Student Handbook 2021-2022
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tattler for Pdf 11/1
Volume XXIX • Number 5 • January 31, 2003 Grand Rapids Fall Book. Clear Channel’s Country WBCT is on top once again! WBCT 9.9-9.6, WSNX 8.1-6.8, WLAV 7.3-6.4, WOOD-FM THETHE 4.9-5.7, WOOD-AM 5.1-5.5, WLHT 4.6-5.2, WGRD 6.4-5.0, WKLQ 5.8- 4.7, WTRV 3.7-4.2, WBFX 3.8-4.0, WODJ 3.9-3.6, WJQK 2.5-2.8, WVTI MAIN STREET 2.8-2.3, WFGR 1.6-2.2, WBBL-AM 1.7-2.1, WMUS 1.5-1.8, WFUR 1.3- CommunicatorNetwork 1.7, WMJH-AM 1.6-1.3, WJNZ-AM 1.1-1.0, WTKG-AM 1.1-1.0, WHTC- AM 0.5-0.7, WGHN 0.5-0.7, WKWM-AM 0.5-0.6, WYGR-AM 1.2-0.6, A T T L E WYVN 0.4-0.5, WMRR 0.8-0.5. Fall books found in this TATTLER are TT A T T L E RR 12+ persons, 6A-12P, M-Su, 6A-mid, Summer 2002 – Fall 2002 com- parisons, unless otherwise noted. Copyright © 2002, The Arbitron Com- TheThe intersectionintersection ofof radioradio && musicmusic sincesince 19741974 pany. These results may not be used without permission from Arbitron. TomTom KayKay -- ChrisChris MozenaMozena -- BradBrad SavageSavage The Conclave gives the 2 minute warning!! Make that, the 2 week Congrats to former Conclave Board member – and longtime Conclave warning. The Conclave wants EVERYONE to know it is STILL accepting agenda committee head – Rob Sisco as he ascends to the post of Presi- applications from high school students throughout the Upper Midwest dent, Nielsen Music and COO, Nielsen Retail Entertainment Infor- and Great Lakes region interested in studying for a career in the radio or mation (REI). -

BASKETBALL GIRLS BASKETBALL FOOTBALL BOYS SOCCER Sep 8
FREE HIGH SCHOOL • COLLEGE • NFL CONTENTS Welcome Page .............................................2 Tribute to Rick “Poncho” Lambert ................26 Henderson County Sports ..........................4-5 Henderson County Officials .........................29 Henderson County Hall of Fame .................6-7 Webster County Officials.............................29 Union County Sports ..................................8-9 Union County Officials ................................29 Union County Hall of Fame ..........................10 University of Kentucky ..........................30, 32 Webster County Sports ..........................12-13 University of Louisville ................................34 Boonville ...................................................14 Western Kentucky ......................................34 Evansville Bosse ........................................14 Notre Dame ...............................................34 Castle .......................................................15 WSON/WMSK/WUCO/ESPN Radio Guide .....36 Evansville Central .......................................15 Cincinnati Reds ..........................................38 Gibson Southern ........................................16 St. Louis Cardinals .....................................39 Evansville Harrison .....................................16 SEC Eastern Division ..................................40 Evansville Mater Dei ...................................17 SEC Western Division .................................41 Evansville Memorial ....................................17 -

Whit Adamson President Tennessee
