Impact of Citalopram and Fluvoxamine on Platelet Response To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Meta-Analysis of the Dose-Response Relationship of SSRI in Obsessive
Molecular Psychiatry (2010) 15, 850–855 & 2010 Macmillan Publishers Limited All rights reserved 1359-4184/10 www.nature.com/mp ORIGINAL ARTICLE Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder MH Bloch1, J McGuire1, A Landeros-Weisenberger1, JF Leckman1 and C Pittenger2 1Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA and 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA We sought to determine differences in efficacy and tolerability between different doses of selective serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder (OCD) using meta-analysis. We identified 9 studies involving 2268 subjects that were randomized, double-blind placebo-controlled clinical trials that compared multiple, fixed- doses of selective serotonin reuptake inhibitors (SSRIs) to each other and to placebo in the treatment of adults with OCD. Change in Y-BOCS score, proportion of treatment responders, and dropouts (all-cause and due to side-effects) were determined for each included study. Weighted mean difference was used to examine mean change in Y-BOCS score. Pooled absolute risk difference was used to examine dichotomous outcomes. Meta-analysis was performed using a fixed effects model in RevMan 4.2.8. We found that compared with either low or medium doses, higher doses of SSRIs were associated with improved treatment efficacy, using either Y-BOCS score or proportion of treatment responders as an outcome. Dose of SSRIs was not associated with the number of all-cause dropouts. Higher doses of SSRIs were associated with significantly higher proportion of dropouts due to side-effects. -

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -
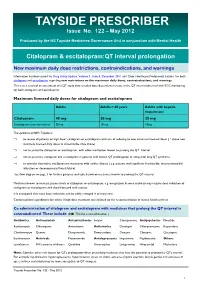
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Doxepin Exacerbates Renal Damage, Glucose Intolerance, Nonalcoholic Fatty Liver Disease, and Urinary Chromium Loss in Obese Mice
pharmaceuticals Article Doxepin Exacerbates Renal Damage, Glucose Intolerance, Nonalcoholic Fatty Liver Disease, and Urinary Chromium Loss in Obese Mice Geng-Ruei Chang 1,* , Po-Hsun Hou 2,3, Wei-Cheng Yang 4, Chao-Min Wang 1 , Pei-Shan Fan 1, Huei-Jyuan Liao 1 and To-Pang Chen 5,* 1 Department of Veterinary Medicine, National Chiayi University, 580 Xinmin Road, Chiayi 60054, Taiwan; [email protected] (C.-M.W.); [email protected] (P.-S.F.); [email protected] (H.-J.L.) 2 Department of Psychiatry, Taichung Veterans General Hospital, 1650 Taiwan Boulevard (Section 4), Taichung 40705, Taiwan; [email protected] 3 Faculty of Medicine, National Yang-Ming University, 155 Linong Street (Section 2), Taipei 11221, Taiwan 4 School of Veterinary Medicine, National Taiwan University, 1 Roosevelt Road (Section 4), Taipei 10617, Taiwan; [email protected] 5 Division of Endocrinology and Metabolism, Show Chwan Memorial Hospital, 542 Chung-Shan Road (Section 1), Changhua 50008, Taiwan * Correspondence: [email protected] (G.-R.C.); [email protected] (T.-P.C.); Tel.: +886-5-2732946 (G.-R.C.); +886-4-7256166 (T.-P.C.) Abstract: Doxepin is commonly prescribed for depression and anxiety treatment. Doxepin-related disruptions to metabolism and renal/hepatic adverse effects remain unclear; thus, the underlying mechanism of action warrants further research. Here, we investigated how doxepin affects lipid Citation: Chang, G.-R.; Hou, P.-H.; change, glucose homeostasis, chromium (Cr) distribution, renal impairment, liver damage, and fatty Yang, W.-C.; Wang, C.-M.; Fan, P.-S.; liver scores in C57BL6/J mice subjected to a high-fat diet and 5 mg/kg/day doxepin treatment for Liao, H.-J.; Chen, T.-P. -
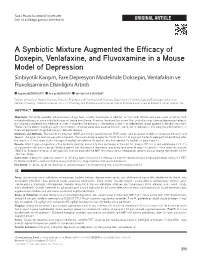
A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
Turk J Pharm Sci 2020;17(3):293-298 DOI: 10.4274/tjps.galenos.2019.94210 ORIGINAL ARTICLE A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine, and Fluvoxamine in a Mouse Model of Depression Sinbiyotik Karışım, Fare Depresyon Modelinde Doksepin, Venlafaksin ve Fluvoksaminin Etkinliğini Artırdı Azadeh MESRIPOUR1*, Andiya MESHKATI1, Valiollah HAJHASHEMI2 1Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Department of Pharmacology and Toxicology, Isfahan, Iran 2Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Isfahan Pharmaceutical Sciences Research Center, Isfahan, Iran ABSTRACT Objectives: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicine in order to augment the efficacy of therapeutic doses of antidepressant drugs appears to be very important. Therefore, the effect of adding a synbiotic mixture to drinking water was assessed in a mouse model of depression following the administration of three antidepressant drugs belonging to different classes. Materials and Methods: The marble burying test (MBT) and forced swimming test (FST) were used as animal models of obsessive behavior and despair. The synbiotic mixture was administered to the mice’s drinking water (6.25x106 CFU) for 14 days and the tests were performed 30 min after the injection of the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg) on days 7 and 14. Results: After 7 days of ingestion of the synbiotic mixture, immobility time decreased in the FST for doxepin (92±5.5 s) and venlafaxine (17.3±2.5 s) compared to the control group (drinking water), but fluvoxamine decreased immobility time after 14 days of ingestion of the synbiotic mixture (70±7.5 s). -

