-0000306-2021 / Love, Dakota E. SA-0000305-2021 / Menasion, Steven John SA-0000303-2021 / Kelly, Joseph Kevin Milbourne, Brett Omar SA-0000308-2021 / Sheehan, Gary SA-0000302-2021 / 10:30 AM Expungement Hearing Ahn, David CR-0000380-2006 Yen, Ronald C. / Baland, Alexandria Michelle Ahn, David CR-0003103-2006 Yen, Ronald C. / Baland, Alexandria Michelle Ahn, David CR-0003233-2007 Chester County District Attorney's Office / Baland, Alexandria Michelle Ahn, David CR-0003885-2006 Chester County District Attorney's Office / Baland, Alexandria Michelle Page 1 of 41 WEDNESDAY, SEPTEMBER -

Irish Babies' Names 2002
7 May 2003 Irish Babies’ Names 2002 Five most popular babies’ names Boys Girls Name Count Name Count Jack 868 Sarah 655 Sean 866 Aoife 585 Adam 798 Emma 577 Conor 748 Chloe 532 James 581 Ciara 516 Jack and Sarah again Jack and Sarah were the most popular babies’ names registered last year. There were 868 boys named Jack (3.1% of baby boys) and 655 girls named Sarah (2.4% of baby girls). See Tables 1 and 2. The top five names for boys and girls remained the same as last year, although the order changed slightly. See Table 1. There were six new entries to the top 100 for boys: Charlie, Connor, Denis, Eric, Seamus and Steven. Eric and Steven returned to the top 100 after missing out last year. Seamus and Connor also returned to the top 100 after being absent since 1998. See Table 1. Published by the Central Statistics Office, Ireland. There were nine new names in the top 100 for girls: Ailbhe, Eabha, Heather, Isabel, Isabelle, Laoise, Lara, Nadine and Sadhbh. Lara returned to the top 100 Ardee Road Skehard Road Dublin 6 Cork after missing out last year. Heather and Nadine also returned to the top 100 hav- Ireland Ireland ing been absent since 1998. Tel: +353-1 497 7144 Tel: +353-21 453 5000 In general, the tables show that girls are given a wider variety of names than Fax: +353-1 497 2360 Fax: +353-21 453 5555 boys. The top 100 accounted for 62.7% of girls’ names compared with 73.6% of LoCall: 1890 313 414 boys’ names. -
Social Work Strategy Compendium of Resources, Innovations & Improvements
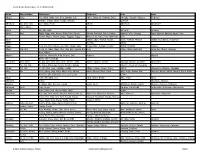
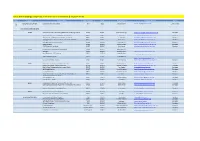
Social Work Strategy Compendium of Resources, Innovations & Improvements Column1 Category Project Title Organisation Year Lead Contact Contact details Status 1 INNOVATION SCHEME Social Work Innovation Scheme DoH 2012 Christine Smyth [email protected] Under revision SWS FUNDED INNOVATIONS NHSCT Quality Improvement of recording assessments in Learning Disability NHSCT 2013/14 Pauline Cummings [email protected] Complete Lean approach to accessing Older People's Services NHSCT 2013/14 Sean Falls [email protected] Complete Aide memoire for NISAT for memory loss assessments NHSCT 2013/14 Karen Harvey [email protected] Complete Quality improvement for assessment and care plans (Physical NHSCT 2013/14 Paula Hanna [email protected] Complete Disability) Trust Wide Contact Support Service NHSCT 2013/14 Doreen Bacon [email protected] Complete Direct Payments NHSCT 2015/16 Sharon McNeill [email protected] Complete CLEAR Dementia Care Model NHSCT 2015/16 Marc Harvey [email protected] Complete SHSCT Implementation of Tele-Visual Smart Boards SHSCT 2013/14 Patrick Robinson Webcams SHSCT 2013/14 Angela Hawkins [email protected] Excel Workbooks - DSF Reporting SHSCT 2013/14 Angela Hawkins [email protected] Video Conferencing CYPS SHSCT 2013/14 Dr Michael Hoy [email protected] Safety in Partnership - Screens SHSCT 2016/17 Niamh Donnelly [email protected] -

Tony Demarco and the Atlantic Wave Includes Tony Demarco, Siobhan Butler, Donie Carroll, Sean Earnest, and Martin O’Connell
Tony DeMarco and the Atlantic Wave includes Tony DeMarco, Siobhan Butler, Donie Carroll, Sean Earnest, and Martin O’Connell Tony DeMarco was born on May 20, 1955, the second of three children raised in East Flatbush by Paul DeMarco and his wife, the former Patricia Dempsey. Paul, a grandson of Italian immigrants, was a teenage lightweight boxing star who turned down an offer to turn pro and work with lightweight champ Paddy “Billygoat” DeMarco in order to pursue a more conventional career on Wall Street. Tony’s maternal grandfather Jimmy Dempsey was a New York City cop and a son of Irish immigrants who married Philomena “Minnie” Fenimore, one of several Italian-American siblings who married into Brooklyn Irish families. Musical ability runs on both sides of Tony’s family. During the Prohibition years, Minnie Dempsey’s Italian immigrant father ran a speakeasy in East New York, where he played the piano and mandolin. Tony’s paternal uncle Louie DeMarco was a singer who performed with 1950s doo-wop groups, including “Dickie Dell and the Ding Dongs.” Tony’s cousin John Pattitucci, from the Fenimore side of the family, is a leading professional bass player who has recorded with jazz stars Chick Corea, Herbie Hancock, and Wayne Shorter. But Tony definitely found his way to Irish traditional music via a different path than the one trod by musicians raised in Irish immigrant households. As he puts it: “I never grew up with the competitive Comhaltas scene—I came through the hippie scene, the folkie scene.” His first exposure to Irish traditional music was through a Folkways recording of the County Sligo fiddler Michael Gorman. -