Whit Adamson running, Don brings together hundreds of the top President personalities from throughout the US and Tennessee Association of Broadcasters abroad for his highly acclaimed Morning Show Nashville, TN Boot Camp. It has become radio’s largest Whit Adamson is gathering of its type. President of the Tennessee Association of Following the success Broadcasters, Nashville, of Morning Show Boot Tennessee. Mr. Camp, he began Talk Adamson holds a B.S. Radio Boot Camp, now degree in Economics and in its 7th year. Talk Finance from MTSU Radio Boot Camp was (1971). During his immediately successful. Don brings in the fourteen year career with leading Talk Radio talent in America, as well as the Nashville NBC Affiliate, WSM-TV/WSMV-TV, internationally. he earned the President's Trophy from the Through his conference, his monthly publication Nashville Advertising Federation, was the Silver for talent, and his daily talent search operation, Medal recipient in 1992 and holds the titles of Don has developed a unique and well-honed Past Vice President and Committee Chairman, insight into the inter-workings and elements of as well as a position on the Board of Directors. successful radio shows. As President of the Tennessee Association of Jockline is a daily newsletter for air talent and Broadcasters, he is a lobbyist for tele- the radio industry, and one you can read daily at communications and advertising issues to the www.themorningmouth.com. United States Congress, State General Assembly, and Federal Communications Commission. Alan Austin Grand Pooba of Creative Mr. Adamson is the founding member and Production incorporator of the Tennessee Association of WBVR/WUHU/WLYE/WBGN Communications. -
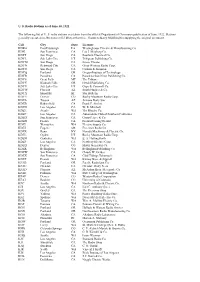
U. S. Radio Stations As of June 30, 1922 the Following List of U. S. Radio
U. S. Radio Stations as of June 30, 1922 The following list of U. S. radio stations was taken from the official Department of Commerce publication of June, 1922. Stations generally operated on 360 meters (833 kHz) at this time. Thanks to Barry Mishkind for supplying the original document. Call City State Licensee KDKA East Pittsburgh PA Westinghouse Electric & Manufacturing Co. KDN San Francisco CA Leo J. Meyberg Co. KDPT San Diego CA Southern Electrical Co. KDYL Salt Lake City UT Telegram Publishing Co. KDYM San Diego CA Savoy Theater KDYN Redwood City CA Great Western Radio Corp. KDYO San Diego CA Carlson & Simpson KDYQ Portland OR Oregon Institute of Technology KDYR Pasadena CA Pasadena Star-News Publishing Co. KDYS Great Falls MT The Tribune KDYU Klamath Falls OR Herald Publishing Co. KDYV Salt Lake City UT Cope & Cornwell Co. KDYW Phoenix AZ Smith Hughes & Co. KDYX Honolulu HI Star Bulletin KDYY Denver CO Rocky Mountain Radio Corp. KDZA Tucson AZ Arizona Daily Star KDZB Bakersfield CA Frank E. Siefert KDZD Los Angeles CA W. R. Mitchell KDZE Seattle WA The Rhodes Co. KDZF Los Angeles CA Automobile Club of Southern California KDZG San Francisco CA Cyrus Peirce & Co. KDZH Fresno CA Fresno Evening Herald KDZI Wenatchee WA Electric Supply Co. KDZJ Eugene OR Excelsior Radio Co. KDZK Reno NV Nevada Machinery & Electric Co. KDZL Ogden UT Rocky Mountain Radio Corp. KDZM Centralia WA E. A. Hollingworth KDZP Los Angeles CA Newbery Electric Corp. KDZQ Denver CO Motor Generator Co. KDZR Bellingham WA Bellingham Publishing Co. KDZW San Francisco CA Claude W. -