(12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed Et Al
US0078.93053B2 (12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed et al. (45) Date of Patent: Feb. 22, 2011 (54) TREATING PSYCHOLOGICAL CONDITIONS WO WO 2006/127418 11, 2006 USING MUSCARINIC RECEPTORM ANTAGONSTS (75) Inventors: Brian Seed, Boston, MA (US); Jordan OTHER PUBLICATIONS Mechanic, Sunnyvale, CA (US) Chau et al. (Nucleus accumbens muscarinic receptors in the control of behavioral depression : Antidepressant-like effects of local M1 (73) Assignee: Theracos, Inc., Sunnyvale, CA (US) antagonist in the porSolt Swim test Neuroscience vol. 104, No. 3, pp. 791-798, 2001).* (*) Notice: Subject to any disclaimer, the term of this Lind et al. (Muscarinic acetylcholine receptor antagonists inhibit patent is extended or adjusted under 35 chick Scleral chondrocytes Investigative Ophthalmology & Visual U.S.C. 154(b) by 726 days. Science, vol.39, 2217-2231.* Chau D., et al., “Nucleus Accumbens Muscarinic Receptors in the (21) Appl. No.: 11/763,145 Control of Behavioral Depression: Antidepressant-like Effects of Local M1 Antagonists in the Porsolt Swin Test.” Neuroscience, vol. (22) Filed: Jun. 14, 2007 104, No. 3, Jun. 14, 2001, pp. 791-798. Bechtel, W.D., et al., “Biochemical pharmacology of pirenzepine. (65) Prior Publication Data Similarities with tricyclic antidepressants in antimuscarinic effects only.” Arzneimittelforschung, vol. 36(5), pp. 793-796 (May 1986). US 2007/O293480 A1 Dec. 20, 2007 Chau, D.T. et al., “Nucleus accumbens muscarinic receptors in the control of behavioral depression: antidepressant-like effects of local Related U.S. Application Data Mantagonist in the Porsolt Swim test.” Neuroscience, vol. 104(3), (60) Provisional application No. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee
Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee Summary of Safety Alert (December 2011) – http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769 Citalopram and escitalopram are associated with dose-dependent QT interval prolongation and should not be used in those with: congenital long QT syndrome; known pre-existing QT interval prolongation; or in combination with other medicines that prolong the QT interval. ECG measurements should be considered for patients with cardiac disease, and electrolyte disturbances should be corrected before starting treatment. For citalopram, new restrictions on the maximum daily doses now apply: 40 mg for adults; 20 mg for patients older than 65 years; and 20 mg for those with hepatic impairment. For escitalopram, the maximum daily dose for patients older than 65 years is now reduced to 10 mg/day; other doses remain unchanged. Recommended actions for prescribers If dose is above maximum recommended dose or patient is taking other medications likely to prolong QTc: Need for more than 1. Discuss with service user/patient. citalopram 40mg daily 2. Consider continued need for citalopram and/or alternative therapies (adults), 20mg daily (elderly and reduced hepatic function) e.g. for OCD, PTSD Adult citalopram Elderly (or other risk factors) Taking ANY other medicines Elderly and escitalopram dose above citalopram dose above likely to cause QTc dose above 10mg daily: prolongation 40mg daily: 20mg daily: Consider risk/benefit with service user. Switch if 1-Consider switching relevant possible medication to alternative with no Monitor If under 18 refer to CAMHS effect on QTc prolongation or Reduce dose stepwise to 40mg citalopram daily for adults (unlicensed use). -

