A Closer Look at Pacritinib: a JAK2/FLT3 Inhibitor for The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Stanford Chem-H Presentation (PDF)
KiNativ® In situ kinase profiling Stanford University ChEM-H confidential @KiNativPlatform Principle of the KiNativ platform • ATP (or ADP) acyl phosphate binds to, and covalently modifies Lysine residues in the active site • Thus, ATP acyl phosphate with a desthiobiotin tag can be used capture and quantitate kinases in a complex lysate Acyl phosphate Desthiobiotin tag ATP 2 ATP acyl phosphate probe covalently modifies kinase in the active site Lysine 2 Lysine 1 3 ATP acyl phosphate probe covalently modifies kinase in the active site Lysine 2 Lysine 1 4 Samples trypsinized, probe-labeled peptides captured with streptavidin, and analyzed by targeted LC-MS2 Identification Quantitation Explicit determination of peptide Integration of signal from MS2 sequence and probe modification site fragment ions from MS2 spectrum 5 Comprehensive Coverage of Protein and Lipid Kinases Protein kinases Atypical kinases Green: Kinases detected on KiNativ Red: Kinases not detected on KiNativ ~80% of known protein and atypical kinases identified on the platform http://www.kinativ.com/coverage/protein-lipid.html 6 Profiling compound(s) on the KiNativ platform Control sample – add probe Sample: Lysate derived from any cell line or tissue from ANY species Treated sample – add inhibitor followed by probe Inhibited kinase Green: Kinases Blue: Probe Gray: Non-kinases Red: Inhibitor 7 Profiling compound(s) on the KiNativ platform Control sample – add probe MS signalMS Sample: Lysate derived from any cell line or tissue from ANY species Treated sample – add inhibitor -

Download Product Insert (PDF)
PRODUCT INFORMATION Pacritinib Item No. 16709 CAS Registry No.: 937272-79-2 Formal Name: 11-[2-(1-pyrrolidinyl)ethoxy]-14,19-dioxa- 5,7,27-triazatetracyclo[19.3.1.12,6.18,12] O heptacosa-1(25),2,4,6(27),8,10,12(26), 16E,21,23-decaene Synonym: SB1518 N N H MF: C28H32N4O3 FW: 472.6 N Purity: ≥98% O Stability: ≥2 years at -20°C Supplied as: A crystalline solid N O UV/Vis.: λmax: 285 nm Laboratory Procedures For long term storage, we suggest that pacritinib be stored as supplied at -20°C. It should be stable for at least two years. Pacritinib is supplied as a crystalline solid. A stock solution may be made by dissolving the pacritinib in the solvent of choice. Pacritinib is soluble in the organic solvent DMSO, which should be purged with an inert gas, at a concentration of approximately 0.5 mg/ml (slightly warmed). Pacritinib is sparingly soluble in aqueous solutions. To enhance aqueous solubility, dilute the organic solvent solution into aqueous buffers or isotonic saline. If performing biological experiments, ensure the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. We do not recommend storing the aqueous solution for more than one day. Description FMS-like tyrosine kinase 3 (FLT3) and Janus kinase 2 (JAK2) are tyrosine kinases that mediate cytokine signaling and are frequently mutated in cancers, particularly acute myeloid leukemia.1,2 Pacritinib is an 1 inhibitor of both FLT3 and JAK2 (IC50s = 22 and 23 nM, respectively). -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Cytokine Signaling in Tumor Progression
Immune Netw. 2017 Aug;17(4):214-227 https://doi.org/10.4110/in.2017.17.4.214 pISSN 1598-2629·eISSN 2092-6685 Review Article Cytokine Signaling in Tumor Progression Myungmi Lee, Inmoo Rhee* Department of Bioscience and Biotechnology, Sejong University, Seoul 05006, Korea Received: Apr 13, 2017 ABSTRACT Revised: Jun 22, 2017 Accepted: Jun 25, 2017 Cytokines are molecules that play critical roles in the regulation of a wide range of normal *Correspondence to functions leading to cellular proliferation, differentiation and survival, as well as in Inmoo Rhee specialized cellular functions enabling host resistance to pathogens. Cytokines released Department of Bioscience and Biotechnology, in response to infection, inflammation or immunity can also inhibit cancer development Sejong University, 209 Neungdong-ro, and progression. The predominant intracellular signaling pathway triggered by cytokines Gwangjin-gu, Seoul 05006, Korea. is the JAK-signal transducer and activator of transcription (STAT) pathway. Knockout mice Tel: +82-2-6935-2432 E-mail: [email protected] and clinical human studies have provided evidence that JAK-STAT proteins regulate the immune system, and maintain immune tolerance and tumor surveillance. Moreover, aberrant Copyright © 2017. The Korean Association of activation of the JAK-STAT pathways plays an undeniable pathogenic role in several types Immunologists of human cancers. Thus, in combination, these observations indicate that the JAK-STAT This is an Open Access article distributed under the terms of the Creative Commons proteins are promising targets for cancer therapy in humans. The data supporting this view Attribution Non-Commercial License (https:// are reviewed herein. creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial Keywords: Cytokine; JAK-STAT; Cancer; Kinase inhibitor use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Pacritinib Combined with Sirolimus and Low-Dose Tacrolimus for GVHD
Author Manuscript Published OnlineFirst on March 22, 2021; DOI: 10.1158/1078-0432.CCR-20-4725 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Pidala J et al GVHD prevention with combined JAK2/mTOR inhibition Pacritinib combined with sirolimus and low-dose tacrolimus for GVHD prevention after allogeneic hematopoietic cell transplantation: Preclinical and Phase I trial results Authors: Joseph Pidala1-3, Kelly Walton4, Hany Elmariah1,3, Jongphil Kim5, Asmita Mishra1,3, Nelli Bejanyan1,3, Taiga Nishihori1,3, Farhad Khimani1,3, Lia Perez1,3, Rawan G. Faramand1,3, Marco L. Davila1-3, Michael L. Nieder1,3, Elizabeth M. Sagatys6, Shernan G. Holtan4, Nicholas J. Lawrence7, Harshani R. Lawrence7, Bruce R. Blazar8, Claudio Anasetti1-3, Said M. Sebti9, Brian C. Betts4* Affiliations: 1Department of Blood and Marrow Transplantation – Cellular Immunotherapy, Moffitt Cancer Center, Tampa, FL, USA, 2Department of Immunology, Moffitt Cancer Center, Tampa, FL, USA, 3Department of Oncologic Sciences, University of South Florida, Tampa, FL, USA, 4Division of Hematology, Oncology, and Transplantation, Department of Medicine, Masonic Cancer Center, University of Minnesota, Minneapolis, MN, USA, 5Department of Biostatistics and Bioinformatics, Moffitt Cancer Center, Tampa, FL, USA, 6Department of Hematopathology and Laboratory Medicine, Moffitt Cancer Center, Tampa, FL, USA, 7Department of Drug Discovery, Moffitt Cancer Center, Tampa, FL, USA, 8Division of Blood and Marrow Transplantation, Department of Pediatrics, Masonic Cancer Center, University of Minnesota, Minneapolis, Minnesota, USA, 9Department of Pharmacology and Toxicology, Virginia Commonwealth University, Richmond, Virginia USA. Running Title: GVHD prevention with combined JAK2/mTOR inhibition *Address correspondence to: Brian C. Betts, MD Division of Hematology, Oncology, and Transplantation, Department of Medicine, University of Minnesota Nils Hasselmo Hall, Room 2-108, 312 Church Street SE Minneapolis, MN 55455 [email protected] COI statement: B.C.B. -