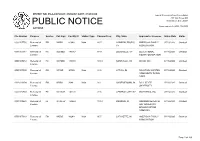
Public Notice >> Licensing and Management System Admin >>
REPORT NO. PN-2-200720-01 | PUBLISH DATE: 07/20/2020 Federal Communications Commission 445 12th Street SW PUBLIC NOTICE Washington, D.C. 20554 News media info. (202) 418-0500 ACTIONS File Number Purpose Service Call Sign Facility ID Station Type Channel/Freq. City, State Applicant or Licensee Status Date Status 0000107750 Renewal of FM WAWI 81646 Main 89.7 LAWRENCEBURG, AMERICAN FAMILY 07/16/2020 Granted License TN ASSOCIATION 0000107387 Renewal of FX W250BD 141367 97.9 LOUISVILLE, KY EDUCATIONAL 07/16/2020 Granted License MEDIA FOUNDATION 0000109653 Renewal of FX W270BK 138380 101.9 NASHVILLE, TN WYCQ, INC. 07/16/2020 Granted License 0000107099 Renewal of FM WFWR 90120 Main 91.5 ATTICA, IN FOUNTAIN WARREN 07/16/2020 Granted License COMMUNITY RADIO CORP 0000110354 Renewal of FM WBSH 3648 Main 91.1 HAGERSTOWN, IN BALL STATE 07/16/2020 Granted License UNIVERSITY 0000110769 Renewal of FX W218CR 141101 91.5 CENTRAL CITY, KY WAY MEDIA, INC. 07/16/2020 Granted License 0000109620 Renewal of FL WJJD-LP 123669 101.3 KOKOMO, IN KOKOMO SEVENTH- 07/16/2020 Granted License DAY ADVENTIST BROADCASTING COMPANY 0000107683 Renewal of FM WQSG 89248 Main 90.7 LAFAYETTE, IN AMERICAN FAMILY 07/16/2020 Granted License ASSOCIATION Page 1 of 169 REPORT NO. PN-2-200720-01 | PUBLISH DATE: 07/20/2020 Federal Communications Commission 445 12th Street SW PUBLIC NOTICE Washington, D.C. 20554 News media info. (202) 418-0500 ACTIONS File Number Purpose Service Call Sign Facility ID Station Type Channel/Freq. City, State Applicant or Licensee Status Date Status 0000108212 Renewal of AM WNQM 73349 Main 1300.0 NASHVILLE, TN WNQM. -

1. About Us 2. Our Reach Market Share Graph Issue Graph 3
since 2008 2012 Map of Kentucky Media Outlet Pickup* *A full list of outlets that picked up KNC can be found in section 8. “KNC reaches markets our other media efforts often don’t reach...delivers stories to media outlets that often don’t have capacity to produce their own.” - Jerry Hardt, , Kentuckians For The Commonwealth 1. About Us 2. Our Reach Market Share Graph Issue Graph 3. Why Solution-Focused Journalism Matters (More Than Ever) 4. Spanish News and Talk Show Bookings 5. Member Benefits 6. List of Issues 7. PR Needs (SBS) 8. Media Outlet List Kentucky News Connection • kentuckynewsconnection.org page 2 1. About Us What is the Kentucky News Connection? Launched in 2008, the Kentucky News Connection is part of a network of independent public interest state-based news services pioneered by Public News Service. Our mission is an informed and engaged citizenry making educated decisions in service to democracy; and our role is to inform, inspire, excite and sometimes reassure people in a constantly changing environment through reporting spans political, geographic and technical divides. Especially valuable in this turbulent climate for journalism, currently 147 news outlets in Kentucky and neighboring markets regularly pick up and redistribute our stories. Last year, an average of 16 media outlets used each Kentucky News Connection story. These include outlets like the Associated Press KY Bureau, WQMF-FM Clear Channel News talk Louisville, WLAP-AM Clear Channel News talk Lexington, WBTF-FM Clear Channel News talk Lexington, WHAS-AM Clear Channel News talk Louisville, Appalachian News Express, Aldia en America and WAMZ-FM Louisville. -
