Selective Serotonin Reuptake Inhibitors and Adverse Effects: a Narrative Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Acute Extrapyramidal Symptoms Following Abrupt Discontinuation of Propranolol
Medical Journal of the Volume 14 Islamic Republic of Iran Number 3 Fall 1379 November 2000 ACUTE EXTRAPYRAMIDAL SYMPTOMS FOLLOWING ABRUPT DISCONTINUATION OF PROPRANOLOL A. ALAVIAN GHAVANINI From the Center Jor Research Consultation, School oj Medicine, Shiraz University ojMedical Sciences, Shiraz, I.R. Iran. ABSTRACT A case of acute extrapyramidal manifestations consisting of dystonia and akathisia following abrupt discontinuation of propranolol is reported. She re sponded well to oral propranolol and intramuscular diazepam. Extrapyramidal symptoms have commonly been associated with acute or chronic administration of neuroleptic drugs. There have been reports of a substantial number of cases with similar clinical characteristics associated with tricyclic antidepressants, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors. Al though it is known that beta-adrenoceptor antagonists are effective in the treat ment of extrapyramidal symptoms, especially akathisia, there has been no previ ous report of such symptoms induced by abrupt withdrawal of these drugs. Al though she had been on low dose amitriptyline and had discontinued this medica tion long before, prolonged use of amitriptyline may have had a predisposing role in the development of these symptoms. MJIRL Vol. 14, No.3, 305-306, 2000. Keywords: Propranolol; Extrapyramidal symptoms; Beta-adrenoceptor antagonists. INTRODUCTION She described a feeling of "being pulled down by gravity." She had never experienced such symptoms before. Thor Extrapyramidal symptoms include acute dystonias, ough physical examination with special focus on the ner akathisia, Parkinson's syndrome, and tardive dyskinesia. vous system was unremarkable except for the involuntary These symptoms are common manifestations of neurolep contraction of jaw muscles and a fine tremor in her ex tic drugs. -

Prevalence of Extrapyramidal Side Effects in Patients on Antipsychotics Drugs at a Tertiary Care Center
f Ps al o ych rn ia u tr o y J Kirgaval et al., J Psychiatry 2017, 20:5 Journal of Psychiatry DOI: 10.4172/2378-5756.1000419 ISSN: 2378-5756 Research Article Open Access Prevalence of Extrapyramidal Side Effects in Patients on Antipsychotics Drugs at a Tertiary Care Center5 Ramprasad Santhanakrishna Kirgaval1*, Srinivas Revanakar2 and Chidanand Srirangapattna2 1Department of Psychiatry, Shimoga Institute of Medical Sciences, Shimoga, Karnataka, India 2Department of Pharmacology, Shimoga Institute of Medical Sciences, Shimoga, Karnataka, India Abstract Background: Antipsychotic drugs are associated with adverse effects that can lead to poor medication adherence, stigma, distress and impaired quality of life. Among the various side effects of anti-psychotics extra pyramidal symptoms constitute one of the important side effects interfering with the compliance of the patients towards medication. Objective: Evaluation of extrapyramidal side effects by AIMS in patients who are on antipsychotics. Results: The extrapyramidal symptoms were more commonly seen in males (62.85%), the age of incidence of maximum in the age group of 34.28, Maximum was seen among the patients on the Risperidone (45.7%), Involvement of the extremities was common (42.85%) and 64.28% of individuals had moderate severity and 54.28% of individuals were aware of the extrapyramidal symptoms which provided mild distress. Conclusion: Extrapyramidal symptoms are one of the commonest side effect of the antipsychotics interfering with compliance of the patients towards adherence to medications, thereby decreasing the efficacy. Keywords: Extrapyramidal symptoms; Compliance; Antipsychotics; positive symptom of the psychosis but have some serious limitations AIMS. such as lack of efficacy against negative symptoms and adverse effects like extrapyramidal symptoms [7]. -