Ansteorran College of Heralds Does Estrill Swet, Retiarius Pursuivant, Make Greetings
Here are the decisions about ILoI0009 made on December 9, 2000 (AS XXXV) at Stargate Yule Revel, as typed by Kathri (who has corrected the item headers where Bordure needed it, which explains why some of the comments seem to be about problems that don't exist.) Griffon, Bordure (and deputy-Asterisk-for-the-day) Unto the Ansteorran College of Heralds does Estrill Swet, Retiarius Pursuivant, make greetings. For information on commentary submission formats or to receive a copy of the collated commentary, you can contact me at: Deborah Sweet 824 E 8th, Stillwater, OK 74074 405/624-9344 (before 10pm) [email protected] Commenters for this issue: Magnus von Lübeck - Raven's Fort. All items were checked against the on-line O&A. Mari Elspeth nic Bryan - Solveig Throndardottir, Name Construction in Mediaeval Japan, Free Trumpet Studies in Heraldry & Onomastics 87 (Albuquerque, NM: The Outlaw Press, 1994). Andrew W. Nelson, The Compact Nelson Japanese-English Character Dictionary, abridged by John H. Haig. (Rutland, Vermont: Charles E. Tuttle Company, 1999). The documentation for a number of the name submissions in this ILoI is not presented in enough detail to be reviewed by the College of Arms without problems. It is not simply enough to (for example) state that a name is in Withycombe. Even "Withycombe, page (page #)" is not enough. Different editions of Withycombe have the headers on different pages. Even the 3rd edition hardback has entries on different pages than the 3rd edition paperback. Name documentation has to be summarized clearly and completely enough that: 1) a commenter can quickly and easily look up the reference and 2) it is clear why this reference supports the registration of the submitted name In a number of the comments below, I refer to the Annals of Connacht. -

The Social and Ideological Role of Crannogs in Early Medieval Ireland
\ j , a ■SI m w NUI MAYNOOTH OUscoil na hÉireann Ma Nuad THE SOCIAL AND IDEOLOGICAL ROLE OF CRANNOGS IN EARLY MEDIEVAL IRELAND by AID AN O’SULLIVAN THESIS FOR THE DEGREE OF PH.D. DEPARTMENT OF MODERN HISTORY NATIONAL UNIVERSITY OF IRELAND MAYNOOTH HEAD OF DEPARTMENT: Professor R.V. Comerford Supervisor of Research: Mr. John Bradley Volume Two of Two APPENDICES AND BIBLIOGRAPHY March 2004 Contents Appendix 1: A select bibliography of early medieval references to crannogs, islands and lakes............................................. 2 Introduction I. A nnals............................................................................................................................... 2 Annals of Ulster.................................................................................................. 5 Annals of the Four Masters............................................................................... 13 Annals o f Connacht...............................................................................................29 II. Hagiographies............................................................................................................ 35 Life o f Berach.........................................................................................................35 Life of Colman Ela................................................................................................ 36 Life of Colman son of Luachan......................................................... ............ ,.36 Life of Cellach of Killala.................................................................. -

Federal Motor Carrier Safety Administration
FEDERAL MOTOR CARRIER SAFETY ADMINISTRATION Raymond Martinez Administrator Jim Mullen Selika Gore Chief Counsel Senior Advisor Cathy F. Gautreaux Deputy Administrator John Van Steenburg Assistant Administrator & Chief Safety Officer Janettarose Greene Kennie J. May Steven J. LaFreniere Sharon Worthy * Wiley Deck Bruce Edwards Senior Advisor Office Director Regulatory Office Director Office Director Internal Control Program Integration Civil Rights Ombudsman External Affairs Government Affairs Officer Jack Schreibman Dr. G. Kelly Regal Larry W. Minor William A. Quade Anne L. Collins Associate Associate Administrator Associate Leonard Bechtel Associate Administrator Associate Administrator Research & Information Administrator Chief Financial Enforcement Administrator Administration Technology Policy Officer Field Operations Curtis Allen Dr. Steven K, Smith Joseph P. DeLorenzo Deputy Associate Office Director Charles A. Horan II Office Director Administrator Analysis, Research & Office Director Enforcement & Siobhan Crawford Administration Technology Truck & Bus Compliance Deputy CFO Standards Kenneth H. Riddle Thomas P. Keane Office Director Office Director Registration & Robert W. Miller Safety Programs Safety Information Office Director Policy, Strategic Planning & Regulations Colleen Coggins † Chief Information Vacant Officer Chief Medical Curtis L. Thomas Vacant Officer Regional Field Regional Field Administrator Administrator Legend: Darrell L. Ruban Darin Jones Proposed Position Regional Field Regional Field Administrator Administrator