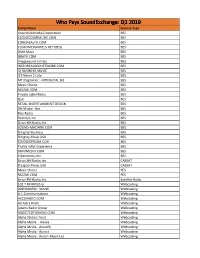
Licensee Count Q1 2019.Xlsx
Who Pays SoundExchange: Q1 2019 Entity Name License Type Aura Multimedia Corporation BES CLOUDCOVERMUSIC.COM BES COROHEALTH.COM BES CUSTOMCHANNELS.NET (BES) BES DMX Music BES GRAYV.COM BES Imagesound Limited BES INSTOREAUDIONETWORK.COM BES IO BUSINESS MUSIC BES It'S Never 2 Late BES MTI Digital Inc - MTIDIGITAL.BIZ BES Music Choice BES MUZAK.COM BES Private Label Radio BES Qsic BES RETAIL ENTERTAINMENT DESIGN BES Rfc Media - Bes BES Rise Radio BES Rockbot, Inc. BES Sirius XM Radio, Inc BES SOUND-MACHINE.COM BES Stingray Business BES Stingray Music USA BES STUDIOSTREAM.COM BES Thales Inflyt Experience BES UMIXMEDIA.COM BES Vibenomics, Inc. BES Sirius XM Radio, Inc CABSAT Stingray Music USA CABSAT Music Choice PES MUZAK.COM PES Sirius XM Radio, Inc Satellite Radio 102.7 FM KPGZ-lp Webcasting 999HANKFM - WANK Webcasting A-1 Communications Webcasting ACCURADIO.COM Webcasting Ad Astra Radio Webcasting Adams Radio Group Webcasting ADDICTEDTORADIO.COM Webcasting Aloha Station Trust Webcasting Alpha Media - Alaska Webcasting Alpha Media - Amarillo Webcasting Alpha Media - Aurora Webcasting Alpha Media - Austin-Albert Lea Webcasting Alpha Media - Bakersfield Webcasting Alpha Media - Biloxi - Gulfport, MS Webcasting Alpha Media - Brookings Webcasting Alpha Media - Cameron - Bethany Webcasting Alpha Media - Canton Webcasting Alpha Media - Columbia, SC Webcasting Alpha Media - Columbus Webcasting Alpha Media - Dayton, Oh Webcasting Alpha Media - East Texas Webcasting Alpha Media - Fairfield Webcasting Alpha Media - Far East Bay Webcasting Alpha Media -

Titans Host Browns to Open December Schedule
FOR IMMEDIATE RELEASE NOVEMBER 30, 2020 TITANS HOST BROWNS TO OPEN DECEMBER SCHEDULE Tennessee Titans (8-3) vs. Cleveland Browns (8-3) Sunday, Dec. 6, 2020 • Noon CST • Nissan Stadium • Nashville, Tenn. • TV: CBS NASHVILLE — The Tennessee Titans return home this week to face the Cleveland Browns in a battle of AFC playoff hopefuls with identical 8-3 records. Kickoff at Nissan Stadium is scheduled for noon CST on Sunday, Dec. 6. Ticket sales for the contest were limited to 21 percent of the Nissan Stadium's normal capacity following current Center for Disease Control guidelines. Detailed information on 2020 TITANS SCHEDULE the team’s Safe Stadium Plan can be found at tennesseetitans.com/safestadium. Result, Score, THE BROADCAST Day Date Opponent Kickoff TV This week’s contest will be regionally televised on CBS, including Nashville affiliate Mon. Sept. 14 at Denver W 16-14 WTVF NewsChannel 5. The broadcast team includes play-by-play announcer Ian Eagle, analyst Charles Davis and reporter Evan Washburn. Sun. Sept. 20 JACKSONVILLE W 33-30 Fans can livestream the broadcast on their mobile devices from the Titans Sun. Sept. 27 at Minnesota W 31-30 Mobile App (iOS and Android) and on TennesseeTitans.com mobile web. Restrictions Sun. Oct. 4 Bye apply. For more information and additional options visit TennesseeTitans.com or NFL.com/ways-to-watch. Tue. Oct. 13 BUFFALO W 42-16 The Titans Radio Network, including Nashville flagship 104.5 The Zone, will carry Sun. Oct. 18 HOUSTON W 42-36 (OT) the game across the Mid-South with the “Voice of the Titans” Mike Keith, analyst Dave Sun. -

