Tension-Type Headache
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -
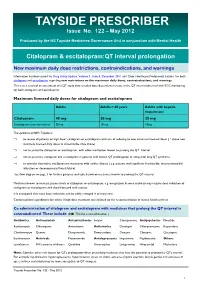
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

(12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed Et Al
US0078.93053B2 (12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed et al. (45) Date of Patent: Feb. 22, 2011 (54) TREATING PSYCHOLOGICAL CONDITIONS WO WO 2006/127418 11, 2006 USING MUSCARINIC RECEPTORM ANTAGONSTS (75) Inventors: Brian Seed, Boston, MA (US); Jordan OTHER PUBLICATIONS Mechanic, Sunnyvale, CA (US) Chau et al. (Nucleus accumbens muscarinic receptors in the control of behavioral depression : Antidepressant-like effects of local M1 (73) Assignee: Theracos, Inc., Sunnyvale, CA (US) antagonist in the porSolt Swim test Neuroscience vol. 104, No. 3, pp. 791-798, 2001).* (*) Notice: Subject to any disclaimer, the term of this Lind et al. (Muscarinic acetylcholine receptor antagonists inhibit patent is extended or adjusted under 35 chick Scleral chondrocytes Investigative Ophthalmology & Visual U.S.C. 154(b) by 726 days. Science, vol.39, 2217-2231.* Chau D., et al., “Nucleus Accumbens Muscarinic Receptors in the (21) Appl. No.: 11/763,145 Control of Behavioral Depression: Antidepressant-like Effects of Local M1 Antagonists in the Porsolt Swin Test.” Neuroscience, vol. (22) Filed: Jun. 14, 2007 104, No. 3, Jun. 14, 2001, pp. 791-798. Bechtel, W.D., et al., “Biochemical pharmacology of pirenzepine. (65) Prior Publication Data Similarities with tricyclic antidepressants in antimuscarinic effects only.” Arzneimittelforschung, vol. 36(5), pp. 793-796 (May 1986). US 2007/O293480 A1 Dec. 20, 2007 Chau, D.T. et al., “Nucleus accumbens muscarinic receptors in the control of behavioral depression: antidepressant-like effects of local Related U.S. Application Data Mantagonist in the Porsolt Swim test.” Neuroscience, vol. 104(3), (60) Provisional application No. -