Modern Antipsychotic Drugs: a Critical Overview
Review Synthèse Modern antipsychotic drugs: a critical overview David M. Gardner, Ross J. Baldessarini, Paul Waraich Abstract mine was based primarily on the finding that dopamine ago- nists produced or worsened psychosis and that antagonists CONVENTIONAL ANTIPSYCHOTIC DRUGS, used for a half century to treat were clinically effective against psychotic and manic symp- a range of major psychiatric disorders, are being replaced in clini- 5 toms. Blocking dopamine D2 receptors may be a critical or cal practice by modern “atypical” antipsychotics, including ari- even sufficient neuropharmacologic action of most clinically piprazole, clozapine, olanzapine, quetiapine, risperidone and effective antipsychotic drugs, especially against hallucina- ziprasidone among others. As a class, the newer drugs have been promoted as being broadly clinically superior, but the evidence for tions and delusions, but it is not necessarily the only mecha- this is problematic. In this brief critical overview, we consider the nism for antipsychotic activity. Moreover, this activity, and pharmacology, therapeutic effectiveness, tolerability, adverse ef- subsequent pharmacocentric and circular speculations about fects and costs of individual modern agents versus older antipsy- altered dopaminergic function, have not led to a better un- chotic drugs. Because of typically minor differences between derstanding of the pathophysiology or causes of the several agents in clinical effectiveness and tolerability, and because of still idiopathic psychotic disorders, nor have they provided a growing concerns about potential adverse long-term health conse- non-empirical, theoretical basis for the design or discovery quences of some modern agents, it is reasonable to consider both of improved treatments for psychotic disorders. older and newer drugs for clinical use, and it is important to inform The neuropharmacodynamics of specific modern anti- patients of relative benefits, risks and costs of specific choices. -

Clomipramine | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Clomipramine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Anafranil Brand Names: Canada Anafranil; MED ClomiPRAMINE; TARO-Clomipramine Warning Drugs like this one have raised the chance of suicidal thoughts or actions in children and young adults. The risk may be greater in people who have had these thoughts or actions in the past. All people who take this drug need to be watched closely. Call the doctor right away if signs like low mood (depression), nervousness, restlessness, grouchiness, panic attacks, or changes in mood or actions are new or worse. Call the doctor right away if any thoughts or actions of suicide occur. This drug is not approved for use in all children. Talk with the doctor to be sure that this drug is right for your child. What is this drug used for? It is used to treat obsessive-compulsive problems. It may be given to you for other reasons. Talk with the doctor. Clomipramine 1/8 What do I need to tell my doctor BEFORE I take this drug? If you have an allergy to clomipramine or any other part of this drug. If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have had a recent heart attack. If you are taking any of these drugs: Linezolid or methylene blue. -

Meta-Analysis of the Dose-Response Relationship of SSRI in Obsessive
Molecular Psychiatry (2010) 15, 850–855 & 2010 Macmillan Publishers Limited All rights reserved 1359-4184/10 www.nature.com/mp ORIGINAL ARTICLE Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder MH Bloch1, J McGuire1, A Landeros-Weisenberger1, JF Leckman1 and C Pittenger2 1Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA and 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA We sought to determine differences in efficacy and tolerability between different doses of selective serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder (OCD) using meta-analysis. We identified 9 studies involving 2268 subjects that were randomized, double-blind placebo-controlled clinical trials that compared multiple, fixed- doses of selective serotonin reuptake inhibitors (SSRIs) to each other and to placebo in the treatment of adults with OCD. Change in Y-BOCS score, proportion of treatment responders, and dropouts (all-cause and due to side-effects) were determined for each included study. Weighted mean difference was used to examine mean change in Y-BOCS score. Pooled absolute risk difference was used to examine dichotomous outcomes. Meta-analysis was performed using a fixed effects model in RevMan 4.2.8. We found that compared with either low or medium doses, higher doses of SSRIs were associated with improved treatment efficacy, using either Y-BOCS score or proportion of treatment responders as an outcome. Dose of SSRIs was not associated with the number of all-cause dropouts. Higher doses of SSRIs were associated with significantly higher proportion of dropouts due to side-effects. -