Mid Essex CCG 'Guidance for the Treatment of Depression in Adults'
Guidance for the treatment of depression in adults MILD DEPRESSION - Medication is not first-line treatment or only treatment for depression Actively monitor symptoms, give life style advice, guided self- help or exercise MODERATE DEPRESSION Consider psychological intervention. This is accessed by referral or self-referral to Mid Essex IAPT (Improving Access to Psychological Therapies) and include Cognitive Behavioural Therapy (CBT) or Interpersonal Therapy (IPT) Ask about OTC/Herbal/St John’s Wort use – NO SSRI to be prescribed if already on St John’s Wort or stop St John’s Wort Consider referral to specialist care early if the patient has significant suicidal ideation, severe depression, depression in bipolar disorder. MODERATE to SEVERE DEPRESSION Discuss medication and treatment options with patient before prescribing, include side effects and risk of suicidal thoughts during onset of treatment. Consider patients co-morbidities when selecting antidepressant and ask about OTC/Herbal/St John’s Wort as described above. Refer to IAPT - Psychological therapies should be continued alongside medication. Ensure adequate duration of treatment has been tried before switching medication or increasing dose. CITALOPRAM 20mg daily or SERTRALINE 50mg daily Citalopram – consider Dose 10mg for 10days then Assess efficacy over 6-8 weeks. If effective see box 1 titration 20mg for 6-8 weeks Ineffective Sertraline – consider Poorly 25mg for 10days then tolerated 50mg for 6-8 weeks Increase to: Citalopram 30mg OD, Switch to fluoxetine or increase to 40mg after 6 line another SSRI or Mirtazapine. st weeks if required (MAX dose 1 Cross-taper when switching. Box 1. in elderly = 20mg) Increase to therapeutic dose. -

Citalopram/Escitalopram (Celexa/Lexapro
Citalopram | Escitalopram (Celexa® | Lexapro®) This sheet is about using citalopram/escitalopram in a pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare provider. What is citalopram and escitalopram? Citalopram is a medication used to treat depression. Citalopram belongs to the class of antidepressants known as selective serotonin reuptake inhibitors (SSRIs). A common brand name for citalopram is Celexa®. The drug escitalopram contains the same active medication as citalopram. These two drugs act in the body in a very similar way. Escitalopram is used to treat depression and generalized anxiety disorder. It is also an SSRI and is sold under the brand name Lexapro®. Sometimes when people find out they are pregnant, they think about changing how they take their medication, or stopping their medication altogether. However, it is important to talk with your healthcare providers before making any changes to how you take this medication. Your healthcare providers can talk with you about the benefits of treating your condition and the risks of untreated illness during pregnancy. Should you choose to stop taking this medication, it is important to have other forms of support in place (e.g. counseling or therapy) and a plan to restart the medication after delivery, if needed. I take citalopram/escitalopram. Can it make it harder for me to get pregnant? It is not known if citalopram/escitalopram can make it harder to get pregnant. Studies in animals found that citalopram might cause some reduced fertility (ability to get pregnant). Does taking citalopram/escitalopram increase the chance for miscarriage? Miscarriage can occur in any pregnancy. -

Tension-Type Headache
Journal ofNeurology, Neurosurgery, and Psychiatry 1996;61:285-290 285 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.61.3.285 on 1 September 1996. Downloaded from A non-selective (amitriptyline), but not a selective (citalopram), serotonin reuptake inhibitor is effective in the prophylactic treatment of chronic tension-type headache Lars Bendtsen, Rigmor Jensen, Jes Olesen Abstract cemed, the most important type of headache.' Objectives-Although the tricyclic anti- Yet remarkably little is known about its patho- depressant amitriptyline is extensively physiology and the treatment available is lim- used in the prophylactic treatment of ited. The only established prophylactic chronic tension-type headache, only few treatment is the tricyclic antidepressant studies have investigated the efficacy of amitriptymine, a non-selective serotonin reup- this treatment and the results are contra- take inhibitor. The efficacy of this treatment dictory. In addition, the new selective has, however, only been investigated in a few serotonin reuptake inhibiting antidepres- placebo controlled studies,3-6 which have sants, which are widely used in depres- reported conflicting results. The scientific sup- sion and of potential value in pain port for the widespread use of amitriptyline in management, have never been investi- the treatment of chronic tension-type gated in a placebo controlled study often- headache, therefore, is scant. sion-type headache. The aim was to The mechanism of action of amitriptyline in evaluate the efficacy of amitriptyline and chronic tension-type headache, as well as in of the selective serotonin reuptake other non-depressive chronic pain states, is inhibitor citalopram in chronic tension- largely unknown, but it is assumed that the type headache.