AM and FM Report
GeoPlanner™ AM and FM Radio Report Posey Solar Prepared on Behalf of Posey Solar LLC March 15, 2021 Posey Solar LLC Solar Power GeoPlanner™ AM and FM Radio Report Posey Solar Table of Contents 1. Introduction - 1 - 2. Summary of Results - 1 - 3. Impact Assessment - 5 - 4. Recommendations - 6 - 5. Contact - 6 - Comsearch Proprietary - 0 - March 15, 2021 Posey Solar LLC Solar Power GeoPlanner™ AM and FM Radio Report Posey Solar 1. Introduction Posey Solar LLC is proposing to construct and place in utility service the Posey Solar Project, an electric generation facility located in Posey County, Indiana. The facility will generate electricity using silicon photovoltaic (PV) modules fixed to single axis solar trackers. It will have an installed capacity of up to 300 MW ac (380 MW dc). Comsearch analyzed AM and FM radio broadcast stations whose service could potentially be affected by the Posey Solar Project. 2. Summary of Results AM Radio Analysis Comsearch found fifteen database records1 for AM stations within approximately 30 kilometers of the project area (AOI) for the solar farm, as shown in Table 1 and Figure 1. The closest station to the AOI is WSWI, licensed in Evansville, Indiana, and located 6.37 km to the east of the AOI. Transmit Frequency Operation Latitude Longitude Distance to ID Call Sign Status2 ERP3 (kHz) Time (NAD 83) (NAD 83) AOI (km) (kW) 1 WSWI LIC 820 0.25 Daytime 37.964764 -87.668352 6.37 2 WRCY LIC 1590 0.5 Daytime 37.934211 -87.928361 9.92 3 WRCY LIC 1590 0.035 Nighttime 37.934211 -87.928361 9.92 4 WEOA LIC 1400 1.0 -

Services That Have Paid Soundexchange Through Q3 2015 Payments Received Through 10/19/2015
Services that have paid SoundExchange through Q3 2015 payments received through 10/19/2015 License Type Service Name Webcasting 100HITZ.COM Webcasting 181.FM Webcasting 3ABNRADIO.ORG Webcasting 8TRACKS.COM Webcasting ABERCROMBIE.COM Webcasting ACAVILLE.COM Webcasting ACCESS.1 COMMUNICATION CORP. SHREVEPORT Webcasting ADAMS RADIO GROUP Webcasting ADDICTEDTORADIO.COM Webcasting AGM SANTA MARIA, L.P. Webcasting AIR1.COM Webcasting AIR1.COM (CHRISTMAS) Webcasting AJG CORPORATION Webcasting ALANSGOLDENOLDIES.COM Webcasting ALL MY PRAISE Webcasting ALLEGHENYMOUNTAINRADIO.ORG *SoundExchange accepts and distributes payments without confirming eligibility or compliance under Sections 112 or 114 of the Copyright Act, and it does not waive the rights of artists or copyright owners that receive such payments. Services that have paid SoundExchange through Q3 2015 payments received through 10/19/2015 Webcasting ALLNEWCOUNTRY.COM - Webcasting ALLWORSHIP.COM Webcasting ALLWORSHIP.COM (CONTEMPORARY) Webcasting ALLWORSHIP.COM (INSTRUMENTAL) Webcasting ALLWORSHIP.COM (SPANISH) Webcasting ALOHA STATION TRUST Webcasting ALPHA MEDIA, LLC - BILOXI, MS Webcasting ALPHA MEDIA, LLC - DAYTON, OH Webcasting ALPHA MEDIA, LLC - HAGERSTOWN, PA Webcasting ALPHA MEDIA, LLC - SAN ANTONIO, TX Business Establishment Service AMBIANCERADIO.COM Webcasting AMERICOM BROADCASTING Webcasting AMI RADIO STREAMING Webcasting ANCIENTFAITHRADIO.COM Webcasting ANGELO.EDU/SERVICES/RAMRADIO Webcasting ANGLICANRADIO.COM Webcasting APEX BROADCASTING, INC. *SoundExchange accepts and distributes -