Impact of Citalopram and Fluvoxamine on Platelet Response To
S24_5 Impact of Citalopram and Fluvoxamine on Platelet Response to Clopidogrel, a Randomized, Double-blind, Crossover Trial Bruria Hirsh Racch1, Galia Spectre2, Ella Shai2, Amit Ritter3, David Varon2, Ronny Alcalai3 1School of Pharmacy, Hadassah Hebrew University Medical Center, Israel 2Coagulation Unit, Hematology, Hadassah Hebrew University Medical Center, Israel 3Heart Institute, Hadassah Hebrew University Medical Center, Israel Background: Selective serotonin reuptake inhibitors (SSRI) are widely used antidepressant agents. Studies have shown that use of SSRI in combination with aspirin or warfarin is associated with an increased risk bleeding, while little information is known about the interaction of SSRIs and clopidogrel. Fluvoxamine and citalopram are both SSRIs and while fluvoxamine is an inhibitor of CYP2C19 and thus might reduce the efficacy of clopidogrel, the effect of citalopram on liver metabolism is unknown. Aim: The aim was to assess the effect these two different SSRIs on platelet aggregation and on the laboratory response to clopidogrel. Methods: A randomized, double-blind, crossover study in 15 healthy volunteers comparing the antiplatelet effect of clopidogrel with and without fluvoxamine or citalopram .The response to clopidogrel was assessed by Light Transmittance Aggregometry with10µmol/L ADP and by vasodilator-stimulated phosphoprotein (VASP) phosphorylation, a measure of P2Y12 receptor reactivity. Results: Mean baseline platelet aggregation was 80.1%±3.4 and reduced to 23.5% after treatment with clopidogrel. Both fluvoxamine and citalopram had modest effect on platelet reactivity (65.8%±6.4, p=0.06 vs. baseline and 67.3%±6.3, p=0.07 vs. baseline respectively). Laboratory response to clopidogrel was significantly better in the presence of citalopram as compared to fluvoxamine both in aggregometry (23.4%±3 vs. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee
Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee Summary of Safety Alert (December 2011) – http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769 Citalopram and escitalopram are associated with dose-dependent QT interval prolongation and should not be used in those with: congenital long QT syndrome; known pre-existing QT interval prolongation; or in combination with other medicines that prolong the QT interval. ECG measurements should be considered for patients with cardiac disease, and electrolyte disturbances should be corrected before starting treatment. For citalopram, new restrictions on the maximum daily doses now apply: 40 mg for adults; 20 mg for patients older than 65 years; and 20 mg for those with hepatic impairment. For escitalopram, the maximum daily dose for patients older than 65 years is now reduced to 10 mg/day; other doses remain unchanged. Recommended actions for prescribers If dose is above maximum recommended dose or patient is taking other medications likely to prolong QTc: Need for more than 1. Discuss with service user/patient. citalopram 40mg daily 2. Consider continued need for citalopram and/or alternative therapies (adults), 20mg daily (elderly and reduced hepatic function) e.g. for OCD, PTSD Adult citalopram Elderly (or other risk factors) Taking ANY other medicines Elderly and escitalopram dose above citalopram dose above likely to cause QTc dose above 10mg daily: prolongation 40mg daily: 20mg daily: Consider risk/benefit with service user. Switch if 1-Consider switching relevant possible medication to alternative with no Monitor If under 18 refer to CAMHS effect on QTc prolongation or Reduce dose stepwise to 40mg citalopram daily for adults (unlicensed use). -

Mid Essex CCG 'Guidance for the Treatment of Depression in Adults'
Guidance for the treatment of depression in adults MILD DEPRESSION - Medication is not first-line treatment or only treatment for depression Actively monitor symptoms, give life style advice, guided self- help or exercise MODERATE DEPRESSION Consider psychological intervention. This is accessed by referral or self-referral to Mid Essex IAPT (Improving Access to Psychological Therapies) and include Cognitive Behavioural Therapy (CBT) or Interpersonal Therapy (IPT) Ask about OTC/Herbal/St John’s Wort use – NO SSRI to be prescribed if already on St John’s Wort or stop St John’s Wort Consider referral to specialist care early if the patient has significant suicidal ideation, severe depression, depression in bipolar disorder. MODERATE to SEVERE DEPRESSION Discuss medication and treatment options with patient before prescribing, include side effects and risk of suicidal thoughts during onset of treatment. Consider patients co-morbidities when selecting antidepressant and ask about OTC/Herbal/St John’s Wort as described above. Refer to IAPT - Psychological therapies should be continued alongside medication. Ensure adequate duration of treatment has been tried before switching medication or increasing dose. CITALOPRAM 20mg daily or SERTRALINE 50mg daily Citalopram – consider Dose 10mg for 10days then Assess efficacy over 6-8 weeks. If effective see box 1 titration 20mg for 6-8 weeks Ineffective Sertraline – consider Poorly 25mg for 10days then tolerated 50mg for 6-8 weeks Increase to: Citalopram 30mg OD, Switch to fluoxetine or increase to 40mg after 6 line another SSRI or Mirtazapine. st weeks if required (MAX dose 1 Cross-taper when switching. Box 1. in elderly = 20mg) Increase to therapeutic dose. -

