Drug Interactions with Antidepressants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Switching from Clonidine Immediate-Release to Guanfacine Extended-Release
/ DE L’ACADÉMIE CANADIENNE DE PSYCHIATRIE DE L’ENFANT ET DE L’ADOLESCENT PSYCHOPHARMACOLOGY Switching from Clonidine Immediate-Release to Guanfacine Extended-Release Dean Elbe PharmD, BCPP1,2,3 s a clinical pharmacy specialist in child and adolescent (Canada) Ltd, 2012b). Clonidine has been used off-label Amental health, I am frequently asked how to switch in children for many years for treatment of insomnia, patients from clonidine immediate-release (IR) to guanfa- ADHD, and disruptive behaviour disorders (Hunt, Capper cine extended-release (XR). This therapeutic switch may be & O’Connell, 1990; Rubinstein; Jaselskis, Cook, Fletcher required when poor adherence to a clonidine IR regimen & Leventhal, 1992; Silver & Licamele, 1994; Palumbo et (typically requiring 3–4 doses daily) is identified, when al., 2008; Efron, Lycett & Sciberras, 2014). A clonidine XR clonidine dose-optimization is limited by sedation, brady- formulation is not available in Canada, but is available in cardia or hypotension, or when coverage situations change. the United States for treatment of ADHD (Concordia Phar- The latter may occur if, for example, new eligibility for a maceuticals, Inc. 2015). government program or a third party-payer occurs. Weight-based dosing guidelines exist for clonidine IR Guanfacine XR, a selective alpha2A agonist, was first mar- (0.003–0.008 mg/kg/day) and guanfacine XR (0.05–0.08 keted in Canada in late 2013 for the treatment of attention mg/kg/day) (Shire Pharma Canada ULC, 2019; Elbe et deficit hyperactivity disorder (ADHD) in children and ado- al., 2018). Based on these guidelines and other literature, lescents (Shire Pharma Canada ULC, 2019). -

Drug Class Review Beta Adrenergic Blockers
Drug Class Review Beta Adrenergic Blockers Final Report Update 4 July 2009 Update 3: September 2007 Update 2: May 2005 Update 1: September 2004 Original Report: September 2003 The literature on this topic is scanned periodically. The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Mark Helfand, MD, MPH Kim Peterson, MS Vivian Christensen, PhD Tracy Dana, MLS Sujata Thakurta, MPA:HA Drug Effectiveness Review Project Marian McDonagh, PharmD, Principal Investigator Oregon Evidence-based Practice Center Mark Helfand, MD, MPH, Director Oregon Health & Science University Copyright © 2009 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 4 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION .......................................................................................................................... 6 Purpose and Limitations of Evidence Reports........................................................................................ 8 Scope and Key Questions .................................................................................................................... 10 METHODS................................................................................................................................. -

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Isoflurane Produces Antidepressant Effects and Induces Trkb Signaling in Rodents
bioRxiv preprint doi: https://doi.org/10.1101/084525; this version posted July 11, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Isoflurane produces antidepressant effects and induces TrkB signaling in rodents Hanna Antilaa, Maria Ryazantsevaa,b, Dina Popovaa, Pia Sipiläa, Ramon Guiradoa, Samuel Kohtalaa,b, Ipek Yalcinc, Jesse Lindholma, Liisa Vesaa, Vinicius Satod, Joshua Cordeirae, Henri Autioa, Mikhail Kislina, Maribel Riose, Sâmia Jocad, Plinio Casarottoa, Leonard Khirouga, Sari Lauria,b, Tomi Tairaa,f, Eero Castréna* and Tomi Rantamäkia,b* aNeuroscience Center, P.O. Box 56, FI-00014 University of Helsinki, Helsinki, Finland. bDivision of Physiology and Neuroscience, Department of Biosciences, Faculty of Biological and Environmental Sciences, P.O. Box 66, FI-00014 University of Helsinki, Helsinki, Finland. cInstitut des Neurosciences Cellulaires et Intégratives, Centre National de la Recherche Scientifique, FR-67084 Strasbourg Cedex, France. dSchool of Pharmaceutical Sciences of Ribeirão Preto 14040-903, Brazil. eTufts University, Boston, MA, USA. fDepartment of Veterinary Biosciences, Faculty of Veterinary Medicine P.O. Box 66, FI-00014 University of Helsinki, Helsinki, Finland. *To whom correspondence should be addressed at: Eero Castrén ([email protected]) or Tomi Rantamäki ([email protected]) A brief burst-suppressing isoflurane anesthesia has been shown to rapidly alleviate symptoms of depression in a subset of patients, but the neurobiological basis of these observations remains obscure. We show that a single isoflurane anesthesia produces antidepressant-like behavioural effects in the learned helplessness paradigm and regulates molecular events implicated in the mechanism of action of rapid-acting antidepressant ketamine: activation of brain-derived neurotrophic factor (BDNF) receptor TrkB, facilitation of mammalian target of rapamycin (mTOR) signaling pathway and inhibition of glycogen synthase kinase 3β (GSK3β). -