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -

Sertraline and Venlafaxine-Induced Nocturnal Enuresis
Case Report DOI: 10.5455/bcp.20140304091103 Sertraline and Venlafaxine-Induced Nocturnal Enuresis Inci Meltem Atay1, Gulin Ozdamar Unal2 ABS TRACT: Sertraline and venlafaxine-induced nocturnal enuresis Nocturnal enuresis is defined as the involuntary discharge of urine after the age of expected continence that occurs during sleep at night. Although there are a few reports in adults for nocturnal enuresis associated 1Assist. Prof., 2M.D., Suleyman Demirel University, School of Medicine, Department with serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs), the of Psychiatry, Isparta - Turkey mechanism or frequency of this side effect have not been identified yet. We report here a case of nocturnal Corresponding author: Dr. İnci Meltem Atay enuresis associated with both sertraline and venlafaxine in different major depressive episodes in an adult Süleyman Demirel Universitesi, Tıp Fakültesi, Psikiyatri Anabilim Dalı, Isparta - Türkiye patient that resolves after the discontinuation of the medications and continuation with escitalopram. To our E-ma il add ress: knowledge, in literature there have been no reports about nocturnal enuresis caused by those two agents in [email protected] the same patient. This case is discussed in detail for the recurrence of nocturnal enuresis, the importance of Date of submission: detailed assessment of even rare side effects and for their possible mechanisms. February 11, 2014 Date of acceptance: March 04, 2014 Keywords: nocturnal enuresis, venlafaxine, sertraline, depression Declaration of interest: I.M.A, G.O.U.: The authors reported no Klinik Psikofarmakoloji Bulteni - Bulletin of Clinical Psychopharmacology 2015;25(3):287-90 conflict of interest related to this article. INTRODUCTION side effect1-6. -
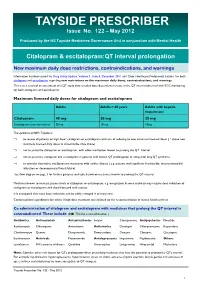
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Pharmacogenetic Testing: a Tool for Personalized Drug Therapy Optimization
pharmaceutics Review Pharmacogenetic Testing: A Tool for Personalized Drug Therapy Optimization Kristina A. Malsagova 1,* , Tatyana V. Butkova 1 , Arthur T. Kopylov 1 , Alexander A. Izotov 1, Natalia V. Potoldykova 2, Dmitry V. Enikeev 2, Vagarshak Grigoryan 2, Alexander Tarasov 3, Alexander A. Stepanov 1 and Anna L. Kaysheva 1 1 Biobanking Group, Branch of Institute of Biomedical Chemistry “Scientific and Education Center”, 109028 Moscow, Russia; [email protected] (T.V.B.); [email protected] (A.T.K.); [email protected] (A.A.I.); [email protected] (A.A.S.); [email protected] (A.L.K.) 2 Institute of Urology and Reproductive Health, Sechenov University, 119992 Moscow, Russia; [email protected] (N.V.P.); [email protected] (D.V.E.); [email protected] (V.G.) 3 Institute of Linguistics and Intercultural Communication, Sechenov University, 119992 Moscow, Russia; [email protected] * Correspondence: [email protected]; Tel.: +7-499-764-9878 Received: 2 November 2020; Accepted: 17 December 2020; Published: 19 December 2020 Abstract: Pharmacogenomics is a study of how the genome background is associated with drug resistance and how therapy strategy can be modified for a certain person to achieve benefit. The pharmacogenomics (PGx) testing becomes of great opportunity for physicians to make the proper decision regarding each non-trivial patient that does not respond to therapy. Although pharmacogenomics has become of growing interest to the healthcare market during the past five to ten years the exact mechanisms linking the genetic polymorphisms and observable responses to drug therapy are not always clear. Therefore, the success of PGx testing depends on the physician’s ability to understand the obtained results in a standardized way for each particular patient. -

Plague Plague
Disease Planning Guide - Plague Mass Post Exposure Prophylaxis I. Disease-specific guidance: The following guide should only be used in events where a plague epidemic has been identified, an Emergency Use Authorization from the Food and Drug Administration has been issued and a state and local emergency declaration has been issued by the proper authorities. Model Standing Order – Pg 1 Clients will arrive at dispensing sites with a voucher indicating which medication, if any, they should receive. Specific guidance related to dispensing is shown in red . Model Standing Order – Pg 2 Clients that present this voucher will not receive medication for the individual named on the form. Dispensers may collect “Do Not Dispense Medication” vouchers for records purposes. Model Standing Order – Pg 3 II. PERSONS FOR WHOM PROPHYLAXIS MAY BE ORDERED Persons who have a confirmed or suspect exposure to Yersinia pestis, the causative agent of plague, as determined by the local or State Health Officer. Table 1: Recommended Post-Exposure Prophylaxis for Inhalational Plague Patient Category Therapy Recommendation Duration 10 days Adults Doxycycline , 100 mg PO BID or Ciprofloxacin , 500 mg PO BID 10 days Ciprofloxacin , 15 mg/kg PO BID, max 500 mg/dose or Doxycycline : >45 kg: 100 mg PO BID Children <45 kg: 2.2 mg/kg PO BID ***************************************** If susceptibility to penicillin has been confirmed: Amoxicillin : >20 kg: 500 mg PO TID <20 kg: 80 mg/kg/day PO divided TID 10 days Doxycycline , 100 mg PO BID or Pregnant women Ciprofloxacin , 500 mg PO BID ***************************************** If susceptibility to penicillin has been confirmed: Amoxicillin 500 mg PO TID 10 days Immunocompromised Doxycycline , 100 mg PO BID or Ciprofloxacin , 500 mg PO BID Adapted from: Working Group on Civilian Biodefense.