Comparison of Janus Kinase Inhibitors to Block the Type I Interferon Pathway in Human
bioRxiv preprint doi: https://doi.org/10.1101/2021.02.08.430317; this version posted February 8, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Title: Comparison of Janus kinase inhibitors to block the type I interferon pathway in human skeletal muscle cells Authors: Travis B. Kinder1* and James Inglese1,2 1National Center for Advancing Translational Sciences, National Institutes of Health, Rockville, MD, USA, 2National Human Genome Research Institute, National Institutes of Health, Bethesda, MD, USA *corresponding author: Travis B. Kinder, PhD Post-Doctoral Research Fellow, Assay Development and Screening Technology, National Center for Advancing Translational Sciences, National Institutes of Health, 9800 Medical Center Drive, Rockville, MD, 20850 [email protected] Funding: This work was supported by a grant from the Cure Juvenile Myositis Foundation and the intramural program of NCATS, NIH, project 1ZIATR000342 (J.I.). Competing interests: None ORCID iD: Travis Kinder: 0000-0003-4161-8213 and James Inglese: 0000-0002-7332-5717 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.02.08.430317; this version posted February 8, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Abstract The family of Janus kinases (JAK1, JAK2, JAK3, TYK2) mediate signal transduction from cytokine receptors by phosphorylation and activation of intracellular signaling pathways and transcription factors. -