2009 Outreach Contact List
Adair Chamber of Commerce Glasgow Regional Educational Adair County Adult Education Department of Parks and Recreation Opportunity Center Adair County Board of Education Emma B. Ward Elementary Glasgow Regional Medical Assistance Adair County Fair Robert B. Turner Elementary School Housing Authority of Glasgow Adair County High School Kentucky Transitional Assistance Adair County Middle School Ballard Program Adair County Public Library Advance Yeoman The Progress Lindsey Wilson College Ballard County Adult Education WCLU Radio - Admissions Center - Financial Aid Ballard County Board of Education Bath WAIN Radio Ballard County Chamber of Bath County Adult Learning Center WAVE Radio Commerce Bath County Cooperative Extension Ballard County Elementary School Service Allen Ballard County Family Resource / Bath County Head Start Allen County Adult Education Center Youth Service Center Bath County High School Allen County Community Action Ballard County Fair Bath County Memorial Library Agency Ballard County Fair Board Bath County Middle School Allen County Community Center Ballard County Health Department Cabinet for Health and Family Allen County Cooperative Extension Ballard County Middle School Services Service Ballard County Weekly - Family Support Allen County Detention Center Ballard Memorial High School - Protection and Permanency Allen County Health Department WBCE Radio Christian Social Services Allen County Primary Center WBEL Radio Commonwealth Educational Allen County Public Library WCBL Radio Opportunity Center - Teen Reading -

OR\G\~~ F\\..~ /.~ RECEIVED Before the "Bddal COIDIVIIICATI0II8 COIIMI88IOII JUN 12 1992 Washinqton, D.C
OR\G\~~ f\\..~ /.~ RECEIVED Before the "BDDaL COIDIVIIICATI0II8 COIIMI88IOII JUN 12 1992 Washinqton, D.C. 20554 FEDERAL COMMUNICATIONS COMMISSIOO OFFICE OF TIlE SECRETAAY 1 In the Matter of ) MM Docket No. 92-39 ) DO'l'DII Uoa.DCUTI.G CO., Ille. ) ) Licensee of station WAGF(AM) ) Dothan, Alabama ) ) Order to Show Cause Why the ) License for station WAGF(AM) ) Dothan, Alabama, ) Should Not be Revoked ) To: Mass Media Bureau Dothan Broadcasting Co., Inc. (hereafter DBC), by its attorneys and pursuant to the Statgent of Policy on Minority ownership of Broadcasting Facilities, 68 FCC2d 979, 42.RR2d 1689 (1978), hereby requests the Mass Media Bureau to authorize the assignaent of the license of standard broadcast Station WAGF, Dothan, Alabama, to Ja..s R. Wilson, III (hereafter Wilson). The purcha.e price ($60,000) i. within 75 percent of the fair market value of WAGF and Wilson is a member of a qualified minority group within the ..aning of the co_ission's distress sale policy. SiD.L. ~, 85 FCC2d 991, 49 RR2d 986 (1981). In support thereof, DBC respectfully states as follows: 1. DBC is the licensee of standard broadcast station WAGF, which is authorized to operate on 1320 kHz with power of 1 KW (DA N) • DBC operated WAGF for about 8 years and in December 1984 No. of C:-:ples rec'd Ust;\ 8 C0 E - 2 - a••igned the licen.. to J-Frank Enterpri..., Inc. (hereatter J Frank). J-Frank and it. principal, Lewi. Frank Johnson, defaulted on proai.sory Hotes to DBC in the principal sua ot $330,000, and in consequence DBC reacquired the WAGF license (and assets) in late 1989 (BAL-890523EB).