Pharmacokinetic Interactions of Drugs with St John's Wort
http://www.paper.edu.cn Pharmacokinetic interactions of Journal of Psychopharmacology 18(2) (2004) 262–276 © 2004 British Association drugs with St John’s wort for Psychopharmacology ISSN 0269-8811 SAGE Publications Ltd, London, Thousand Oaks, CA and New Delhi 10.1177/0269881104042632 Shufeng Zhou Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Eli Chan Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Shen-Quan Pan Department of Biological Sciences, Faculty of Science, National University of Singapore, Singapore. Min Huang Institute of Clinical Pharmacology, School of Pharmaceutical Sciences, Sun Yat-Sen University, Guangzhou 510089, PR China. Edmund Jon Deoon Lee Department of Pharmacology, Faculty of Medicine, National University of Singapore, Singapore. Abstract There is a worldwide increasing use of herbs which are often cancer patients receiving irinotecan treatment. St John’s wort did not administered in combination with therapeutic drugs, raising the alter the pharmacokinetics of tolbutamide, but increased the incidence potential for herb–drug interactions. St John’s wort (Hypericum of hypoglycaemia. Several cases have been reported that St John’s wort perforatum) is one of the most commonly used herbal antidepressants. A decreased cyclosporine blood concentration leading to organ rejection. literature search was performed using Medline (via Pubmed), Biological St John’s wort caused breakthrough bleeding and unplanned pregnancies Abstracts, Cochrane Library, AMED, PsycINFO and Embase (all from their when used concomitantly with oral contraceptives. It also caused inception to September 2003) to identify known drug interaction with serotonin syndrome when coadministered with selective serotonin- St John’s wort. The available data indicate that St John’s wort is a reuptake inhibitors (e.g. -

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -

M2021: Pharmacogenetic Testing
Pharmacogenetic Testing Policy Number: AHS – M2021 – Pharmacogenetic Prior Policy Name and Number, as applicable: Testing • M2021 – Cytochrome P450 Initial Presentation Date: 06/16/2021 Revision Date: N/A I. Policy Description Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome (CYP) P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. CYP P450 are essential to produce many biochemical building blocks, such as cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in CYP P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased levels of toxic substances in the body. Approximately 58 CYP genes are in humans (Bains, 2013; Tantisira & Weiss, 2019). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. Azathioprine and mercaptopurine are used for treatment of nonmalignant immunologic disorders; mercaptopurine is used for treatment of lymphoid malignancies; and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011). Dihydropyrimidine dehydrogenase (DPD), encoded by the gene DPYD, is a rate-limiting enzyme responsible for fluoropyrimidine catabolism. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors, such as colorectal, breast, and aerodigestive tract tumors (Amstutz et al., 2018). A variety of cell surface proteins, such as antigen-presenting molecules and other proteins, are encoded by the human leukocyte antigen genes (HLAs). -

CYP3A4 Mediated Pharmacokinetics Drug Interaction Potential of Maha
www.nature.com/scientificreports OPEN CYP3A4 mediated pharmacokinetics drug interaction potential of Maha‑Yogaraj Gugglu and E, Z guggulsterone Sarvesh Sabarathinam1, Satish Kumar Rajappan Chandra2 & Vijayakumar Thangavel Mahalingam1* Maha yogaraja guggulu (MYG) is a classical herbomineral polyherbal formulation being widely used since centuries. The aim of this study was to investigate the efect of MYG formulation and its major constituents E & Z guggulsterone on CYP3A4 mediated metabolism. In vitro inhibition of MYG and Guggulsterone isomers on CYP3A4 was evaluated by high throughput fuorometric assay. Eighteen Adult male Sprague–Dawley rats (200 ± 25 g body weight) were randomly divided into three groups. Group A, Group B and Group C were treated with placebo, MYG and Standard E & Z guggulsterone for 14 days respectively by oral route. On 15th day, midazolam (5 mg/kg) was administered orally to all rats in each group. Blood samples (0.3 mL) were collected from the retro orbital vein at 0.25, 0.5, 0.75, 1, 2, 4, 6, 12 and 24 h of each rat were collected. The fndings from the in vitro & in vivo study proposed that the MYG tablets and its guggulsterone isomers have drug interaction potential when consumed along with conventional drugs which are CYP3A4 substrates. In vivo pharmacokinetic drug interaction study of midazolam pointed out that the MYG tablets and guggulsterone isomers showed an inhibitory activity towards CYP3A4 which may have leads to clinically signifcant interactions. Te use of alternative medicine such as herbal medicines, phytonutrients, ayurvedic products and nutraceuticals used widely by the majority of the patients for their primary healthcare needs. -