Annexes to the Annual Report of the European Medicines Agency 2014
Annexes to the annual report of the European Medicines Agency 2014 Table of contents Annex 1 – Members of the Management Board ............................................................................. 2 Annex 2 – Members of the Committee for Medicinal Products for Human Use ................................... 4 Annex 3 – Members of the Pharmacovigilance Risk Assessment Committee ...................................... 6 Annex 4 – Members of the Committee for Medicinal Products for Veterinary Use ............................... 8 Annex 5 – Members of the Committee on Orphan Medicinal Products ............................................ 10 Annex 6 – Members of the Committee on Herbal Medicinal Products .............................................. 12 Annex 07 – Committee for Advanced Therapies .......................................................................... 14 Annex 8 – Members of the Paediatric Committee ........................................................................ 16 Annex 9 – Working parties and working groups .......................................................................... 18 Annex 10 – CHMP opinions in 2014 on medicinal products for human use ...................................... 22 Annex 11 – CVMP opinions in 2014 on medicinal products for veterinary use .................................. 36 Annex 12 – COMP opinions in 2014 on designation of orphan medicinal products ............................ 41 Annex 13 – HMPC European Union herbal monographs in 2014.................................................... -

Medical Product Quality Report – COVID-19 Issues
Medical Product Quality Report – COVID-19 Issues Issue 8. January 2021 The document has been produced by the Medicine Quality Research Group, Centre of Tropical Medicine & Global Health, Nuffield Department of Medicine, University of Oxford This report was prepared by Kerlijn Van Assche, Céline Caillet and Paul Newton of the Medicine Quality Research Group, that is part of the MORU Tropical Health Network and Infectious Diseases Data Observatory (IDDO), Centre for Tropical Medicine & Global Health, Nuffield Department of Medicine, University of Oxford, UK. The Globe system was developed by Clark Freifeld (HealthMap, Boston Children’s Hospital, North Eastern University) and Andrew Payne (IDDO), Alberto Olliaro (IDDO) and Gareth Blower (ex-IDDO) with curation of the English reports by Konnie Bellingham, Kitignavong Inthaphavanh and Vayouly Vidhamaly, linked to the Lao- Oxford-Mahosot Hospital-Wellcome Trust Research Unit (LOMWRU), Microbiology Laboratory, Mahosot Hospital, Vientiane, Lao PDR. This document is open access but we would be grateful if you could cite it as: Medicine Quality Research Group, University of Oxford. Medical Product Quality Report – COVID-19 Issues. Issue 8, January 2021. The work is kindly supported by the Bill&Melinda Gates Foundation, the University of Oxford and the Wellcome Trust. March 3th, 2021 2 Contents 1. Summary of findings ........................................................................................... 4 2. Introduction ........................................................................................................ -

Supplementary Materials
1 Supplementary Materials Figure S1. Flowchart of the Material and Methods: PRISMA flow diagram of the study. RCT, randomized controlled trial. 2 Table S1. Search strategies modified in MEDLINE (a), Embase (b), Cochrane CENTRAL (c), and Web of Science (d) a. Search strategy in MEDLINE (via Ovid MEDLINE(R), 1946–present; search date: 2021/01/29) # Search syntax Citations found 1 ("atopic dermatitis" OR eczema*).mp 2 exp "Dermatitis, Atopic"/ OR exp "Eczema"/ 3 ((Janus ADJ3 kinase* ADJ3 inhibit*) OR (JAK* ADJ3 inhibit*) OR Abrocitinib OR "PF-04965842" OR Baricitinib OR LY3009104 OR Olumiant OR INCB028050 OR Delgocitinib OR "JTE-052" OR Gusacitinib OR ASN002 OR Ruxolitinib OR INCB018424 OR INCA24 OR Tofacitinib OR Tasocitinib OR "Tofacitinib citrate" OR Xeljanz OR CP690550 OR Upadacitinib OR "ABT-494" OR RINVOQ OR Cerdulatinib OR "RVT-502" OR PRT062070 OR Peficitinib OR ASP015K OR Filgotinib OR GLPG0634 OR Solcitinib OR "1206163-45-2" OR GLPG0778 OR GSK2586184 OR SHR0302 OR "ATI-502" OR "ATI 50002" OR "A 301" OR "PF- 06700841" OR "RVT-501" OR Decernotinib OR "VX-509" OR Pacritinib OR SB1518 OR Oclacitinib OR Apoquel OR "PF-03394197" OR Fedratinib OR TG101348 OR SAR302503 OR "Fedratinib hydrochloride" OR Inrebic).mp 4 exp "Janus Kinase Inhibitors"/ 5 (1 OR 2) AND (3 OR 4) 195 b. Search strategy in Embase (via Ovid, 1974–present; search date: 2021/01/29) # Search syntax Citations found 1 ("atopic dermatitis" OR eczema*).mp 2 exp "atopic dermatitis"/ OR exp "eczema"/ 3 ((Janus ADJ3 kinase* ADJ3 inhibit*) OR (JAK* ADJ3 inhibit*) OR Abrocitinib -
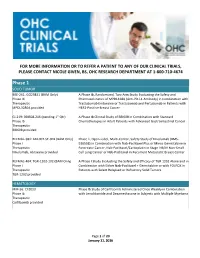
OHC Clinical Trials List V4
FOR MORE INFORMATION OR TO REFER A PATIENT TO ANY OF OUR CLINICAL TRIALS, PLEASE CONTACT NICOLE GIVEN, BS, OHC RESEARCH DEPARTMENT AT 1-800-710-4674 Phase 1 SOLID TUMOR BRE-261: GO29831 (BAM Only) A Phase Ib, Randomized, Two-Arm Study Evaluating the Safety and Phase Ib Pharmacokinetics of MPDL328A (Anti-PD-L1 Antibody) in Combination with Therapeutic Trastuzumab Emtansine or Trastuzumab and Pertuzumab in Patients with MPDL3280A provided HER2-Positive Breast Cancer GI-219: BBI608-246 (pending 1st Qtr) A Phase Ib Clinical Study of BBI608 in Combination with Standard Phase Ib Chemotherapies in Adult Patients with Advanced Gastrointestinal Cancer Therapeutic BBI608 provided REFMAL-381: ABI-007-ST-001 (BAM Only) Phase 1, Open-Label, Multi-Center, Safety Study of Nivolumab (BMS- Phase I 936558) in Combination with Nab-Paclitaxel Plus or Minus Gemcitabine in Therapeutic Pancreatic Cancer, Nab-Paclitaxel/Carboplatin in Stage IIIB/IV Non-Small Nivolumab, Abraxane provided Cell Lung Cancer or Nab-Paclitaxel in Recurrent Metastatic Breast Cancer REFMAL-404: TGR-1202-102 (BAM Only) A Phase I Study Evaluating the Safety and Efficacy of TGR 1202 Alone and in Phase I Combination with Either Nab-Paclitaxel + Gemcitabine or with FOLFOX in Therapeutic Patients with Select Relapsed or Refractory Solid Tumors TGR-1202 provided HEMATOLOGY MM-56: CFZ013 Phase Ib Study of Carfilzomib Administered Once Weekly in Combination Phase Ib with Lenalidomide and Dexamethasone in Subjects with Multiple Myeloma Therapeutic Carfilzomib provided Page 1 of 20 January 11, -