Citalopram/Escitalopram (Celexa/Lexapro
Citalopram | Escitalopram (Celexa® | Lexapro®) This sheet is about using citalopram/escitalopram in a pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare provider. What is citalopram and escitalopram? Citalopram is a medication used to treat depression. Citalopram belongs to the class of antidepressants known as selective serotonin reuptake inhibitors (SSRIs). A common brand name for citalopram is Celexa®. The drug escitalopram contains the same active medication as citalopram. These two drugs act in the body in a very similar way. Escitalopram is used to treat depression and generalized anxiety disorder. It is also an SSRI and is sold under the brand name Lexapro®. Sometimes when people find out they are pregnant, they think about changing how they take their medication, or stopping their medication altogether. However, it is important to talk with your healthcare providers before making any changes to how you take this medication. Your healthcare providers can talk with you about the benefits of treating your condition and the risks of untreated illness during pregnancy. Should you choose to stop taking this medication, it is important to have other forms of support in place (e.g. counseling or therapy) and a plan to restart the medication after delivery, if needed. I take citalopram/escitalopram. Can it make it harder for me to get pregnant? It is not known if citalopram/escitalopram can make it harder to get pregnant. Studies in animals found that citalopram might cause some reduced fertility (ability to get pregnant). Does taking citalopram/escitalopram increase the chance for miscarriage? Miscarriage can occur in any pregnancy. -

Citalopram Distribution in Postmortem Cases
Journal of Analytical Toxicology, Vol. 25, October 2001 Case Report[ Citalopram Distribution in Postmortem Cases Barry Levine*, Xiang Zhang, and John E. Smialek Office of the Chief Medical Examiner, Stateof Maryland, 111 Penn Street, Baltimore, Maryland Gary W. Kunsman and Michael E. Fronlz Bexar County Medical Examiner's Office, 7337 Louis PasteurDrive, San Antonio, Texas78229 Downloaded from https://academic.oup.com/jat/article/25/7/641/729633 by guest on 27 September 2021 Abstract I N-desmethylcitalopram, N-didesmethylcitalopram, citalopram N-oxide, and a propionic acid metabolite. Only parent drug and This is a report of the analytical findings in 13 cases investigated by the desmethyl metabolite appear in the urine in amounts greater either the Office of the Chief Medical Examiner, State of Maryland than 10% of a dose (4). Steady-state plasma therapeutic concen- or the Bexar County (San Antonio, TX) Medical Examiner's Office trations of citalopram are in the range of 0.04 to 0.1 mg/L (5,6). in which citalopram, a highly selective serotonin reuptake inhibitor Although citalopram has been available in Europe as an anti- used therapeutically as an antidepressant, was identified. In 8 of depressant since the 1980s, the drug has only recently been the 9 cases in which both blood and urine specimens were approved for use in the United States. The following is a summary received, the urine citalopram concentration exceeded the blood of the analytical findings in cases reported to the Office of the concentration, indicating that urine is an appropriate specimen for Chief Medical Examiner, State of Maryland and the Bexar County screening citalopram use. -

Long-Term Administration of Citalopram Reduces Basal and Stress-Induced Extracellular Noradrenaline Levels in Rat Brain
Psychopharmacology (2007) 194:73–81 DOI 10.1007/s00213-007-0826-8 ORIGINAL INVESTIGATION Long-term administration of citalopram reduces basal and stress-induced extracellular noradrenaline levels in rat brain Yukie Kawahara & Hiroshi Kawahara & Fumi Kaneko & Masatoshi Tanaka Received: 24 December 2006 /Accepted: 7 May 2007 /Published online: 30 May 2007 # Springer-Verlag 2007 Abstract suppressed only in the LC. The effect of local application of Rationale Panic disorders are commonly treated with clonidine was enhanced only in the BLA. selective serotonin reuptake inhibitors (SSRIs). However, Conclusion The present results indicate that chronic ad- the effect of SSRIs on noradrenaline systems in the brain ministration of citalopram strongly decreases the extracel- has not been fully elucidated at the present time. lular levels of noradrenaline in the brain. The anti-panic Objectives The effects of long-term administration of effect of citalopram might be due to sensitization of the α2- citalopram, an SSRI, on basal as well as stress-induced adrenoceptors leading to suppression of the stress response extracellular noradrenaline levels in the basolateral nucleus through noradrenergic activity. This mechanism is specific of the amygdala (BLA) and the locus coeruleus (LC) were for the BLA. determined. In addition, the responsiveness of noradren- aline transporters and α2-adrenoceptors were determined Keywords Citalopram . Microdialysis . Amygdala . after long-term administration of citalopram. Basolateral . Rat . Noradrenaline . Chronic treatment -