Memory Deficits Associated with Clonidine
Letter to the Editor Letters to the Editor are invited for comment on a topic of current interest or on Table material published in GENERAL HOSPITAL PSYCHIATRY. Letters should be typed doubled spaced and are subject to editing according to space limitations. - Memory Deficits Associated with Attent KnO Clonidine WA Verbal WA Drugs used in the treatment of essential hyperten- Initiation of clonidine therapy (0.1 mg b.i.d.) in WA sion are among the most commonly prescribed. April 1984 resulted in well-controlled hypertension Tactilc Some of these agents have primary effects on neu- without immediately apparent adverse effects. Fulc rotransmitter systems and are centrally active. However, the coincidence of the onset of memory Verba Thus, drugs such as a-methyldopa, propranalol, complaints and the beginning of clonidine treat- 3% ment suggested that clonidine might be respon- List Ll and reserpine have well-established neuropsychia- Fulc tric complications, ranging from depression to cog- sible. si nitive impairments and psychosis [l].Since the use After consultation with the patient's internist, a R of these drugs is widespread and unavoidable, we switch was made to captopril, an angiotensin-con- T must be alert to the possibility that these drugs verting enzyme inhibitor. Before the change we T administered tests of attention, concentration, and contribute to psychologic complaints and symp- -R toms of our patients. verbal skills as well as the Fuld Object-Memory Evaluation, which includes a measure of verbal 'Age-a Clonidine, a presynaptic adrenergic a2agonist, bNonc has become well established as a useful and rela- fluency as well as a selective reminding list learning tively safe therapeutic agent. -
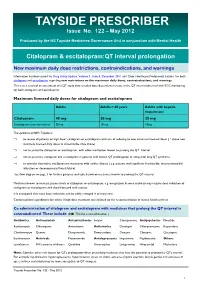
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

TRANDATE® (Labetalol Hydrochloride) Tablets
NDA 18716/S-026 Page 2 PRODUCT INFORMATION TRANDATE® (labetalol hydrochloride) Tablets DESCRIPTION: Trandate Tablets are adrenergic receptor blocking agents that have both selective alpha1-adrenergic and nonselective beta-adrenergic receptor blocking actions in a single substance. Labetalol hydrochloride (HCl) is a racemate chemically designated as 2-hydroxy-5-[1-hydroxy-2-[(1 methyl-3-phenylpropyl)amino]ethyl]benzamide monohydrochloride, and it has the following structure: Labetalol HCl has the empirical formula C19H24N2O3•HCl and a molecular weight of 364.9. It has two asymmetric centers and therefore exists as a molecular complex of two diastereoisomeric pairs. Dilevalol, the R,R′ stereoisomer, makes up 25% of racemic labetalol. Labetalol HCl is a white or off-white crystalline powder, soluble in water. Trandate Tablets contain 100, 200, or 300 mg of labetalol HCl and are taken orally. The tablets also contain the inactive ingredients corn starch, FD&C Yellow No. 6 (100- and 300-mg tablets only), hydroxypropyl methylcellulose, lactose, magnesium stearate, pregelatinized corn starch, sodium benzoate (200-mg tablet only), talc (100-mg tablet only), and titanium dioxide. CLINICAL PHARMACOLOGY: Labetalol HCl combines both selective, competitive, alpha1-adrenergic blocking and nonselective, competitive, beta-adrenergic blocking activity in a single substance. In man, the ratios of alpha- to beta-blockade have been estimated to be approximately 1:3 and 1:7 following oral and intravenous (IV) administration, respectively. Beta2-agonist activity has been demonstrated in animals with minimal beta1-agonist (ISA) activity detected. In animals, at doses greater than those required for alpha- or beta-adrenergic blockade, a membrane stabilizing effect has been demonstrated.