Overview of Planned Or Ongoing Studies of Drugs for the Treatment of COVID-19
Version of 16.06.2020 Overview of planned or ongoing studies of drugs for the treatment of COVID-19 Table of contents Antiviral drugs ............................................................................................................................................................. 4 Remdesivir ......................................................................................................................................................... 4 Lopinavir + Ritonavir (Kaletra) ........................................................................................................................... 7 Favipiravir (Avigan) .......................................................................................................................................... 14 Darunavir + cobicistat or ritonavir ................................................................................................................... 18 Umifenovir (Arbidol) ........................................................................................................................................ 19 Other antiviral drugs ........................................................................................................................................ 20 Antineoplastic and immunomodulating agents ....................................................................................................... 24 Convalescent Plasma ........................................................................................................................................... -

State-Of-The-Art Solutions for Myelofibrosis the Intersection of JAK Inhibitors, Allogeneic Transplant, and Other Strategies for Patient Care
State-of-the-Art Solutions for Myelofibrosis The Intersection of JAK Inhibitors, Allogeneic Transplant, and Other Strategies for Patient Care This session is open only to registrants of the 2020 Transplantation and Cellular Therapy (TCT) Meetings of ASTCT and CIBMTR in Orlando, FL. Disclosures Prithviraj Bose, MD, has a financial Jeanne M. Palmer, MD, has a financial interest/relationship or affiliation in the form of: interest/relationship or affiliation in the form of: Consultant and/or Advisor for Celgene Consultant and/or Advisor for CTI BioPharma Corporation; CTI BioPharma Corp.; Incyte Corp. Corporation; and Kartos Therapeutics, Inc. Grant/Research Support from Astellas Pharma US, Inc.; Blueprint Medicines Corporation; Celgene Corporation; CTI BioPharma Corp.; Incyte Corporation; Kartos Therapeutics, Inc.; NS Pharma,Inc.; Pfizer, Inc.; Promedior, Inc. and Constellation Pharmaceuticals. This CME activity is jointly provided by The Medical College of Wisconsin and PVI, PeerView Institute for Medical Education. This activity is supported by an educational grant from Celgene Corporation. Visit us at PeerView.com/MF2020 • Watch for the onDemand version in the coming weeks • Download the slides and Practice Aids • Apply for CME credit Join the conversation on Twitter @PeerView Need more information? Send an email to [email protected] Welcome, Introduction, and Baseline Assessment Jeanne M. Palmer, MD Associate Professor, Division of Hematology and Oncology Photo Pending Vice Chair and Section Lead, Division of Hematology Program Director,