Escitalopram Oxalate
HIGHLIGHTS OF PRESCRIBING INFORMATION --------------WARNINGS AND PRECAUTIONS------------ These highlights do not include all the information Clinical Worsening/Suicide Risk: Monitor for clinical needed to use Lexapro® safely and effectively. See full worsening, suicidality and unusual change in behavior, prescribing information for Lexapro®. especially, during the initial few months of therapy or at times of dose changes (5.1). Lexapro® (escitalopram oxalate) Tablets Serotonin Syndrome: Serotonin syndrome has been Lexapro® (escitalopram oxalate) Oral Solution reported with SSRIs and SNRIs, including Lexapro, both Initial U.S. Approval: 2002 when taken alone, but especially when co-administered WARNING: Suicidality and Antidepressant Drugs with other serotonergic agents (including triptans, See full prescribing information for complete boxed tricyclic antidepressants, fentanyl, lithium, tramadol, warning. tryptophan, buspirone, amphetamines, and St. John’s Increased risk of suicidal thinking and behavior in Wort). If such symptoms occur, discontinue Lexapro and children, adolescents and young adults taking initiate supportive treatment. If concomitant use of antidepressants for major depressive disorder (MDD) Lexapro with other serotonergic drugs is clinically and other psychiatric disorders. Lexapro is not warranted, patients should be made aware of a potential approved for use in pediatric patients less than 12 increased risk for serotonin syndrome, particularly during years of age (5.1). treatment initiation and dose increases (5.2). Discontinuation of Treatment with Lexapro: A gradual reduction in dose rather than abrupt cessation is -------------------RECENT MAJOR CHANGES---------------- recommended whenever possible (5.3). Warnings and Precautions (5.2) 1/2017 Seizures: Prescribe with care in patients with a history of seizure (5.4). --------------INDICATIONS AND USAGE------------------- Activation of Mania/Hypomania: Use cautiously in Lexapro® is a selective serotonin reuptake inhibitor (SSRI) patients with a history of mania (5.5). -

Citaloprami a Review of Pharmacological and Clinical Effects
Citaloprami a review of pharmacological and clinical effects Kalyna Bezchlibnyk-Butler, BScPhm; Ivana Aleksic, BSc; Sidney H. Kennedy, MD Bezchlibnyk-Butler Department of Pharmacy, and Centre for Addiction and Mental Health (CAMH), Toronto, Ont., and Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton, Alta.; Aleksic CAMH; Kennedy CAMH and Department of Psychiatry, University of Toronto, Toronto, Ont. Objective: To provide clinicians with a critical evaluation of citalopram, a selective serotonin reuptake inhibitor (SSRI) that has been available in Canada since March 1999. Data sources: Commercial search- es (MEDLINE and BiblioTech) and an "in-house" search (InfoDrug) were used to find published English-lan- guage references for clinical and preclinical publications. There was no restriction of publication dates. Primary index terms used were: pharmacological properties, receptors, pharmacological selectivity, phar- macokinetics, age-related pharmacokinetics, sex-related pharmacokinetics, renal dysfunction, hepatic dys- function, cytochrome activity, drug interactions, adverse reactions, antidepressant switching, precautions, overdose, drug discontinuation, children, geriatric, depression, combination therapy, placebo control, refractory depression, anxiety disorders and medical disorders. Study selection: A total of 74 studies were reviewed. Twenty-one of these studies specifically examined the clinical efficacy and tolerability of citalopram in depressive disorders as well as other disorders. In depressive disorders, clinical studies were required to have either placebo or active comparison controls for a minimum of 3 weeks. For other dis- orders, in the absence of double-blind trials, open-label studies were included. Pharmacological studies were limited to animal studies focusing on citalopram's selectivity and receptor specificity, and positron emission tomography studies were incorporated to include human pharmacological data.